Approach
A diagnosis of bradycardia is generally made on an ECG or telemetry monitor when there is slowing of the heart rhythm to below 50 bpm, even if only transient. Some consider bradycardia to be a heart rate <60 bpm, but this is in dispute and most consider rates of <50 bpm to represent bradycardia. Bradycardia can also be detected during home blood pressure monitoring using electronic blood pressure monitors, smartphone heart rhythm monitoring applications, and wearable devices that incorporate heart rhythm detection technology. The challenge is determining the aetiology of the bradycardia and determining the site at which there is reduction in either impulse generation or propagation. The primary use of testing is to correlate symptoms with bradycardia and/or to establish a potentially dangerous condition as the cause of bradycardia, even though the patient may be asymptomatic.
History
The most important diagnostic factor is age. Older patients present frequently with bradycardia owing to disease in the sinus node, the atrioventricular (AV) node, or the His-Purkinje system. In the AV conduction system, age-related fibrosis and sclerosis (Lev-Lenegre Syndrome) account for AV block in almost half of the cases. Older patients in particular may also present with bradycardia associated with medicines that have AV-node-blocking properties, such as beta-blockers, calcium-channel blockers, and digoxin; therefore, a detailed drug history should be taken in every patient with bradycardia. Additionally, diuretics may lead to electrolyte disorders, which can cause bradycardia if severe.
History should focus on the timing, severity, frequency, duration, and chronicity of symptoms. Additionally, clinicians should ask about aggravating or alleviating factors, relationship to exercise or exertion, nocturnal symptoms, temporal relationship to medications, postural changes, emotional distress, or manoeuvres that increase vagal tone such as coughing, defecation, vomiting, or wearing tight collars. Clinicians should inquire about daytime sleepiness, memory difficulties, or night-time snoring when thinking about sleep-disordered breathing (SDB) as a potential cause.[11]
A thorough travel history should be obtained to evaluate for any exposures to infections that can lead to bradycardia or myocarditis. For example, Trypanosoma cruzi is a parasite endemic to South and Latin America, and infection can lead to Chagas' disease, which may cause myopericarditis. Additionally, Lyme disease is prevalent in Northeastern US, and can lead to AV nodal conduction delays.
A family or personal history of infiltrative diseases, autoimmune disease, congenital cardiac disease, or cardiovascular disease is also important to ask about.
A complete review of systems should focus on rashes (e.g., erythema migrans in Lyme disease), tick or insect bites, headaches (suggesting increased intracranial pressure), daytime fatigue or snoring evaluating for SDB, exposures to toxins, history of recent or cardiac surgeries/heart transplant, chest pain, or crescendo angina, which may be concerning for myocardial infarction.
Sinus bradycardia is often noted in patients with significant hypothyroidism, whether or not they have other symptoms of the disease. Asymptomatic or symptomatic sinus bradycardia may occur in association with hypothermia.
One of the most common symptoms associated with bradycardia is dizziness or lightheadedness. Many patients also complain of worsening fatigue. Syncope is possible with long pauses or slow heart rates, especially in patients with complete heart block and a slow ventricular escape rhythm with left ventricular dysfunction or in patients with second-degree AV block. These symptoms generally occur owing to bradycardia-induced cerebral hypoperfusion, especially in the setting of left ventricular dysfunction. Exercise intolerance and shortness of breath is also common and may be due to sinus node, AV node, or His-Purkinje system disease. Chest pain is a rare presentation. Bradycardia can be asymptomatic and benign, especially in younger individuals and in trained athletes.
Physical examination
The physical examination is usually non-specific. Palpation of peripheral pulse or cardiac auscultation may reveal a slow, regular heart beat of below 50 bpm or an irregular pulse of varying intensity. Bradycardia by pulse may not necessarily be bradycardia by auscultation or ECG as ventricular bigeminy can present with a slow pulse but not actually represent bradycardia. Occasionally, this and other rhythm disturbances can cause a “pulse deficit” in which a slow pulse mimics a slow heartbeat (i.e., bradycardia).
