History and exam
Key diagnostic factors
common
disclosure of inappropriate contact
Disclosure of any inappropriate contact should prompt a complete sexual abuse or assault evaluation and report to the appropriate child protective agency. It is preferable to record the disclosure of abuse in the patient's own words, rather than in a summary statement.[34]
uncommon
acute anogenital trauma (any change); transections and absent hymen (in children)
Transections (complete tears of the hymen) and absent hymen are indicative of trauma to this area.[Figure caption and citation for the preceding image starts]: Acute vaginal trauma in an 11-year-old victim of abduction and rapeGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].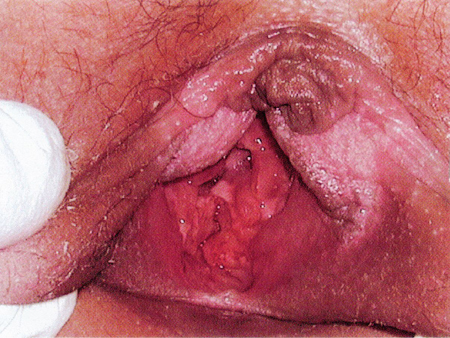 [Figure caption and citation for the preceding image starts]: Absent hymen from 4 to 7 o'clock position in a sexually active 14-year-old girlGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Absent hymen from 4 to 7 o'clock position in a sexually active 14-year-old girlGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].
The majority of sexually abused children have normal genital examination findings. Even in cases of confirmed sexual abuse, normal genital findings are common.[41]
sexually transmitted infections
In children, confirmation of certain infections (HIV, syphilis, gonorrhoea, chlamydia, trichomonas) is diagnostic of sexual contact once perinatal (and percutaneous, in the case of HIV) transmission is excluded, while others (herpes simplex virus, anogenital condyloma acuminatum) are suspicious for sexual contact.[34][47] Bacterial vaginosis is inconclusive for sexual contact. In sexually active adults, it is often difficult to determine whether infections resulted from sexual assault or were pre-existing.
Other diagnostic factors
common
normal genital findings
The majority of sexually abused children and approximately half of assaulted adult women have normal genital examination findings. Even in cases of confirmed sexual abuse, normal genital findings are common.[41]
uncommon
anogenital lesions
Warts, ulcers, and bruises or petechiae may be indicative of sexual contact or trauma and warrant further investigation.[34]
Molluscum contagiosum, rashes, haemangiomas, nevi, lichen sclerosus, and urethral prolapse can be confused with signs of sexual abuse or assault. A repeat examination after 1 to 2 weeks may aid diagnosis, as these lesions will probably persist, whereas physical signs of sexual abuse will resolve or heal over time.
In adults, evidence of sexually transmitted infections generally results from previous sexual contact.
Anal fissures and tags are non-specific findings that may result from trauma to the anus or other conditions. Peri-anal laceration with exposure of tissue below the dermis is indicative of blunt force penetrating trauma.
Anogenital condyloma accuminata raises suspicion of sexual contact.[34] Human papillomavirus may be acquired from birth but present months or even years later. Lesions appearing for the first time in a child older than 5 years of age may be more likely to be the result of sexual transmission.
Anogenital ulcerations may be due to herpes simplex virus. Once herpes simplex infection is confirmed, this raises suspicion of sexual contact.[34]
labia and perineum injury
Injuries to the pubis, labia, and perineum may occur with accidental trauma such as a straddle injury, or may be associated with sexual abuse. A thorough history can help with diagnosis.[34]
non-genital injuries
May be associated with sexual abuse or assault. A thorough history and complete physical examination can help determine the aetiology.
vaginal or penile discharge
This is a non-specific finding that should prompt testing for sexually transmitted infections as well as routine culture for other infections. Vaginal discharge is common in non-abused and abused girls and women.
Once trichomonas infection is confirmed, this gives a high suspicion for sexual contact.[34] Bacterial vaginosis is inconclusive for sexual contact.[34]
Once infection with gonorrhoea or chlamydia is confirmed, this is diagnostic of sexual contact if perinatal transmission is excluded.[34]
harmful behaviours
Harmful behaviours can include substance misuse, and thoughts or acts of self-harm or attempted suicide.[38]
sexual behaviour problems in children
chronic medical complaints in children
May indicate child psychological stress.
frequent or persistent genitourinary complaints
May indicate child psychological stress or sexually transmitted infection.
hymenal notches
Notching of the hymen may result from trauma.
Notching should be confirmed in pre-pubertal girls using the knee-chest position, and in older girls by using a cotton swab or other device.[Figure caption and citation for the preceding image starts]: Knee-chest position for examination of a pre-pubertal girlGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].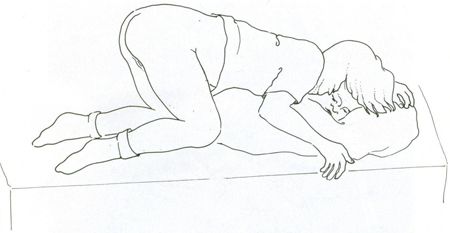
Indeterminate findings include: deep notches or clefts in the posterior/inferior rim (between 3 and 9 o'clock) of the hymen in pre-pubertal girls; deep notches or complete clefts in the hymen at 3 or 9 o'clock in adolescent girls; complete clefts/transections at 3 or 9 o’clock.
Risk factors
weak
sexual abuse of other children in the home
Sexual abuse of other children in the home should prompt sexual abuse evaluation. The strength of association of sexual abuse of other children in the home to sexual abuse of the presenting child is unclear.[17]
childhood exposure to intimate partner violence
adolescents and young women
Adolescents and young women are the most likely groups to be sexually assaulted.
poverty or homelessness
People with a low income and homeless people are at increased risk of sexual assault.[15]
sex workers
Sex workers are at increased risk of sexual assault.[15]
living in institutions or areas of conflict
People living in institutions or in areas of conflict are at increased risk of sexual assault. A history of sexual assault is more prevalent among incarcerated women than among the general female population.[16]
Use of this content is subject to our disclaimer