Approach
Treatment of osteochondritis dissecans is joint-specific.
Definition of terms used in treatment
Stable lesion: a stable lesion is one that maintains its subchondral stability and remains located in its bed. It may or may not have intact articular cartilage. The patient will usually deny mechanical symptoms including catching or locking. The patient may or may not have recurrent effusions.
Unstable lesion: subchondral stability of the lesion is lost. The lesion may or may not remain in its original bed. Mechanical symptoms may be present (including catching, locking, recurrent effusion). Stability of the lesion is often assessed with magnetic resonance imaging (MRI).
Skeletally immature: physes remain open or unfused.
Skeletally mature: physes are fused.
Failure of conservative/non-operative treatment: symptoms persist despite an adequate trial of non-operative treatment for a minimum of 6 weeks.
Prolonged conservative care involves at least 6 weeks of conservative management that may involve the following:
Activity modification which is done to the point of pain relief. For many active athletes, discontinuing competitive athletics will result in resolution of symptoms.
Protected weight-bearing with crutches should be offered for patients with continued discomfort with ambulation alone.
Short-term immobilisation can be done with a cast or knee immobiliser, however the role of short-term immobilisation is unclear. Prolonged immobilisation should be avoided.[3]
Pain relief may be gained with the use of non-steroidal anti-inflammatory drugs (NSAIDs) or paracetamol, but symptom relief may interfere with monitoring of disease progression and therefore should be used judiciously.
Malalignment: weight-bearing line (mechanical axis) passes through the extremes of either the medial or lateral compartment. A weight-bearing line that passes through the involved compartment may inhibit healing or exacerbate symptoms.
Reducible: lesion is intact and large enough to be placed back in its bed and fixed in place.
Non-reducible: lesion is unable to be placed back in original bed because of fragmentation or osteolysis, or because the lesion is not large enough for fixation to be feasible.
Osteochondral allograft: a current technique for the salvage of full-thickness defects. The technique involves taking a matching osteochondral plug from an allograft specimen to replace the full-thickness defect.
Autologous chondrocyte implantation: involves a primary procedure for cartilage biopsy to harvest the autologous chondrocytes. The autologous chondrocytes are then cultured. In a second procedure, the cultured autologous chondrocytes are implanted below a periosteal flap covering the osteochondral defect.
Knee
1. Stable lesions
In the skeletally immature patient
Initial treatment includes activity modification, protected weight-bearing, short-term immobilisation, and pain relief (NSAIDs and/or paracetamol).
Evidence indicates large (288.0 ± 102.6 mm²) but stable lesions are less likely to heal over 6 months of conservative care.[36] A logistic regression model was predictive of healing status based on patient age, normalised lesion size (relative to the femoral condyle), and presenting symptoms (giving way, swelling, locking, or clicking)
If there is failure of non-operative treatment (symptoms persist without improvement over 6 months) or if the lesion becomes unstable, surgery is recommended.[37] Surgical treatment involves drilling the subchondral bone with the intention of stimulating vascular ingrowth and subchondral bone healing.[3] Osteotomy or guided growth may be considered if malalignment is present.[Figure caption and citation for the preceding image starts]: After drilling of lesion, complete resolution (healing) of osteochondritis dissecans lesionFrom the collection of H. Chambers, MD [Citation ends].
 [Figure caption and citation for the preceding image starts]: Healed osteochondritis dissecansFrom the collection of H. Chambers, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Healed osteochondritis dissecansFrom the collection of H. Chambers, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Healed osteochondritis dissecansFrom the collection of H. Chambers, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Healed osteochondritis dissecansFrom the collection of H. Chambers, MD [Citation ends].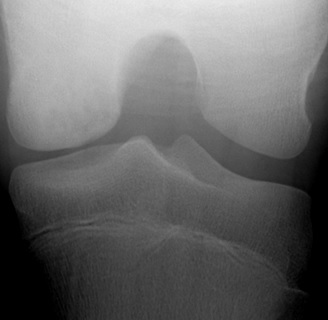 [Figure caption and citation for the preceding image starts]: Magnetic resonance imaging (MRI) of knee demonstrating healingFrom the collection of H. Chambers, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Magnetic resonance imaging (MRI) of knee demonstrating healingFrom the collection of H. Chambers, MD [Citation ends].
In the skeletally mature patient
Activity modification, protected weight-bearing, short-term immobilisation, and pain relief. Osteotomy may be considered if malalignment is present.
If there is failure of non-operative treatment or the lesion becomes unstable, surgery (transchondral or retroarticular drilling) is recommended.[3] Success of drilling is better in skeletally immature patients, but the technique is warranted in all patients with a stable lesion where conservative management has failed.