Patients with bradycardia secondary to complete heart block can have intermittent cannon a-waves in their jugular venous pulse (JVP) owing to atrial contraction against a closed tricuspid valve. Similarly, there may be a variable S1 during complete AV block. During a junctional or ventricular rhythm with 1:1 V-to-A conduction, there may be cannon a-waves.
Because bradycardia can contribute to heart failure, patients may have a third heart sound, rales, jugular venous distension, and abdominal and lower extremity oedema. Signs of hypothyroidism should be assessed (e.g., dry or coarse skin or hair, facial oedema). Poor cardiac output due to bradycardia may be manifest as hypotension, mental status changes, and/or pallor; the extremities may be cool to the touch. Orthostatic vital sign measurements may help diagnose underlying autonomic dysfunction.
ECG
A 12-lead ECG is the first test in the diagnosis of bradycardia, regardless of the suspected cause. It is simple and easy to perform and provides diagnostic information. ECG also offers important clues regarding underlying conditions that could have caused the bradycardia; however, it only gives a snapshot in time that may not be helpful for diagnosis if bradycardia or symptoms are intermittent. In this situation, ambulatory monitoring is needed to correlate symptoms to bradycardia.
Sinus node dysfunction
Sinus bradycardia: regular P-wave followed by QRS at a rate of <50 bpm; ambulatory ECG monitoring is helpful to correlate symptoms with heart rate.[41]
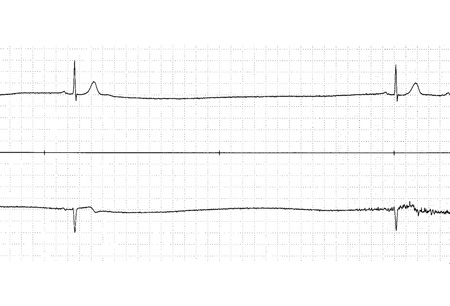
Sinus nodal pauses or arrest: long RR cycle length, which is longer than the RR interval of the underlying sinus rhythm. [Figure caption and citation for the preceding image starts]: ECG showing sinus pauseFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
Sinus nodal exit block: an absent P-wave and prolongation of the RR cycle length, usually twice the underlying sinus RR interval.
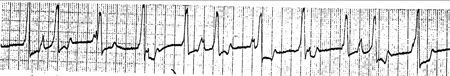
Tachycardia-bradycardia syndrome: episodic periods of tachycardia (usually atrial flutter, atrial fibrillation, or atrial tachycardia), followed by termination of the tachycardia leading to sinus arrest or long sinus pauses, followed by sinus bradycardia.[Figure caption and citation for the preceding image starts]: ECG showing tachy-brady syndromeFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: ECG showing tachy-brady syndromeFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing tachy-brady syndromeFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: ECG showing tachy-brady syndromeFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing tachy-brady syndromeFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].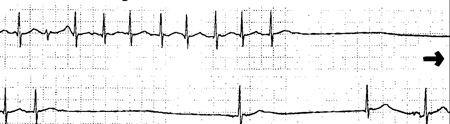 [Figure caption and citation for the preceding image starts]: ECG showing tachy-brady syndromeFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing tachy-brady syndromeFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
AV conduction disturbance
First-degree AV block: fixed prolongation of the PR interval over 0.2 seconds.[13][Figure caption and citation for the preceding image starts]: ECG showing first-degree atrioventricular (AV) blockFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].

