Approach
The three main joints involved include the knee, the ankle, and the radiocapitellar joint of the elbow. Examination should be joint-specific. The most critical factor influencing management of a patient with osteochondritis dissecans is the apparent stability or instability of the osteochondritis dissecans fragment.
History
The majority of patients with osteochondritis dissecans are adolescent or young adult athletes. Traumatic injury may or may not be associated with the onset of pain. If a history of trauma is present, specific questions regarding the type of injury should be asked.
Symptoms
Vague joint pain may be present. The pain may be exacerbated by increased activity (i.e., sport participation).
Clinical evaluation of the knee
Symptoms: stair-climbing or running up- or downhill will exert more force in the region of the osteochondritis dissecans and may further exacerbate the pain. Mechanical symptoms, including locking, catching, and recurrent effusion, may suggest an intra-articular loose body or an unstable osteochondritis dissecans lesion.
Gait: the patient may ambulate with an antalgic gait protecting the involved extremity. They may ambulate with an external rotation gait, attempting to unload the lateral aspect of the medial femoral condyle from the medial tibial spine.
Swelling: an effusion may be present, which can be appreciated with ballottement.
Wilson's test: may be positive, representing a lesion in the classic location, the lateral aspect of the medial femoral condyle. Wilson's test is performed by flexing the knee to 90º and internally rotating the tibia. The knee is then extended slowly. Worsening pain at 30º of flexion, which is relieved with external rotation of the tibia, represents a positive test. This test, however, has a rather low sensitivity and specificity.
Direct palpation: the joint line and the femoral condyles should be directly palpated to help differentiate meniscal from osteochondral pathology. Pain on the joint line is more likely to represent meniscal pathology, whereas tenderness along the femoral condyle may represent an osteochondral defect.
Loss of range of movement (ROM): a large effusion or intra-articular loose bodies may result in loss of motion, specifically terminal extension.
Quadriceps atrophy: this may be present with chronic injury.
Clinical evaluation of the ankle
Symptoms: mechanical symptoms, including locking, catching, and recurrent effusion, may be present, indicating an unstable osteochondritis dissecans or intra-articular loose body.
Gait: the patient may have an antalgic gait.
Swelling: an ankle effusion may be present and is most easily appreciated at the posteromedial and anterolateral aspect of the joint.
Direct palpation: with the ankle in maximum dorsiflexion, there may be tenderness with palpation over the posteromedial aspect of the talar dome. With the ankle in maximal plantar flexion, there may be tenderness with palpation over the anterolateral aspect of the talar dome.
Clinical evaluation of the elbow
Symptoms: the patient may complain of pain and tenderness over the lateral aspect of the elbow, specifically the capitellum.
Swelling: an effusion may be present.
Palpation: crepitus with pronation and supination may be elicited. Tenderness with palpation over the capitellum may be present.
Loss of ROM: often loss of motion, specifically extension, can be demonstrated.
Active radiocapitellar compression test may be positive. This can be elicited by applying a valgus force to the elbow with pronation and supination.
Plain x-rays
Knee views should include:
Standing anteroposterior view of the bilateral knees
Lateral view at 30º of flexion
Merchant or skyline view of the patellofemoral joint
Notch or posteroanterior (PA) flexion view.
Particular attention should be paid on the posterolateral aspect of the medial femoral condyle, which is often best seen on the notch or PA flexion view
Lower extremity alignment should be assessed with a full-length lower extremity film. If malalignment exists and the weight-bearing line passes through the involved compartment, some orthopaedic surgeons will consider an osteotomy to unload the involved compartment.[3]
[Figure caption and citation for the preceding image starts]: Tunnel view of osteochondritis dissecansFrom the collection of H. Chambers, MD [Citation ends].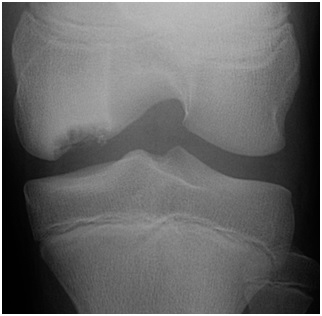 [Figure caption and citation for the preceding image starts]: Preoperative radiograph with large osteochondritis lesion of the femoral condyleFrom the collection of H. Chambers, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Preoperative radiograph with large osteochondritis lesion of the femoral condyleFrom the collection of H. Chambers, MD [Citation ends]. Ankle views should include:
Ankle views should include:
Anteroposterior
Lateral
Mortise of the ankle.
Heel rise view may reveal posterolateral or posteromedial defects.
Elbow views should include:
Anteroposterior
Lateral
Internal and external oblique.
Further imaging
All patients should first be evaluated with clinical examination and plain x-rays. In general, suspected soft-tissue injuries (sprains and strains) are best evaluated with magnetic resonance imaging (MRI), while subtle bony injuries are best visualised by computed tomography (CT). Further diagnostic studies may be chosen after orthopaedic consultation.
CT
This modality is very useful in identifying loose bodies within the joint. The sharp contrast between bone and soft tissue, along with the ability to obtain fine slices, make CT a good tool to identify loose bodies trapped within joint recesses and synovial folds. The ability to obtain axial, coronal, and sagittal images further enhances its utility in identifying osteochondral injury. This is particularly helpful if there is an effusion of the joint. If there is not an effusion, an arthrogram can be performed to evaluate the cartilage surface.
