Approach
Symptoms and signs of joint dislocation include pain, swelling, characteristic posturing, and the inability to move.
Diagnosis is usually confirmed with plain x-rays.
History
Any patient presenting after a traumatic injury complaining of shoulder, finger, knee, elbow, or hip pain, accompanied by painful or incomplete range of motion or characteristic posturing, needs prompt work-up with appropriate imaging.
Physical examination
Shoulder dislocation
Patients commonly present with an arm in a characteristic position of external rotation and slight abduction. They usually have significant pain when attempting motion and are apprehensive about moving the affected joint.
Fullness anteroinferior to the coracoid process is palpable.[54]
A thorough neurological examination is essential to document function of the radial, ulnar, axillary, and median nerves prior to any reduction, and the patency of the axillary artery must be confirmed by the presence of symmetrical radial pulses.[54]
Radial nerve function is assessed by having the patient demonstrate thumb, finger, and wrist extension, along with intact sensation over the dorsum of the hand.
Ulnar nerve function is assessed by having the patient demonstrate active finger abduction and intact sensation over the medial border of the hand including the small finger and ulnar border of the ring finger.
Median nerve function is assessed by having the patient demonstrate finger flexion, the OK sign, and intact sensation over the palm and thenar eminence.
Axillary nerve motor function is difficult to assess secondary to pain and swelling, but intact sensation over the deltoid indicates some function of the nerve.
While most common shoulder dislocations are anterior (>95%), posterior dislocations do occur (2% to 4%), often following electrocution or seizure, and present with the arm held in adduction and internal rotation; they will also be unable to externally rotate the affected extremity actively or passively.[21][54]
Inferior dislocations (i.e., luxatio erectae) occur in 0.5% of cases, and present with a palpable mass in the axilla and the arm fully abducted over the head, with the inability to adduct the arm.[22] They often occur following accidents involving a high-energy impact such as a motorcycle collision. Inferior dislocations are associated with a high rate of complications such as tendon and ligament injuries, vascular compromise, and neurological damage.
Finger dislocation
Patients often present with varying degrees of oedema and ecchymosis (bruising), and are apprehensive about moving the affected joint.
Care must be taken to document the neurovascular status of the affected finger by confirming the presence of sensation on the radial and ulnar borders of the digit.
Any abrasions or lacerations to the joint should alert the physician to the possibility of an open wound, necessitating consideration of antibiotic coverage and orthopaedic consultation.
Distal finger dislocations are often considered to be sprains and are often missed.[15]
Most dislocations of the proximal interphalangeal, distal interphalangeal, and metacarpophalangeal joints are dorsal; some may be volar (i.e., towards the palm). Volar injuries are often unstable and can be easily missed.[15][55][Figure caption and citation for the preceding image starts]: Dislocated distal phalanx, index finger, left handBobjgalindo, CC BY-SA 4.0, via Wikimedia Commons [Citation ends].

Patellar dislocation
Patients often present with a swollen knee held in flexion and an obvious lateral prominence. However, it is not uncommon for patellar dislocations to reduce spontaneously during transport, leg extension, or examination.
[Figure caption and citation for the preceding image starts]: Patellar dislocation: knee held in partial flexion with a visible mass lateral to the lateral femoral condyleYerimah G et al. BMJ Case Rep. 2013 May 2:2013:bcr2013009832; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Left knee radiograph demonstrating lateral patella dislocationYerimah G, et al. BMJ Case Rep. 2013 May 2:2013:bcr2013009832; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Left knee radiograph demonstrating lateral patella dislocationYerimah G, et al. BMJ Case Rep. 2013 May 2:2013:bcr2013009832; used with permission [Citation ends].
Patellar dislocation is often associated with haemarthrosis (bleeding into joint spaces) and a positive apprehension test. In this test, the patient lies supine on a table with the knee flexed to between 20° and 30° and the quadriceps relaxed. The examiner carefully glides the patella laterally, observing for the apprehension sign (i.e., anxiety and resistance), which denotes a positive test.