Second-degree AV block:
Mobitz I: grouped beating with a constant PP interval, lengthening in the PR interval and changing (usually shortening) RR intervals with the cycle ending with a P-wave not followed by a QRS complex. As the PR interval gradually prolongs, the RR interval tends to stay the same or shorten.[14][Figure caption and citation for the preceding image starts]: ECG showing Mobitz I (Wenckebach) second-degree atrioventricular (AV) blockFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: ECG showing Mobitz I (Wenckebach) second-degree atrioventricular (AV) blockFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing Mobitz I (Wenckebach) second-degree atrioventricular (AV) blockFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: ECG showing Mobitz I (Wenckebach) second-degree atrioventricular (AV) block during acute inferior wall myocardial infarctionFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing Mobitz I (Wenckebach) second-degree atrioventricular (AV) block during acute inferior wall myocardial infarctionFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].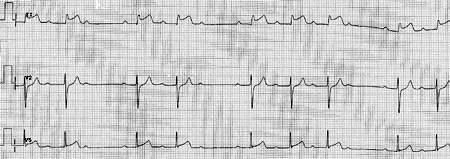
Mobitz II: associated with single non-conducted P-waves with a constant PP interval and constant PR intervals (no change in the PR of over 0.025 seconds).[15][Figure caption and citation for the preceding image starts]: ECG showing Mobitz II second-degree atrioventricular (AV) blockFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: ECG showing Mobitz II second-degree atrioventricular (AV) blockFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing Mobitz II second-degree atrioventricular (AV) blockFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].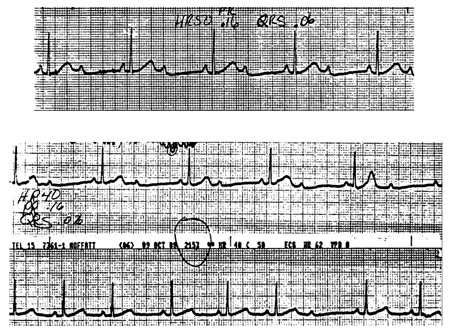
2:1 AV block: only one PR interval to examine before the blocked P-wave and 2 P-waves for every QRS complex. Block can be at the level of the AV node or the His-Purkinje system. If the QRS is narrow, the level of the block is probably in the AV node (which is more benign). If the QRS is wide (owing to bundle branch block or other conduction delay), block in the AV node is still most common but block in the His-Purkinje system is more frequent than when the QRS complex is narrow.[Figure caption and citation for the preceding image starts]: ECG showing 2:1 atrioventricular (AV) blockFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: ECG showing 2:1 atrioventricular (AV) blockFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing 2:1 atrioventricular (AV) blockFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].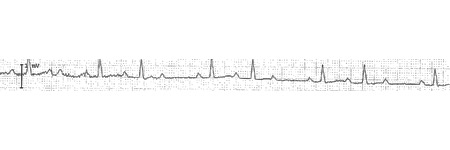
High-degree: more than one sequentially blocked P-wave. Block can be at the level of the AV node or the His-Purkinje system, as is the case with 2:1 AV block.
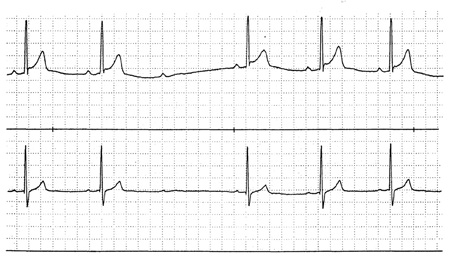
Third-degree AV block: occurs when there are no conducted impulses from the atria to the ventricles. There is no consistent PR relationship. It may occur with ventricular or junctional escape rhythm.[Figure caption and citation for the preceding image starts]: ECG showing complete atrioventricular (AV) blockFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: ECG showing complete atrioventricular (AV) blockFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing complete atrioventricular (AV) blockFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: ECG showing complete atrioventricular (AV) block with ventricular escapeFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing complete atrioventricular (AV) block with ventricular escapeFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: ECG showing complete atrioventricular (AV) block with ventricular escapeFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing complete atrioventricular (AV) block with ventricular escapeFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].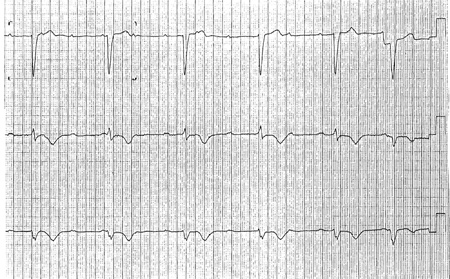 [Figure caption and citation for the preceding image starts]: ECG showing complete atrioventricular (AV) block with junctional escapeFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing complete atrioventricular (AV) block with junctional escapeFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
Paroxysmal AV block: normal AV nodal conduction followed by sudden block of AV conduction associated with a long pause and multiple blocked P-waves, with subsequent resumption of AV conduction. This may begin with an ectopic impulse.