Note: adult osteochondritis dissecans lesions have a greater propensity for instability and typically follow a clinical course that is progressive and unremitting. The majority of adult osteochondritis dissecans lesions necessitate surgical intervention. However, in the adult patient with a stable lesion, non-operative treatment should be the first line of management.
2. Unstable lesion or failure of conservative management: arthroscopy is indicated. Depending on findings, the procedure will be as follows.
If lesions appear stable but conservative management has failed, transchondral or retroarticular drilling is performed.
If lesions appear unstable but reducible, fixation is performed.
Poly 96L/4D-lactide copolymer bioabsorbable implants seem to be safe and effective for the management of unstable juvenile osteochondritis dissecans lesions of the knee. In addition, non-absorbable screws, pins, and nails have also shown efficacy.
If lesions appear unstable with fragmentation or osteolysis, fixation with bone graft augmentation is performed. If lesions are reducible but subchondral support is lost, fragment excision is performed. If lesions are fragmented or irreducible, salvage techniques are used.
If lesions appear unstable and chondral damage is present, fragment excision and chondrocyte transplant, microfracture, osteochondral graft, or synthetic grafting are indicated. Each of these techniques has advantages and disadvantages. Studies have yet to show which salvage technique provides the best outcome.
Elbow
Management depends on the stability of the lesion, which can be determined using clinical history, physical examination, MRI, and bone scans.[5] The lack of mechanical symptoms including catching or locking and the absence of an effusion would suggest that the lesion is stable.
1. Stable lesion with intact articular cartilage and in situ subchondral fragments
Initial treatment is conservative. Sport and other aggravating activities should be avoided for 3 to 6 weeks until symptoms subside with NSAIDs and/or paracetamol for symptomatic treatment. Some specialists recommend a hinged elbow brace for protection. Physiotherapy begins once symptoms have abated. Unrestricted sport activity may begin 3 to 6 months after treatment is initiated.[8] Conservative management has shown favourable results when the lesion is detected early.[38]
2. Persistent symptoms despite conservative treatment, intra-articular loose bodies, or evidence of instability, including violation of intact cartilage or detachment
These patients require surgery.[39] The only widely agreed treatment includes arthroscopic removal of intra-articular loose bodies. An open arthrotomy may be necessary if there is a large fragment.
Debate continues with regards to excision of the unstable fragment with subchondral drilling or abrasion chondroplasty versus attempted fixation of the segment with or without bone graft.[8]
3. Salvage techniques
The role of salvage procedures is not yet well defined. These include wedge osteotomy, osteochondral grafting, periosteal grafting, perichondral grafting, and articular cartilage allograft transplantation.
Ankle (involving the talus)
For asymptomatic lesions, low-symptomatic lesions, and stable lesions with intact articular surface, conservative management is recommended:
Initial treatment includes activity modification, short-term immobilisation, and protected weight-bearing protocol with a stable lesion with an intact articular surface. NSAIDs and/or paracetamol are used for symptomatic treatment.
One series reported that 77% of patients treated with 6 months of conservative therapy continued to have symptoms and persistent lesions on radiograph.[40] An additional 6 months of conservative management for those patients with persistent lesions resulted in 42% having surgery for unhealed lesions and pain.
If there is failure of conservative management, there are intra-articular loose bodies, or the lesion becomes unstable, surgery is recommended.
Surgical management options include:
Debridement and bone marrow stimulation (microfracture, abrasion arthroplasty, drilling).
Fixation of the lesion to the talar dome (retrograde drilling, internal fixation, bone graft).
In cases of failed primary treatment, an osteochondral transplant or cultured chondrocyte transplant can be considered.[41]
Stimulating the development of hyaline cartilage (autologous chondrocyte implantation, osteochondral allograft or autograft).[42] Each of these techniques has advantages and disadvantages. Studies have yet to show which salvage technique provides the best outcome.[Figure caption and citation for the preceding image starts]: Osteochondral lesion of medial talusFrom the collection of H. Chambers, MD [Citation ends].
 [Figure caption and citation for the preceding image starts]: Healing after drilling of lesionFrom the collection of H. Chambers, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Healing after drilling of lesionFrom the collection of H. Chambers, MD [Citation ends].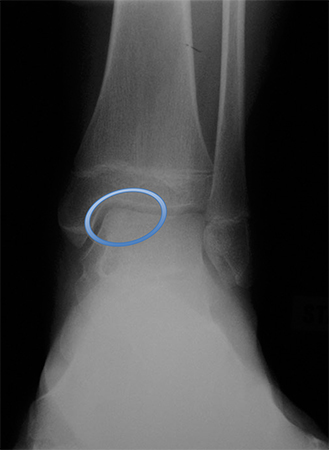
Use of this content is subject to our disclaimer