Tenderness to palpation over the medial patellar retinaculum indicates a tear of the medial patellofemoral ligament. If pain permits, the physician should also perform a full knee examination to determine concomitant injury to the other ligamentous structures. This may include the anterior/posterior drawer and Lachman's tests to examine the cruciate ligaments, the McMurray's test to evaluate for meniscal tears, and varus and valgus stress testing to evaluate the function of various knee ligaments.
The patient should demonstrate the ability to perform a supine straight leg raise to exclude patellar or quadriceps tendon rupture.[16][32][56][57]
Elbow dislocation
Patients typically present with the elbow held in flexion and have significant pain following any attempt at active or passive movement.
The olecranon is prominent, and there is often a significant amount of soft tissue swelling around the elbow. [Figure caption and citation for the preceding image starts]: Right elbow dislocation: dislocated radial head (a), olecranon (b), and tensed triceps tendon (c) resulting in a skin depression (d) just proximal to the radial headLui TH, et al. BMJ. 2020 Oct 8:371:m3494; used with permission [Citation ends].
A thorough neurological examination is imperative to document function of the radial, ulnar, and median nerves prior to any reduction. The patency of the brachial artery must be confirmed by the presence of symmetrical radial pulses.
Radial nerve function is assessed by having the patient demonstrate thumb, finger, and wrist extension, along with intact sensation over the dorsum of the hand.
Ulnar nerve function is assessed by having the patient demonstrate active finger abduction and intact sensation over the medial border of the hand including the small finger and ulnar border of the ring finger.
Median nerve function is assessed by having the patient demonstrate finger flexion, the OK sign, and intact sensation over the palm and thenar eminence.
Axillary nerve motor function is difficult to assess secondary to pain and swelling, but intact sensation over the deltoid indicates some function of the nerve.
Most elbow dislocations are posterior or posterolateral (80% to 90%), but some can be anterior. In these circumstances the arm is held in extension and will appear shortened relative to the contralateral extremity. A posterior dislocation of the elbow associated with a fracture of the ulnar coronoid process and fracture of the radial head is described as the 'terrible triad'.
Intra-articular dislocations are rare, but when they occur usually require general anaesthesia for closed or open reduction.[58]
Hip dislocation
Hip dislocation is an uncommon event.
The classic appearance of posterior hip dislocation is with the hip in a position of flexion, internal rotation, and adduction.
Sciatic nerve injury may occur with stretching of the nerve over the posteriorly dislocated femoral head. Fragments of bone from a posterior wall fracture can also cause injury to the nerve.
Anterior hip dislocation classically presents with the hip held in external rotation, with mild flexion and abduction.
Anterior hip dislocation can cause injury to the femoral artery, vein, or nerve.
Concomitant injuries are quite common with hip dislocations, and they therefore require thorough evaluation. Ipsilateral knee, patella, and femur fractures are common. Pelvic fractures and spine injuries may also be seen.[4]
Imaging
Shoulder dislocation
The diagnosis can be made on x-rays alone.
An anteroposterior (AP) x-ray view of the shoulder should be taken with internal and external humeral rotation.[59] These should be accompanied by axillary lateral and/or scapular Y views to confirm diagnosis. Each of these x-ray views is 92% sensitive for acute shoulder dislocation.[60] On a scapular Y view, the humeral head lies anteriorly to the Y in anterior dislocations, and posteriorly to the Y in posterior dislocations. In standard AP views, the humeral head rests anteroinferiorly to the coracoid in anterior dislocations. However, in posterior dislocations, the humerus can appear to be reduced. Therefore, axillary or scapular Y views are essential for accurate diagnosis, as up to 79% of posterior shoulder dislocations are initially misdiagnosed. Axillary views can correctly identify posterior dislocations in 100% of patients when combined with AP views of the shoulder.[61][62] An axillary lateral or a modified axillary view known as the Velpeau view may also be used to confirm diagnosis.
A possible fracture of the proximal humerus should be excluded, as attempts at reduction could further displace this fracture.
If a vascular injury is of concern based on the physical examination, an arteriogram may be required.
