Approach
RVO frequently presents as sudden, painless, unilateral vision loss. Most affected patients are age >65 years.[6] A patient with branch retinal vein occlusion (BRVO) can present with vision loss in 1 quadrant of their visual field, while a patient with central retinal vein occlusion (CRVO) presents with vision loss in the whole visual field. Similarly, a patient with a hemiretinal vein occlusion (HRVO) can present with a vision loss in the whole superior or inferior hemifield of vision, respecting the horizontal meridian.
History
Commonly, older patients have a history of hypertension, diabetes mellitus, atherosclerosis, cardiovascular disease, tobacco use, or glaucoma.[2][6][22] Younger affected patients are more likely to have a history of hypercoagulability or vasculitis.[17][18][19][23]
Commonly, patients with an RVO may present with symptoms of complications from BRVO, CRVO, or HRVO. Vision-threatening complications include macular oedema and neovascularisation. Patients with macular oedema report decreased central vision. Those with a vitreous haemorrhage secondary to retinal neovascularisation complain of floaters throughout their field of vision. A painful, red eye with vision loss could be a presentation of increased intra-ocular pressure in the setting of iris or angle neovascularisation (commonly referred to as neovascular glaucoma).
Patients may have a history of ocular injections, retinal laser treatment, cataract surgery, or refractive surgery.[4][24]
Physical examination
Visual acuity is usually decreased, especially in patients with CRVO, macular oedema, or vitreous haemorrhage. A visual acuity worse than 20/200 is a sign suggesting an ischaemic CRVO.[9][10] A relative afferent pupillary defect would also suggest an ischaemic CRVO.[9][10][25] Intra-ocular pressure should be checked in both eyes to assess the risk of glaucoma, which is a risk factor for RVO, and is elevated in an eye affected by neovascular glaucoma.[22] Confrontational visual field testing can help localise the retinal quadrant(s) affected by the RVO.
Perform slit lamp biomicroscopy with appropriate lenses to evaluate retinopathy (indirect ophthalmoscopy is preferable for examination of the far peripheral retina). During the slit lamp examination, check the iris for neovascularisation and perform gonioscopy to rule out neovascularisation of the angle.
Acutely, dilated fundus examination demonstrates venous tortuosity and dilation, intra-retinal haemorrhages and thickening, and cotton-wool spots in the affected regions of the RVO. A BRVO would have these features in 1 quadrant and in the region of an arteriovenous crossing. An HRVO would have these features in either the superior or inferior retinal hemisphere. In a CRVO, all 4 quadrants of retinal tissue are affected. In addition, CRVO is more likely to feature optic nerve head oedema.
Complications of RVO should be searched for during the dilated fundus examination. The presence or absence of macular thickening should be documented. Although more commonly found in CRVO and HRVO, neovascularisation and/or vitreous haemorrhage may be found in any eye with RVO. Collateral vessel formation, either across the horizontal raphe in the macula (BRVO) or at the optic nerve head (CRVO), is a sign of chronicity.[Figure caption and citation for the preceding image starts]: Colour photograph, right eye; central retinal vein occlusion; multiple intra-retinal haemorrhages in each quadrantFrom the personal library of Dr Aziz Khanifar [Citation ends].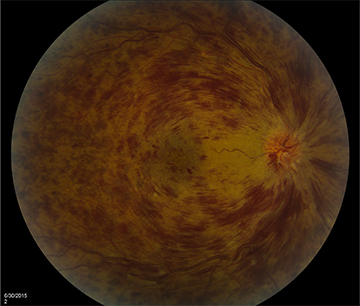 [Figure caption and citation for the preceding image starts]: Optical coherence tomogram, right eye; central retinal vein occlusion; large cystoid thickening throughout maculaFrom the personal library of Dr Aziz Khanifar [Citation ends].