Vagotonic AV block: slowing of the sinus node with prolongation of the PR interval followed by AV block owing to transient abrupt increase in parasympathetic tone.
Congenital complete heart block: usually associated with a narrow QRS complex escape rhythm arising in the AV node.
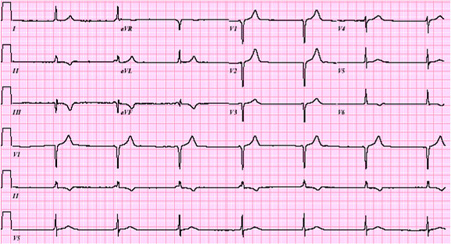
Escape rhythms may also occur in AV block, such as atrial (abnormal P-wave and decreased PR interval), junctional (above the bundle of His, produces a rate of approximately 40-60 bpm and narrow QRS complexes), and ventricular rhythms (below the bundle of His, produces a slower rate of 20-40 bpm and wide QRS complexes). [Figure caption and citation for the preceding image starts]: ECG showing junctional rhythmFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
Atrioventricular dissociation
Independent activation of the atria and ventricles results in no fixed relationship between the P-waves and the QRS complexes. The PR intervals are variable in a random fashion. Ventricular rate is the same as or faster than the atrial rate. There are 2 types:
Isorhythmic: when the atrial rate is the same (or nearly the same) as the ventricular rate but the P-wave is not conducted
Interference: when P-waves and QRS rates are similar but, occasionally, the atria conduct to the ventricles. [Figure caption and citation for the preceding image starts]: ECG showing interference atrioventricular (AV) dissociationFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: ECG showing interference atrioventricular (AV) dissociationFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing interference atrioventricular (AV) dissociationFrom the collection of Brian Olshansky, MD, FAHA, FACC, FHRS, FESC; used with permission [Citation ends].
Laboratory investigations
There are no specific laboratory investigations used to diagnose bradycardia; however, initial work-up should include thyroid function tests and a complete metabolic panel to rule out electrolyte disturbances, particularly hyperkalaemia, hypokalaemia, hypercalcaemia, and hypocalcaemia.[41] Cardiac enzymes should be obtained if bradycardia is associated with ECG changes suggestive of myocardial infarction or ischaemia. Patients who have junctional bradycardia and who are prescribed digoxin should have their serum digoxin level checked. Patients with chronic bradycardia may have evidence of worsening renal function. Any additional laboratory testing should be guided by information obtained by history and physical examination to aid identification of the underlying cause.
Other initial investigations
Holter or event monitoring, exercise testing, carotid sinus massage, and echocardiogram all form part of the initial work-up in addition to the ECG and are especially useful for intermittent bradycardia or patients with symptoms. If patients have sinus bradycardia, they should be further evaluated only if they are symptomatic or show evidence of haemodynamic compromise.
Holter monitoring
Enables correlation of symptoms with episodes of bradycardia.[41] Diagnostic clues are obtained in 50% to 70% of patients with bradycardia suspected on clinical grounds.[42][43] However, events can be missed if symptoms do not occur in the 24- to 48-hour monitoring period.
Asymptomatic bradycardia and pauses (especially nocturnal) are not uncommon in the normal heart and are probably non-diagnostic.
Shows sinus pauses, sinus arrest, second- or third-degree AV block, or severe sinus bradycardia with symptoms. First-degree AV block or Mobitz type I AV block may be noted while patients are asleep owing to high vagal tone.
May be used if severe sinus node dysfunction (e.g., sinus exit block, sinus pauses, sinus arrest, or tachy-brady syndrome) is suspected but cannot be documented.