MRI scans provide excellent visualisation of soft tissue anatomy and may be ordered if any associated injuries (e.g., rotator cuff tears) are suspected.
Point-of-care ultrasound (POCUS) has been suggested as an additional diagnostic tool for shoulder dislocation. It has the potential to reduce time to diagnosis and reduction, as well as radiation exposure and healthcare costs. One systematic review found that POCUS had 100% sensitivity and specificity for the identification of shoulder dislocations and reductions, and 96.8% sensitivity and 99.7% specificity for the detection of associated fractures.[63] However, it is not yet clear exactly when ultrasound is optimal - pre- or post-reduction - and which x-rays it should replace. [Figure caption and citation for the preceding image starts]: Scapular Y x-ray view showing an anterior dislocation of the shoulderPersonal collection of Dr Paul Novakovich [Citation ends].
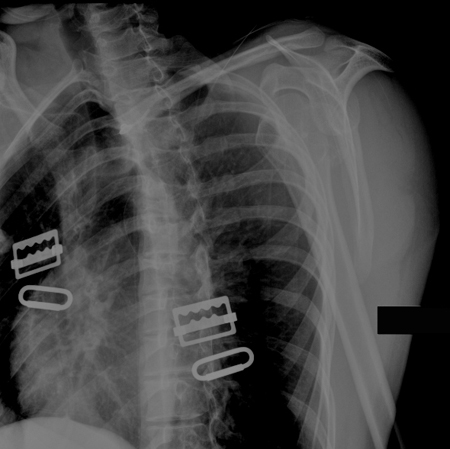 [Figure caption and citation for the preceding image starts]: Scapular Y x-ray view showing an anterior fracture dislocation of the shoulder and fracture of the greater tuberosityPersonal collection of Dr Paul Novakovich [Citation ends].
[Figure caption and citation for the preceding image starts]: Scapular Y x-ray view showing an anterior fracture dislocation of the shoulder and fracture of the greater tuberosityPersonal collection of Dr Paul Novakovich [Citation ends]. [Figure caption and citation for the preceding image starts]: Anteroposterior x-ray view of a shoulder showing an anteroinferior dislocationPersonal collection of Dr Paul Novakovich [Citation ends].
[Figure caption and citation for the preceding image starts]: Anteroposterior x-ray view of a shoulder showing an anteroinferior dislocationPersonal collection of Dr Paul Novakovich [Citation ends]. [Figure caption and citation for the preceding image starts]: Anteroposterior x-ray view of a shoulder showing a missed posterior dislocation: the glenohumeral joint appears reducedPersonal collection of Dr Paul Novakovich [Citation ends].
[Figure caption and citation for the preceding image starts]: Anteroposterior x-ray view of a shoulder showing a missed posterior dislocation: the glenohumeral joint appears reducedPersonal collection of Dr Paul Novakovich [Citation ends]. [Figure caption and citation for the preceding image starts]: Axillary lateral of a shoulder with a missed posterior dislocation: humeral head clearly is not reduced and is locked on the posterior rim of the glenoidPersonal collection of Dr Paul Novakovich [Citation ends].
[Figure caption and citation for the preceding image starts]: Axillary lateral of a shoulder with a missed posterior dislocation: humeral head clearly is not reduced and is locked on the posterior rim of the glenoidPersonal collection of Dr Paul Novakovich [Citation ends].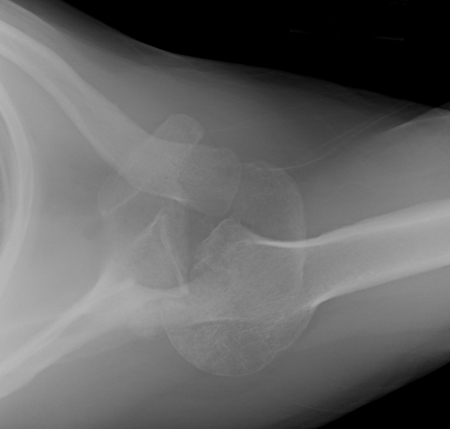
Finger dislocation
Clinical suspicion is based on the history and physical examination and may warrant plain film imaging of the hand or individual finger.