MRI
Gives direct visualisation of the chondral surface in axial, coronal, and sagittal planes. MRI has been shown to be a useful non-invasive mechanism to identify osteochondral lesions.[24][25][26] It helps to delineate the stability of the lesion as well as the location and number of lesions and loose bodies. The sensitivity of MRI to determine the extent of chondral injury compared with arthroscopy has ranged from 33% to 96% in available studies and usually underestimates the extent of the lesion.[27] MRI imaging protocol for juvenile osteochondritis dissecans is often centre-specific. Ideally, protocols should include a cartilage-sensitive sequence and a fluid-sensitive sequence. Attention is given to the amount of localised marrow oedema, as well as lesion location and size, and stability of an osteochondral fragment.[Figure caption and citation for the preceding image starts]: Coronal MRI image of the talus, showing an osteochondral lesion on the medial aspect of the talar domeGupta RK, Kansay R, Aggarwal V, et al. Osteochondritis dessicans of the talus in a 26-year-old woman. BMJ Case Reports 2009; doi:10.1136/bcr.06.2008.0091 [Citation ends]. [Figure caption and citation for the preceding image starts]: Sagittal magnetic resonance image (MRI) of the talus, showing an osteochondral lesion on the posterior aspect of the talar domeGupta RK, Kansay R, Aggarwal V, et al. Osteochondritis dessicans of the talus in a 26-year-old woman. BMJ Case Reports 2009; doi:10.1136/bcr.06.2008.0091 [Citation ends].
[Figure caption and citation for the preceding image starts]: Sagittal magnetic resonance image (MRI) of the talus, showing an osteochondral lesion on the posterior aspect of the talar domeGupta RK, Kansay R, Aggarwal V, et al. Osteochondritis dessicans of the talus in a 26-year-old woman. BMJ Case Reports 2009; doi:10.1136/bcr.06.2008.0091 [Citation ends].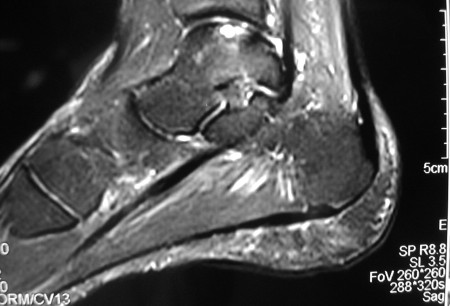 Comparisons of arthroscopic and MRI findings have been used to classify osteochondritis dissecans severity, and thus predict the stability of the osteochondritis dissecans fragment.[28][29]
Comparisons of arthroscopic and MRI findings have been used to classify osteochondritis dissecans severity, and thus predict the stability of the osteochondritis dissecans fragment.[28][29]
Stage I
Arthroscopic finding: irregularity and softening of cartilage. No fissure. No definable fragment.
MRI finding: No break, but thickening in articular cartilage.
Stage II
Arthroscopic finding: articular cartilage breached but not displaceable.
MRI finding: articular cartilage breached, low signal rim behind fragment indicating fibrous attachment.
Stage III
Arthroscopic finding: definable fragment, displaceable, but still attached partially by some cartilage (i.e., a flap lesion).
MRI finding: articular cartilage breached with high T2 signal changes behind fragment suggesting fluid behind the lesion.
Stage IV
Arthroscopic finding: loose body and defect of the articular surface.
MRI finding: loose body with defect of articular surface.
The accuracy of MRI for staging the osteochondritis dissecans lesion can be improved from 45% to 85% by interpreting the high signal T2 line (stage III) as a predictor of instability only when it is accompanied by a breach in the cartilage on the T1-weighted image.[30][Figure caption and citation for the preceding image starts]: Preoperative anteroposterior magnetic resonance imaging (MRI)From the collection of H. Chambers, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Preoperative lateral magnetic resonance imaging (MRI) with no articular cartilage involvementFrom the collection of H. Chambers, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Preoperative lateral magnetic resonance imaging (MRI) with no articular cartilage involvementFrom the collection of H. Chambers, MD [Citation ends].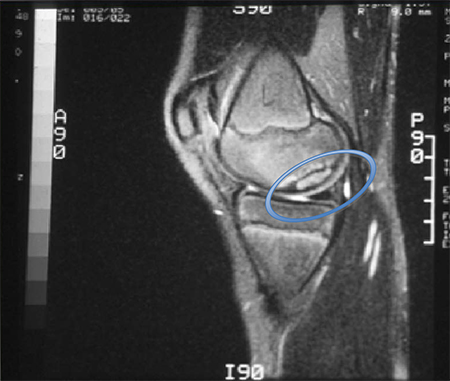
MR arthrogram
Can provide additional information regarding the articular surface. Intra-articular administration of contrast can be performed in the absence of a large joint effusion. This can aid the accuracy of MRI to diagnose subtle chondral defects and to determine the stability of the osteochondral lesion. Intravenous administration of gadolinium, which is then secreted by the synovium, improves visualisation of bony oedema and osteochondral lesions.[31][32] MR arthrogram is particularly helpful in the elbow, as cartilaginous loose bodies can be identified.
Diagnostic arthroscopy
Remains the most specific and sensitive test, but as an invasive procedure, its role in initial diagnosis should be limited because of the availability of advanced non-invasive imaging techniques.
Use of this content is subject to our disclaimer