Approach
Characteristic clinical appearance combined with laboratory confirmation by potassium hydroxide (KOH) preparation of scale from affected skin demonstrating short hyphae and spores is normally sufficient to diagnose PV.[13]
History
Although PV has been reported in infants, children, and older people, it is most common in adolescents and young adults, when sebaceous gland activity is maximal.[13]
Most patients are asymptomatic. However, pruritus does occur in some cases.[13] The typical complaint is cosmetic disfigurement as a result of pigmentary abnormalities associated with the disease.[29]
Patients commonly relate a relapsing/recurring history of disease, with active flares being most common during summer months and at times of increased temperature and humidity.[13]
The patient history may include a history of hyperhidrosis, family history of the disease, participation in athletics, use of oral contraceptives, use of occlusive ointments or creams, use of systemic corticosteroids, and immunosuppressive disorders including HIV disease. These are risk factors for the disease and should be determined.[7]
Physical examination
PV presents most commonly on the trunk, neck, and upper shoulders: the seborrhoeic areas of the trunk.[13][29]Facial involvement is uncommon but has been described in children in tropical regions.[2][6] Less-common sites of involvement include the scalp, legs, and groin, or within a radiotherapy field.[1]
Lesions are dyschromic, round to oval macules and confluent patches that vary in colour from hypopigmented shades of white to hyperpigmented shades of pink, red, salmon, brown, or, rarely, black.[2] Although most patients present with a single colour change, sometimes 2 colours are present, with areas of hyperpigmentation limited to areas covered by clothes and hypopigmented areas on uncovered skin that is tanned in the normal-pigmented areas.[2] Fine overlying (pityriasiform) scale is common in hyperpigmented lesions of PV but is less common in depigmented lesions.[20] In some instances, if this scale is not evident on initial examination, it can be evoked by either stretching or lightly scraping the affected skin (‘evoked scale’ sign of PV).[31]
Examination of the skin with a Wood light (filtered UV light with a peak of 365 nanometres) can also aid in diagnosing the condition, especially to detect subclinical patches of PV. Lesions of PV may fluoresce a characteristic bright yellow or gold colour under Wood lamp examination in a darkened room. However, Wood lamp examination is positive in only one third of cases, limiting the usefulness of the test.[13] This is most likely due most infections being secondary to non-fluorescent species of Malassezia, as only M furfur seems to produce the indole compounds that fluoresce under Wood light.[2][13][Figure caption and citation for the preceding image starts]: Pityriasis versicolor in a light-skinned personFrom the collection of Brian L. Swick, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Pityriasis versicolor in a dark-skinned personFrom the collection of Brian L. Swick, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Pityriasis versicolor in a dark-skinned personFrom the collection of Brian L. Swick, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Hyperpigmented pityriasis versicolorFrom the collection of Brian L. Swick, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Hyperpigmented pityriasis versicolorFrom the collection of Brian L. Swick, MD [Citation ends].
Investigations
Always confirm a diagnosis of PV by direct microscopical examination of scale from lesions with a KOH preparation. In preparing the specimen, obtain scale and debris from skin lesions by light scraping with a #15 surgical blade or stripping off scale with tape. The specimen is then placed on a glass slide and examined after application of 10% KOH solution with or without Parker ink (which quickly stains the fungi blue) or chlorazol black (which quickly stains the fungi green). If the test is positive, examination should reveal fungal elements with a characteristic spaghetti-and-meatballs appearance indicating the presence of both yeast and short hyphae.[13]
In most cases, a KOH preparation is adequate to diagnose the condition. However, if adequate scale cannot be obtained or if the results are inconclusive, a skin biopsy can be obtained to confirm the diagnosis and exclude other conditions with a similar presentation, especially pityriasis alba, seborrhoeic dermatitis, confluent and reticulate papillomatosis, and vitiligo.
Gram staining may be used as a diagnostic adjunct, with gentian violet applied directly to the affected skin to distinguish PV from other scaly eruptions that can be associated with hyper- or hypopigmented macules and patches.[32]
Fungal culture is not necessary for diagnosis of PV and is difficult for most laboratories to perform, as special media are required.[Figure caption and citation for the preceding image starts]: KOH and chlorazol black preparation showing short hyphae and sporesFrom the collection of Brian L. Swick, MD [Citation ends].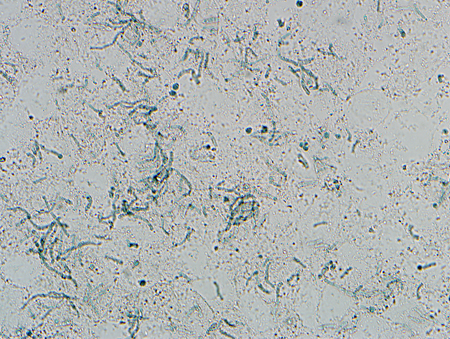
Use of this content is subject to our disclaimer