[Figure caption and citation for the preceding image starts]: Optical coherence tomogram, right eye; central retinal vein occlusion; large cystoid thickening throughout maculaFrom the personal library of Dr Aziz Khanifar [Citation ends].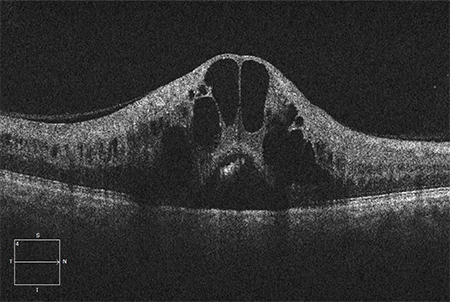
Tests
A fluorescein angiogram should be ordered whenever the diagnosis of RVO is suspected but not confirmed by clinical examination. In addition, fluorescein angiography provides information on complications of RVO, which should be addressed when planning treatment. These complications include retinal ischaemia, macular oedema, and neovascularisation. Presence of macular oedema can be confirmed and quantified using optical coherence tomography (OCT). OCT may reveal intraretinal hyporeflectivity and thickening of the neurosensory retina (evidence of cystoid macular oedema).[4] Sub-retinal hyporeflectivity (evidence of sub-retinal fluid) can be found in eyes with large amounts of macular oedema. In BRVO, macular oedema will be present asymmetrically; for example, for a superior BRVO, only the superior half of the macula will be oedematous. OCT can also be used to evaluate response to therapy for macular oedema. Electroretinography can also confirm the perfusion status of CRVO, especially in the setting of vitreous haemorrhage or significant intra-retinal haemorrhage that prohibits utility of fluorescein angiogram, although it is rarely used in routine clinical practice.[25]
For younger patients with RVO, a thorough history should be taken, exploring the possibilities of either an altered coagulable state or a vasculitis as the underlying aetiology. For young women, this includes determining whether the patient is using oral contraceptives. A limited diagnostic evaluation should then be completed, depending on the patient’s medical history. For altered coagulable states, this would include looking for activated protein C resistance, protein C deficiency, protein S deficiency, antithrombin III deficiency, elevated homocysteine, antiphospholipid antibody syndrome, and factor V Leiden. If appropriate, vasculitic diseases such as systemic lupus erythematosus (SLE) should be ruled out.
[Figure caption and citation for the preceding image starts]: Fluorescein angiogram, right eye; central retinal vein occlusion; delayed drainage of veins in each quadrantFrom the personal library of Dr Aziz Khanifar [Citation ends].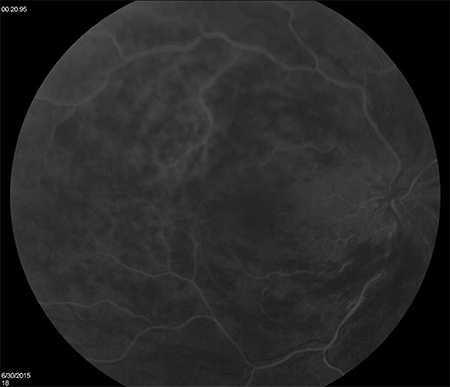 [Figure caption and citation for the preceding image starts]: Colour photograph, left eye; branch retinal vein occlusion; multiple intra-retinal images in quadrant of blocked veinFrom the personal library of Dr Aziz Khanifar [Citation ends].
[Figure caption and citation for the preceding image starts]: Colour photograph, left eye; branch retinal vein occlusion; multiple intra-retinal images in quadrant of blocked veinFrom the personal library of Dr Aziz Khanifar [Citation ends].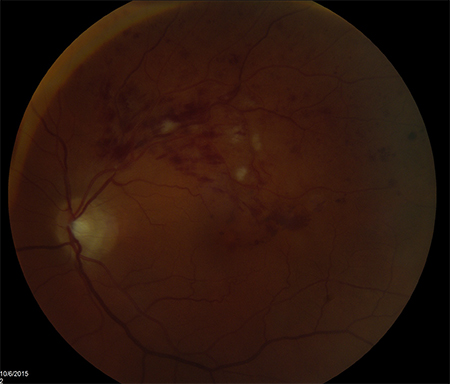 [Figure caption and citation for the preceding image starts]: Fluorescein angiogram, left eye; branch retinal vein occlusion; delayed drainage of blocked vein superotemporallyFrom the personal library of Dr Aziz Khanifar [Citation ends].
[Figure caption and citation for the preceding image starts]: Fluorescein angiogram, left eye; branch retinal vein occlusion; delayed drainage of blocked vein superotemporallyFrom the personal library of Dr Aziz Khanifar [Citation ends].
Use of this content is subject to our disclaimer