May help distinguish the location of the block (i.e., AV node versus His-Purkinje system) in 2:1 and high-degree AV block. A long-monitored strip should be run because 2:1 AV block is unlikely to persist. The other forms of AV block (Mobitz I or II) should then become apparent. Monitoring while the patient does some form of exertion (e.g., arm exercise, standing, and walking) may also help to demonstrate the level of block. Block at the level of the AV node should improve with the adrenergic stimulation, but block below the AV node in the His-Purkinje system may worsen as AV nodal conduction improves and increases the frequency of inputs to the His-Purkinje system.
Event monitoring/mobile cardiac telemetry
Widely used in the diagnosis of symptomatic bradycardia and can be worn for up to 30 days.
Earlier designs were patient-triggered and so relied on the patient being able to recognise his or her symptoms and activate the monitor in a timely manner. This issue has been corrected by newer-generation monitors with auto-triggering capability.
Smartphone event monitors convert cardiac electric signal to an ultrasound FM sound signal, which is then demodulated to a digital ECG tracing. The ECG is generated in real time and can also be stored and instantaneously transmitted to a secure server for further analysis.
Photoplethysmographic-based smart devices (e.g., watches) may also be used.
Shows sinus pauses, sinus arrest, second- or third-degree AV block, or severe sinus bradycardia with symptoms. May be used if severe sinus node dysfunction (e.g., sinus exit block, sinus pauses, sinus arrest, or tachy-brady syndrome) is suspected but cannot be documented. Particularly useful in diagnosing Mobitz I AV block.
Exercise testing
A sub-normal increase in heart rate after exercise (chronotropic incompetence) can be useful in diagnosing sinus node dysfunction.[42][44] However, sensitivity and specificity are unclear and the results obtained may not be reproducible.[45] Even so, exercise-induced AV block, even if asymptomatic, can be significant and suggests disease of the His-Purkinje system.
Identifying symptoms owing to sinus bradycardia can be difficult; however, exercise testing can be useful to help determine sinus node dysfunction as the cause of symptoms.
Useful in determining level of block in second-degree AV block.
Useful for exercise-induced symptoms where AV block is suspected.
Carotid sinus massage
Performed during continuous ECG monitoring (after evaluating for the presence of carotid bruit by direct auscultation) in the evaluation of carotid sinus hypersensitivity, which causes symptomatic bradycardia and is associated with sinus node dysfunction.[41]
Diagnostic yield of carotid sinus massage can be increased by performing this during head-up tilting.[46]
A pause of over 3 seconds with symptoms is indicative of a cardio-inhibitory response from carotid sinus hypersensitivity.
Can help diagnose Mobitz I and II AV block; it will accentuate Wenckebach in the AV node but will have an opposite effect if the block is below the His bundle.
May help distinguish the location of the block (i.e., AV node versus His-Purkinje system) in 2:1 and high-degree AV block. It may improve block in the His-Purkinje system by slowing the sinus and AV nodal inputs to the His-Purkinje system, enabling the His-Purkinje system longer in which to recover between inputs.
Care should be taken when performing this manoeuvre and evaluation for carotid bruit should be performed before it is attempted.
Echocardiogram
Although it provides no direct diagnostic role for bradycardia, it provides valuable information regarding underlying heart disease that can influence management and decision making. Patients with significantly reduced left ventricular systolic function may have underlying obstructive coronary artery disease and should be considered for either non-invasive testing (such as myocardial perfusion imaging) or invasive testing (coronary angiography) based on the index of clinical suspicion. This is particularly important in the presence of left bundle branch block or right bundle branch block and left anterior hemiblock in association with symptomatic bradycardia (e.g., syncope). These patients are more likely to develop bradycardia particularly due to AV block. Patients who are found to have significantly reduced left ventricular systolic function should be referred for an implantable cardioverter defibrillator (ICD) if clinically appropriate.[41]
Further investigations
Implantable-loop recorder
A subcutaneous monitoring device used for the detection of cardiac arrhythmias. Typically implanted under local anaesthesia in the left parasternal or pectoral region. Small devices can be inserted by a qualified physician using an injection approach, and can be used for monitoring for up to 3 years.
