History and exam
Key diagnostic factors
common
presence of risk factors
Key risk factors include use of alcohol, tobacco, or betel; chronic candidiasis; immunosuppression; and some genetic conditions.
homogeneous white plaques
Majority are found along the lateral tongue margin, floor of the mouth, and buccal/labial mucosa. Less commonly may be seen within the retromolar region. [Figure caption and citation for the preceding image starts]: Homogeneous leukoplakiaCourtesy of Dr James Sciubba; used with permission [Citation ends].
other causes for white lesions excluded
Local, traumatic causes, infections, neoplasms, and mucocutaneous diseases must be ruled out for a diagnosis of oral leukoplakia to be made.
uncommon
non-homogeneous appearance
Speckled leukoplakia has a mixed red-and-white appearance with the presence of red (atrophic) areas irregularly scattered within the keratotic or white component.
Nodular leukoplakia has small aggregated hemispherical red or white surface alterations or excrescences that may show a red background or substrate.
Sublingual leukoplakia (sublingual keratosis) is characterised by wide areas of smooth to heterogeneous surface alterations over the floor of the mouth, sometimes extending to the ventral tongue surface. It is associated with an increased degree of dysplastic to malignant change, with some stating that nearly 1 in 2 cases may become malignant, although lower rates have also been reported.[128][129]
Proliferative verrucous leukoplakia is characterised by a verruciform, progressive, often multifocal keratosis. It is the least common type of oral leukoplakia but has a high risk of progressive dysplasia and malignant transformation.[130] [Figure caption and citation for the preceding image starts]: Speckled leukoplakiaCourtesy of Dr James Sciubba; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Proliferative verrucous leukoplakiaCourtesy of Dr James Sciubba; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative verrucous leukoplakiaCourtesy of Dr James Sciubba; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Sublingual leukoplakiaCourtesy of Dr James Sciubba; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Sublingual leukoplakiaCourtesy of Dr James Sciubba; used with permission [Citation ends].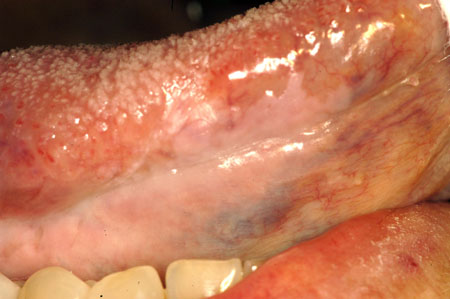
Other diagnostic factors
common
male sex
Oral leukoplakia is more common in men than in women in a ratio of 2:1.
age >40 years
More than 80% of cases of oral leukoplakia occur in patients older than 40 years, with most cases occurring between 40 and 70 years of age.[131]
Risk factors
strong
tobacco use
Tobacco in all of its forms (smoking and smokeless; chewed, snuff, within betel quid) is strongly linked to the formation of oral mucosal alterations in the form of leukoplakia, as well as other oral mucosal conditions including erythroplakia and submucous fibrosis.
Positive dose-relationships are noted with chewing tobacco habit in the production of multiple pre-malignant lesions.[25][26][27]
alcohol use
Alcohol consumption is an independent risk factor and a common accompaniment to tobacco use.[28]
While the primary or specific mechanisms of ethanol-induced carcinogenesis have been poorly defined, data have demonstrated that acetaldehyde, the first ethanol metabolite, and lipid peroxidation-derived adducts are formed within the oral mucosa in abusers of alcohol with leukoplakia.[29]
Contributing to the role of alcohol-induced leukoplakia is its proven enhancement of mucosal permeability that allows the entry of tobacco carcinogens through the epithelial layers.[30]
In never-users of tobacco, and irrespective of the type of beverage and drinking pattern, alcohol has been shown to be related to leukoplakia development.[31][32]
areca nut (betel quid) use
While the use of betel leaf alone has not been confirmed to contribute to leukoplakia development, the combinations of ingredients used in the quid are implicated. The quid is formed by the betel leaf envelope and a combination of areca nut, spices, slaked lime, and resins. Areca nut is the primary ingredient that is classified by the International Agency for Research on Cancer as a carcinogen. Tobacco may also be added to the quid.
