Aetiology
The association of SLD with inflammatory changes and fibrosis in obese patients was first described over 50 years ago. The term metabolic dysfunction-associated steatohepatitis was first used to describe a group of patients who developed liver failure following surgical jejunoileal bypass for obesity.[17][18]
Metabolic dysfunction-associated steatotic liver disease (MASLD) is commonly associated with other metabolic comorbidities including obesity, diabetes mellitus, hypertension, dyslipidaemia, obstructive sleep apnoea, cardiovascular diseases, and chronic kidney disease.[3][7] Rates of MASLD occurrence are higher in patients with hypothyroidism, hypogonadism, growth hormone deficiency, and polycystic ovarian syndrome.[3]
Pathophysiology
Most experts now consider fatty liver as the hepatic manifestation of metabolic syndrome.[19] The most widely held hypothesis implicates insulin resistance as the key mechanism leading to the accumulation of excessive triglyceride accumulation in the liver and subsequent development of SLD.[3] Once steatosis is present, some have proposed a second hit or additional oxidative injury, which is required to manifest the necro-inflammatory component seen in steatohepatitis. Antioxidant deficiencies; hepatic iron; fat-derived hormones, including leptin, adiponectin, and resistin; and intestinal bacteria have all been implicated as potential oxidative stressors. Hence, metabolic dysfunction-associated steatohepatitis (MASH) is a subset of MASLD.[20]
Classification
Clinico-pathological classification of metabolic dysfunction-associated steatotic liver disease[4]
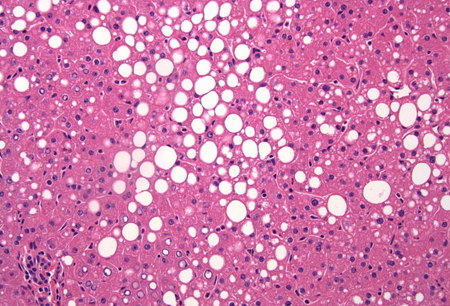
Steatosis
Macrovesicular or mixed predominantly macro-/microvesicular without evidence of inflammation or fibrosis (bland).[Figure caption and citation for the preceding image starts]: A wedge biopsy of the liver from a 52-year-old female organ donor; the biopsy shows moderate mixed micro- and macrovesicular steatosis; there is no significant lobular inflammation or necrosis (haematoxylin and eosin, [H&E] stain, x 200)From the collection of Kapil B. Chopra, MD [Citation ends].
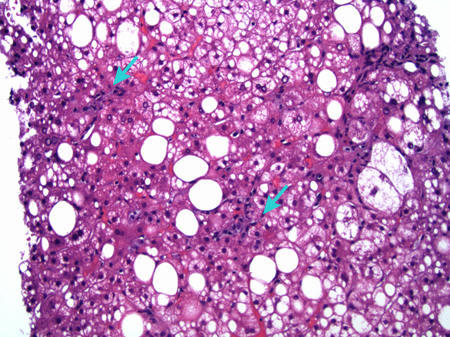
Steatohepatitis (metabolic dysfunction-associated steatohepatitis or MASH)
Macrovesicular or mixed predominantly macro-/microvesicular steatosis with evidence of hepatocyte ballooning degeneration, mild diffuse lobular mixed acute and chronic inflammation, and perivenular perisinusoidal collagen deposition.[Figure caption and citation for the preceding image starts]: A case of metabolic dysfunction-associated steatohepatitis; the biopsy shows ballooning degeneration of the hepatocytes (middle right) and spotty lobular inflammation in addition to mixed micro- and macrovesicular steatosis (H&E, x 200)From the collection of Kapil B. Chopra, MD [Citation ends].
MASH-associated fibrosis
Wound healing response in which damaged regions of chronic inflammatory disease are encapsulated by extracellular matrix or scar tissue. In its initial stages, fibrosis is thought to be reversible to some degree, but in the late stages it is felt to be irreversible. In MASH, fibrosis is staged 0 to 4.
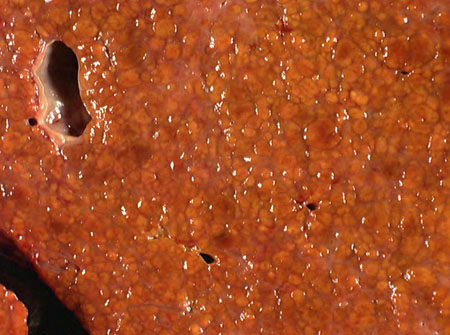
MASH-associated cirrhosis
Histological definition connoting the last stage of progressive hepatic fibrosis. Characterised by the distortion of hepatic architecture and the formation of regenerative nodules. It is traditionally believed to be an irreversible condition.[Figure caption and citation for the preceding image starts]: A native hepatectomy specimen from a patient with a history of metabolic dysfunction-associated steatohepatitis; a cross-section of the liver shows mixed, predominantly micronodular cirrhosis; the orange-yellow colour of the nodules is due to moderate mixed micro- and macrovesicular steatosis involving 40% of the liver parenchymaFrom the collection of Kapil B. Chopra, MD [Citation ends].
MASH-associated end-stage liver disease
Term used to describe the stage at which patients with cirrhosis develop clinical complications. A majority of the complications are sequelae and manifestations of advanced fibrosis, with portal hypertension and decreased synthetic function of the liver. They include ascites, portosystemic encephalopathy, variceal bleeding, hepatocellular carcinoma, and the hepatorenal and hepatopulmonary syndromes.
Histological scoring system definition[5]
The NASH Clinical Research Network scoring system is the standard histological scoring system used to characterise MASLD. It is composed of five broad histological categories: steatosis, inflammation, hepatocellular injury, fibrosis, and miscellaneous features. A score of 1 defines possible or borderline steatohepatitis, with 2 or greater indicating definite steatohepatitis.
Use of this content is subject to our disclaimer