Approach
In adults, snoring is often a multifactorial condition with a variety of causal factors; hence, there will never be one single universal cure. It is important to rule out obstructive sleep apnea (OSA) and upper airway resistance syndrome (UARS) in the patient who snores. For these conditions, CPAP is the main form of treatment.
An accurate assessment to identify the causal anatomic site of a patient's snoring is essential to guide treatment. Most patients need to lose weight, stop smoking, and avoid drinking alcohol. Medical treatment of nasal disorders and mandibular advancement splints can also play an important role.
In patients with non-OSA severe snoring who are not overweight, have failed with conservative measures, and have a single, well-defined site of obstruction (usually at palatal level), surgery may be considered. There are a great number of surgical options but, in general, procedures with minimal morbidity, such as nasal surgery, radiofrequency tissue volume reduction (RFTVR) and pillar implants, should be considered before a uvulopalatopharyngoplasty (UPPP), unless the patient has large tonsils. Other surgeries are available, such as injection snoreplasty, uvulopalatal flap, lingual tonsillectomy, punctuate palatal diathermy, and cautery-assisted palatal stiffening.[38][39][40][41][42] Factors such as the patient's clinical features and preferences, along with the surgeon's training and experience, will determine the most appropriate procedure in each individual case.
Children require a different approach to treatment than adults. Allergic rhinitis should be treated and obese children should be encouraged and helped to lose weight. Intranasal corticosteroids may improve snoring in children.[43] Adenotonsillectomy may cure snoring but, for most children, simple snoring without evidence of OSA or UARS is currently believed by most surgeons to be a benign self-limiting phenomenon that requires no treatment other than parental reassurance.[44] However, evidence is emerging that some children with simple snoring in the absence of OSA have cognitive and behavioral sequelae.[45] Even so, not many surgeons would currently recommend surgery in children for simple snoring alone. However, if there are other indications for surgery (e.g., recurrent tonsillitis, or nasal obstruction from adenoidal hypertrophy) then an adenoidectomy, a tonsillectomy, or a combined procedure may be curative.
For more information on obstructive sleep apnea, see the Obstructive sleep apnea in adults and Dyssomnias in children.
General measures
Patients with simple snoring can be reassured that there is no evidence of long-term health risk. For some patients this reassurance will be sufficient, while others will request further treatment.
If the patient's BMI is over 25, then weight loss is very important. Patients should also be advised to avoid alcohol, smoking, and sedatives. If the patient experiences nasal congestion on lying flat, he or she may be advised to sleep with the head elevated to reduce hydrostatic congestion. If snoring is worse when lying on the back, simple measures such as pinning a rolled-up sock to the back of nightwear or wearing a t-shirt with a breast pocket the wrong way round and putting a small object such as a squash ball in the pocket to discourage lying on the back during sleep may be successful. If snoring disturbs the partner only, then ear plugs or earmuffs may help reduce the volume.[46]
There are a multitude of aids available that claim to decrease the sound level of snoring. However, randomized controlled trials have shown no benefit from lubricating throat sprays, nasal dilator strips, and ergonomically shaped pillows.[34][47] Oropharyngeal exercises may have some limited benefit.[48]
Nasal treatments
A reduced nasal cross-sectional area increases nasal resistance to airflow and promotes inspiratory collapse of both the oropharynx and hypopharynx.[49] Clinical reports describe nasal obstruction-induced snoring, but the exact role of the nasal airway in its pathogenesis is unclear.[50][51][52] If patients complain of nasal obstruction as well as snoring, then nasal treatment may improve their snoring.