Where tobacco is absent from the betel quid, there is a direct dose-response relationship in the frequency and duration of areca nut chewing and the risk of oral pre-cancers (including leukoplakia).[33] In the presence of concomitant tobacco use (smoking), the annual incidence rate for leukoplakia is higher than in non-smokers.[34]
The addition of the areca nut as thin shavings, strips, or ground powder in the absence of tobacco plays an important role in oral pre-cancerous and cancerous lesion development.[35]
A stated mechanism in the pathogenesis of oral precancerous lesions in association with areca nut chewing relates to the high frequency of hypermethylation of p14, p15, and p16, independent of p53 mutations, as well as mutations in the epidermal growth factor receptor (EGFR; Q787Q mutation in exon 7).[36][37]
chronic candidiasis
The precise role of chronic intra-oral candidal infection (candidiasis) in the development or aetiology of leukoplakia remains uncertain.
Debate revolves around the idea that candidal infection is superimposed on a pre-existing leukoplakia or dysplastic lesion versus the demonstrated association that certain Candida albicans biotypes have a high nitrosation potential indicative or suggestive of an endogenous nitrosamine synthesis.[38][39]
In support of the infectious aetiology is the demonstrated conversion of non-homogeneous leukoplakia to homogeneous leukoplakia with antifungal therapy, with some lesions disappearing completely.[40]
One study found a significant association between histologically confirmed fungal infection in association with epithelial dysplasia, while there was a significant negative association of fungal infection with benign hyperkeratosis and lichenoid reactions.[41]
genetic predisposition
Certain variant haplotypes may predispose to leukoplakia and oral cancer; variants on the XRCC1 and GSTM3 loci are associated.[42] Mitochondrial polymorphisms may also be important. Inherited bone marrow failure and disturbed telomere biological syndromes typified by dyskeratosis congenita carry a significantly higher risk of leukoplakias developing into squamous carcinoma.[43]
immunosuppression
Fanconi's anaemia
In Fanconi's anaemia - a rare autosomal recessive bone marrow failure syndrome characterised by aplastic anaemia, leukemia, and other cancers (including oral cancer) - accompanying oral leukoplakia. Skin lesions may present as pigmented, reticulated forms. Dystrophic nails reminiscent of dyskeratosis congenita may also be seen.[46]
Oral lesions in patients with fully expressed Fanconi anaemia was reported in 45% of patients in one study.[47] However, in a series of paediatric Fanconi's anaemia patients, no oral lesions considered to be leukoplakia or other pre-cancerous lesions were noted.[48]
weak
sunlight exposure
HPV infection
Oncogenic strains of the HPV - in particular, types 16 and 18 - are likely to be critical aetiological factors in oropharyngeal and tongue base squamous cell carcinoma. However, a similar association with these strains of HPV and oral cavity cancer and leukoplakia has not been made.
Although some proliferative verrucous leukoplakias have been found to harbour HPV, an aetiological role has not been proven.[52] In one study, <30% of oral leukoplakias analysed were positive for both HPV-6/11 and HPV-16, although more recently, with the use of in situ hybridisation, HPV has been reported as a specific risk factor for the development of potentially malignant oral lesions.[53][54] The significance of these findings remains unclear.
Treponema pallidum infection (syphilis)
The association of late-stage syphilis has historically been strongly linked to oral leukoplakia and squamous cell carcinoma of the dorsum of the tongue, although on a worldwide basis the reporting of this association has been uncommon in recent years as a result of treatment of early stage syphilis and cure. The previous treatment regimens using heavy metals such as arsenicals with known carcinogenic properties may have contributed to carcinoma of the tongue in syphilis patients.
However, it has been demonstrated that 8% of patients with malignant and pre-malignant lesions of the tongue had syphilis antibodies present.[55] In addition, some data suggest that patients with syphilis have a raised incidence of cancer of the tongue.[56]
Routine testing is not recommended but may be appropriate in select patients.
Use of this content is subject to our disclaimer