History and exam
Key diagnostic factors
common
cough
Occurs in 98% of adult patients and is the most common symptom of bronchiectasis in both adults and children. An acute exacerbation often presents as worsening of cough.
May be associated with large amounts of purulent sputum and, less commonly, hemoptysis.
Cough may be worsened by lying flat or on one side.
sputum production
Daily sputum production is present in two-thirds of adult patients and a wet or productive cough is also common in children. Bloody sputum is present in about 50% of adult patients and is usually mild (i.e., sputum with flecks of blood). Hemoptysis is less common in children and adolescents.
Sputum production will often increase during acute respiratory infections.
An acute exacerbation often presents as a change in sputum color and an increase in sputum volume.
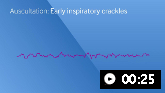
crackles, high-pitched inspiratory squeaks and rhonchi
Many patients will have crackles on pulmonary auscultation. High-pitched inspiratory squeaks and pops are commonly heard.
Auscultation sounds: Early inspiratory crackles
dyspnea
Present in majority of adults patients, especially with exertion.
Often correlates with severity of bronchiectasis on chest CT.
Less common in children and adolescents but if present signifies a severe exacerbation, irrespective of duration.[9]
fever
More than half of patients with bronchiectasis will have recurrent episodes of fever.
An acute exacerbation often presents with fever.
Other diagnostic factors
common
fatigue
A nonspecific but very common symptom. An acute exacerbation often presents with fatigue.
hemoptysis
Present in about 50% of adult patients and is usually mild (i.e., sputum with flecks of blood).
Thought to originate from the bronchial arteries or bronchial-pulmonary anastomoses.
May become massive (>250 mL/day), which warrants hospital admission and immediate referral to a pulmonologist and/or a thoracic surgeon or interventional radiologist for treatment.
Less common in children and adolescents.[9]
rhinosinusitis
Present in about 60% of adult patients.[48] More common in bronchiectasis due to a primary mucociliary clearance defect, such as primary ciliary dyskinesia or cystic fibrosis.
weight loss
A nonspecific sign in adults.
wheezing
Present in one quarter of patients, but more common in bronchiectasis patients who have concomitant asthma.
Less common in children and adolescents.[9]
Auscultation sounds: Expiratory wheeze
Risk factors
strong
cystic fibrosis
Most common identifiable cause of bronchiectasis.
A diagnosis of cystic fibrosis should be considered in younger adults with recurrent sinopulmonary infection and/or bronchiectasis, even in the absence of gastrointestinal symptoms.[3]
Although primarily diagnosed in early childhood, an initial presentation of recurrent sinopulmonary infections in adulthood has become more frequent. Cystic fibrosis patients diagnosed later in life tend to have less pancreatic insufficiency, leading to a reduced likelihood of diabetes and better lung function than patients diagnosed early in life.[26]
Typically presents with sinusitis and bronchiectasis.
Typical colonizing organisms include Pseudomonas aeruginosa or Staphylococcus aureus.
Mutations of the cystic fibrosis transmembrane conductance regulator (CFTR) gene lead to abnormalities of the chloride channels causing viscous mucus and abnormal airway clearance.
host immunodeficiency
Includes immunoglobulin deficiency and HIV infection.
Deficiencies in humoral immunity (either congenital or acquired) associated with decreased levels of IgG (or IgG subclasses), IgM, or IgA are shown to lead to increased risk of sinopulmonary infections and bronchiectasis.[27]
Leads to diffuse disease.
Treatment with intravenous immunoglobulin replacement has been shown to decrease infection rate and the progression of bronchiectasis.[28]
previous infections
Associated with bronchial destruction resulting in bronchiectasis.
Patients with long-standing asthma may develop an exaggerated hyperimmune response to inhaled Aspergillus fumigatus, resulting in chronic airway damage.[29]
Mycobacterium avium-intracellulare complex may colonize the airways of normal hosts, primarily women over 50 years.[30]
Bronchiectasis may occur following viral infections (e.g., measles, influenza, pertussis) or due to prior infections with Mycobacteria tuberculosis or severe bacterial pneumonia.
Swyer-James or Macleod syndrome are forms of lung hypoplasia occurring secondary to childhood infection such as adenovirus.
congenital disorders of the bronchial airways
Patients with Young syndrome exhibit similar features to those of cystic fibrosis patients (including bronchiectasis, sinusitis, and obstructive azoospermia) but without a cystic fibrosis transmembrane conductance regulator (CFTR) genetic mutation or positive sweat chloride test.[31]
Other conditions associated with bronchiectasis include Mounier-Kuhn syndrome (tracheobronchomegaly), Williams-Campbell syndrome (also known as tracheomalacia, characterized by absence or weakness of bronchial cartilage, leading to bronchial collapse), pulmonary sequestration, and yellow nail syndrome.[3]
primary ciliary dyskinesia
An autosomal-recessive disorder with a defect in ciliary structure and/or function.[32] The dysfunctional cilia lead to recurrent ear, sinus, and lung infections.
Kartagener syndrome includes the clinical triad of bronchiectasis, chronic sinusitis, and situs inversus, and occurs in approximately 50% of patients with primary ciliary dyskinesia.[33][34][35]
weak
alpha-1 antitrypsin deficiency
A genetic disorder that predisposes to the development of COPD and, less commonly, bronchiectasis. The estimated prevalence of bronchiectasis in these patients is between 2% and 43%.[36]
connective tissue disease
Bronchiectasis occurs in 1% to 3% of rheumatoid arthritis (RA) patients. Although typically a late finding, one study showed that bronchiectasis preceded the systemic complications of RA in 20% of patients.[37]
Other diseases that may lead to bronchiectasis are Ehlers-Danlos syndrome, Marfan syndrome, and Sjogren syndrome.
inflammatory bowel disease
aspiration or inhalation injury
Blockage and tissue damage increase risk.
focal bronchial obstruction
Includes broncholith, stenosis, tumor, and adenopathy with extrinsic compression.
tall, thin, white females, age 60 or over
Are at greater risk of pulmonary nontuberculous mycobacteria (PNTM)-related bronchiectasis. Mitral valve prolapse, scoliosis, and heterozygous cystic fibrosis transmembrane conductance regulator (CFTR) mutations have been found in greater frequency in these patients.[40]
prematurity
Prematurity is associated with bronchiectasis in children.[41]
Use of this content is subject to our disclaimer