Studies reporting subjective effects of nasal dilators (available over the counter at most pharmacies) suggest reduction of snoring and improvement of sleep quality, but objective evaluations are lacking or are less convincing, and no particular dilator would seem superior.[53][54][55][56][57][58] In patients with allergic rhinitis treated with an intranasal corticosteroid, sleep disturbances and daytime fatigue tended to improve.[59] In transient snoring associated with an upper respiratory tract infection, nasal decongestants, such as topical oxymetazoline, may be considered for a short period. Surgical correction of a septal deviation, turbinate hypertrophy, and removal of nasal polyps may all help snoring by overcoming nasal obstruction, though this cannot be guaranteed.[23] Options to overcome nasal obstruction due to turbinate hypertrophy include cautery, laser, radiofrequency, reduction, and outfracturing.[60] Improvement in snoring following surgery is far more likely if the BMI is below 28.[61][62]
In children, topical intranasal corticosteroids may have an effect in reducing adenoid size and can improve the symptoms of snoring.[10][43][63]
Mandibular advancement splint (MAS)
This appliance is usually fitted by a dentist or maxillofacial surgeon and is worn in the mouth overnight. It resembles a combined upper and lower gum shield, joined in such a way as to hold the lower jaw forward. This in turn draws the base of the tongue forward, thereby enlarging the oropharyngeal airway. The MAS is therefore primarily for use in patients where snoring is occurring at the tongue base level. The MAS only works effectively in patients who have a sufficient number of teeth anchored into the upper and lower mandibles, so is generally unsuitable for patients with dentures or poor dentition.
One randomized controlled trial of a MAS versus placebo for simple snoring showed subjective improvement in snoring frequency in 76% of patients and in snoring severity in 84% of patients.[64] Another randomized controlled trial showed that a thermoplastic MAS was an effective treatment in 2 out of 3 patients who snored and the sleep and daytime tiredness of partners also improved.[65]
However, one review found that MAS as compared with placebo resulted in a reduction of snoring loudness in only 38% of patients with non-OSA snoring and an improvement of sleep disturbance in 54% of partners.[66]
It is a relatively simple treatment, reversible, cost effective, and a genuine nonsurgical alternative to patients who represent a poor surgical risk. Patients may develop some minor complications of the jaw, with mouth or tooth pain and changes in dental occlusion.
Palatal implants
In an attempt to provide a single-treatment, office-based procedure, palatal implants have been developed. The aim is to place 3 implants near the junction of the hard and soft palate, thereby extending the rigidity of the hard palate into the soft palate. This helps reduce vibration and flutter of the soft palate, thus reducing snoring.[2] There may be an overall improvement in snoring for 88% of patients (including other procedures) and 79% in those treated only with palatal implants.[67] Longer-term results have shown a visual analog scale (VAS) snoring score reduction from 7.1 to 4.8 at 360 days, with 80% of patients and 71% of bed partners being satisfied with the result of this intervention.[68] One meta-analysis study involving patients who snore found that loudness of snoring, as assessed on a VAS scored by bed partners, was reduced by a standardized mean difference of -0.591 (P <0.001) after treatment with palatal implants, which the investigators concluded was a moderate effect on snoring.[69] The procedure is relatively expensive and implant extrusion may occur.
Radiofrequency treatment to the soft palate and tongue base
Radiofrequency is delivered submucosally via a needle placed into the soft palate. This results in an area of scarring and hence stiffening of the soft palate with reduced vibration. In addition there is volumetric tissue reduction.[70] The main advantages of this technique are that it can be carried out as a day case or outpatient procedure under local anesthetic and causes significantly less postoperative pain and other complications than uvulopalatopharyngoplasty (UPPP) or uvulopalatoplasty (UVPP).[71][72][73]
Initial results have been very encouraging with an 82% reduction in the VAS snoring score in those with a BMI below 25. This figure decreased dramatically to only 31% in those with a BMI over 30.[62] Multiple points can be applied and the procedure repeated. The more lesions treated and the more times the procedure is repeated, the better the outcome.[74]