AP, oblique, and lateral views of the affected joint are mandatory in evaluating a patient with a hand injury to exclude fracture and/or dislocation.
These x-rays should be closely inspected for associated fractures and avulsions, which may indicate ligament or tendon damage.
Further imaging is usually not necessary in the acute management of simple dislocations. [Figure caption and citation for the preceding image starts]: X-ray showing dislocation of the proximal interphalangeal joint, left index fingerHellerhoff, CC BY-SA 3.0 via Wikimedia Commons [Citation ends].

Patellar dislocation
Clinical suspicion is based on the history, and physical examination warrants AP and lateral x-ray views of the knee. However, it is not uncommon for patellar dislocations to reduce spontaneously during examination or following leg extension.
Dislocation can be confirmed on a Merchant or sunrise (infra-patellar) view, which should demonstrate the medial facet of the patella resting on the lateral trochlea of the femur.
Images should be inspected closely for evidence of osteochondral lesions.
CT scans are not necessary unless adequate x-rays cannot be obtained or are inconclusive.
MRI scans of the knee joint can be useful in determining associated ligament injuries or osteochondral lesions but are not necessary to confirm an acute patellar dislocation.[57][Figure caption and citation for the preceding image starts]: Left knee radiograph demonstrating lateral patella dislocationYerimah G, et al. BMJ Case Rep. 2013 May 2:2013:bcr2013009832; used with permission [Citation ends].

Elbow dislocation
Clinical suspicion is based on the history; physical examination should prompt radiographic imaging of the elbow.
Most elbow dislocations are posterior or posterolateral (80% to 90%). Standard AP and lateral x-ray views of the elbow joint are the initial radiographic study of choice. In a posterior dislocation, these show the radius and ulna lying posterior to the distal humerus.
The radial head should always be in line with the capitellum, and the olecranon should rest in the trochlea on a standard lateral view.
In addition, AP and lateral x-ray views of the forearm are necessary to exclude associated forearm fractures (e.g., Monteggia fracture).
A radial head/capitellum view may be used to discern radial head and coronoid fractures. Radial head fractures and coronoid fractures can be difficult to discern on plain x-rays but are readily apparent on a non-contrast CT scan of the elbow.[44]
Further imaging to exclude other extremity injuries may be required and should be based on a thorough physical examination. [Figure caption and citation for the preceding image starts]: Anteroposterior x-ray view of an elbow dislocationPersonal collection of Dr Paul Novakovich [Citation ends].
 [Figure caption and citation for the preceding image starts]: Lateral x-ray view of a posterolateral elbow dislocationPersonal collection of Dr Paul Novakovich [Citation ends].
[Figure caption and citation for the preceding image starts]: Lateral x-ray view of a posterolateral elbow dislocationPersonal collection of Dr Paul Novakovich [Citation ends].
Hip dislocation
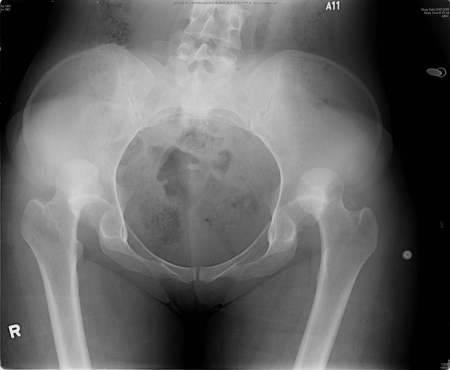
Pelvic x-rays (Judet views, and inlet and outlet views) are routinely obtained to assess for possible concomitant fractures to the pelvis.
A CT scan of the pelvis can identify specific fracture patterns, as well as smaller bony lesions (loose bodies) that may prevent a closed reduction and mandate an open reduction in the operating room.[4][Figure caption and citation for the preceding image starts]: X-ray showing bilateral hip posterior dislocationFan KY, et al. BMJ Case Rep. 2015 Mar 25:2015:bcr2014204031; used with permission [Citation ends].
Use of this content is subject to our disclaimer