Useful modality if a patient has infrequent symptoms that are difficult to record with non-invasive tools such as ECG, Holter monitors, and/or event monitors due to their infrequent nature, but are suspected to be secondary to a bradyarrhythmia. It is safe and efficacious in these settings.[47][48]
Also useful to rule out bradyarrhythmia as a cause of symptoms by identifying normal sinus rhythm at the time of a symptom event of interest.
May show sinus pauses, sinus arrest, second- or third-degree AV block, or severe sinus bradycardia with symptoms. May be used if severe sinus node dysfunction (e.g., sinus exit block, sinus pauses, sinus arrest, or tachy-brady syndrome) is suspected but cannot be documented. It is particularly useful in diagnosing Mobitz I AV block.
Tilt-table testing
Used to evaluate adequacy of the autonomic system, especially when there is suspicion of neurocardiogenic syncope with a paroxysmal drop in heart rate due to vagal activation.[41]
A commonly used method is head-upright tilting, which causes dependent venous pooling and thereby provokes the autonomic response.
Electrophysiological testing
Recommended when symptoms cannot be correlated clearly and when significant bradyarrhythmias are suspected based on presentation and other clinical information but cannot be diagnosed by non-invasive modalities.[41]
Electrophysiological measurements of sinus node function serve only as an adjunct to clinical and non-invasive parameters because these tests are based on assumptions that limit their validity and clinical utility.
There is little utility for electrophysiology testing in already-documented second- and third-degree AV block. Testing can be useful in patients with AV block and no clear symptom association; in patients with symptoms of bradycardia in whom AV block is suspected but not documented; and when the site of AV block cannot be determined reliably by surface tracings.
His-ventricle interval of over 100 milliseconds in a patient with bradycardia, even in the absence of symptoms, is a high-risk finding.[49][50]
Overall, the role of electrophysiological testing for bradycardia is limited, owing to low sensitivity and specificity. Positive findings may not be the reason for patient symptoms.[51][52]
May be used if severe sinus node dysfunction (e.g., sinus exit block, sinus pauses, sinus arrest, tachy-brady syndrome) is suspected but cannot be documented.
Atrial pacing at progressively shorter cycle lengths during an electrophysiology study can manifest Mobitz type I in subjects with normal or abnormal AV node conduction.
Useful to demonstrate the location of the block (i.e., AV node versus His-Purkinje system) in 2:1 and high-degree AV block.
Nocturnal pulse oximetry or overnight polysomnography
Useful for patients with symptoms suspicious for SDB, including daytime somnolence, multiple night-time awakenings, morning headaches, loud snoring, and dry mouth on awakening.
Prior to pacemaker placement, patients with risk factors for SDB should be evaluated with polysomnography. In one small study, eight patients with asymptomatic bradyarrhythmias were referred for pacemaker evaluation; seven of the patients had bradyarrhythmias only at night or during the day while asleep.[53] Patients with symptoms suggestive of sleep apnoea were referred for overnight polysomnography studies that were all positive for obstructive sleep apnoea. Treatment for sleep apnoea led to reduced sleep apnoea symptoms and continued asymptomatic nocturnal bradyarrhythmias without pacemaker therapy after a 22-month follow-up. Therefore, it is paramount to screen patients for sleep apnoea when presenting with nocturnal bradycardia before pacemaker placement. This is especially true when asymptomatic nocturnal bradycardias are noted on inpatient overnight cardiac monitoring, or home-based smartphone or watch sleep monitoring apps.
Guidelines recommend that all patients with bradycardia or conduction disorder during sleep and documented SDB should be treated for SDB.[11][25]
Particularly in patients with nocturnal bradyarrhythmias or conduction disturbances that are asymptomatic, treatment of obstructive sleep apnoea may prevent progression to symptomatic conduction delays.
How to record an ECG. Demonstrates placement of chest and limb electrodes.
Use of this content is subject to our disclaimer