Radiofrequency can also be applied to the tongue base, again under local anesthesia, and has been shown to reduce snoring scores on a VAS scale, but not to the point of patient satisfaction.[75] However, repeat procedures may be necessary before a clinically significant improvement is seen. Complications are reported at a rate of 2% and include ulcers of the tongue base or soft palate, dysphagia, temporary hypoglossal nerve palsy, and an abscess of the tongue base.[76] The four radiofrequency generators available have comparable efficacy and good safety.[77]
Laser- or radiofrequency-assisted uvulopalatoplasty (UVPP)
This procedure can be carried out under local or general anesthetic. It is traditionally performed using a laser. The uvula is vaporized by the laser and troughs created through the soft palate on each side of the uvula base to form a neo-uvula. There are numerous variations of the technique, but the general principle is to stiffen the soft palate and thereby minimize snoring due to palatal flutter.[12]
Short- and long-term results are similar to UPPP, in that there is a significant decline in benefit over time with early success rates of 74% to 79% and long-term success rates of 55%.[78][79] Occasionally excessive scarring and contraction of the velopharyngeal space may lead to worsening in nasal breathing and snoring.[80]
Radiofrequency is a relatively new technique that uses low-temperature radiofrequency energy delivered via a probe. Radiofrequency-assisted uvulopalatoplasty uses the same surgical method as laser-assisted uvula palatoplasty (LAUP) but employs radiofrequency instead and reportedly results in significantly lower postoperative pain and complications while maintaining the advantages of LAUP.[81][82]
Uvulopalatopharyngoplasty (UPPP)
This is a procedure performed under general anesthetic that involves tonsillectomy and excision of the uvula. The tonsillar pillars are then sutured together. The effect of this is to stiffen the soft palate by scarring and to increase the space behind the soft palate to minimize obstruction. Complications include severe postoperative pain, hemorrhage, nasal regurgitation due to excessive palatal resection, dry throat, swallowing problems, and voice changes.[12] Short-term success rates are quoted as ranging from 65% to 100% in well-selected patient groups; however, long-term successes fall dramatically to approximately 45%.[83][84][85] Patients with larger tonsils (size 3 or 4), smaller tongues (size 1 or 2), and a lower BMI tend to have the best results. Patients with a BMI over 40 tend not to benefit.[86][Figure caption and citation for the preceding image starts]: Crowded oropharynx due to tonsils, prominent posterior pillars, and large uvulaFrom the collection of Dr Showkat Mirza; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Uvulopalatopharyngoplasty, with removal of tonsils and uvula and suturing of uvula stump and pillars, thereby creating an enlarged oropharyngeal inletFrom the collection of Dr Showkat Mirza; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Uvulopalatopharyngoplasty, with removal of tonsils and uvula and suturing of uvula stump and pillars, thereby creating an enlarged oropharyngeal inletFrom the collection of Dr Showkat Mirza; used with permission [Citation ends].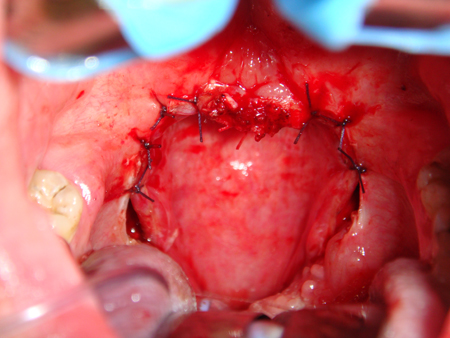
Tonsillectomy and adenoidectomy
For most children with simple snoring without evidence of OSA or UARS, surgery would not normally be considered. However, if there are other indications for surgery (e.g., recurrent tonsillitis, or nasal obstruction from adenoidal hypertrophy), then an adenoidectomy or tonsillectomy or combined procedure may be curative.
For the majority of children with OSA, adenotonsillectomy results in improvement in respiratory parameters measured by polysomnography and quality-of-life measures, although the correlation between the two is poor.[87] Severe OSA preoperatively is associated with persistence of OSA after adenotonsillectomy. Postoperative reports of symptoms such as snoring and witnessed apneas correlate well with persistence of OSA after adenotonsillectomy.[87]
Continuous positive airway pressure (CPAP)
Sleeping with a sealed mask over the face, with applied positive airway pressure, prevents the upper airway from collapsing, thereby stopping airway obstruction and snoring. It is the first-line treatment in adults with UARS or OSA.
CPAP is also effective in children with OSA, but is generally only used when adenotonsillectomy is contraindicated or has failed.[88] CPAP is difficult for approximately 20% of children to tolerate. Since children grow rapidly, frequent follow-up visits are necessary and the mask must be adjusted at least every 6 months.
Use of this content is subject to our disclaimer