Screening for peripheral neuropathy
Screening for peripheral neuropathy should be undertaken in patients with:[1]Pop-Busui R, Boulton AJ, Feldman EL, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care. 2017 Jan;40(1):136-54.
https://diabetesjournals.org/care/article/40/1/136/37160/Diabetic-Neuropathy-A-Position-Statement-by-the
http://www.ncbi.nlm.nih.gov/pubmed/27999003?tool=bestpractice.com
[39]American Diabetes Association Professional Practice Committee. Introduction and methodology: standards of care in diabetes-2025. Diabetes Care. 2025 Jan 1;48(1 suppl 1):S1-5.
https://diabetesjournals.org/care/article/48/Supplement_1/S1/157562/Introduction-and-Methodology-Standards-of-Care-in
http://www.ncbi.nlm.nih.gov/pubmed/39651982?tool=bestpractice.com
Type 2 diabetes, from diagnosis
Type 1 diabetes, 5 years after diagnosis
Metabolic syndrome or impaired glucose tolerance with symptoms of peripheral neuropathy.
Screening is conducted at least annually thereafter, using symptoms and signs. Assessment for distal symmetric polyneuropathy should include a careful history and assessment of either temperature or pinprick sensation (small-fibre function) and vibration sensation using a 128-Hz tuning fork (for large-fibre function). All people with diabetes should have annual 10-g monofilament testing to identify feet at risk for ulceration and amputation. Foot evaluation should also include vascular assessment and inspection of the skin. Note that patients with evidence of sensory loss or prior ulceration or amputation should have their feet inspected at every visit.[39]American Diabetes Association Professional Practice Committee. Introduction and methodology: standards of care in diabetes-2025. Diabetes Care. 2025 Jan 1;48(1 suppl 1):S1-5.
https://diabetesjournals.org/care/article/48/Supplement_1/S1/157562/Introduction-and-Methodology-Standards-of-Care-in
http://www.ncbi.nlm.nih.gov/pubmed/39651982?tool=bestpractice.com
The Michigan Neuropathy Screening Instrument (MNSI) and similar symptom scoring systems are useful in clinical research.[114]Feldman EL, Stevens MJ, Thomas PK, et al. A practical two-step quantitative clinical and electrophysiological assessment for the diagnosis and staging of diabetic neuropathy. Diabetes Care. 1994 Nov;17(11):1281-9.
http://www.ncbi.nlm.nih.gov/pubmed/7821168?tool=bestpractice.com
[115]Young MJ, Adams JE, Anderson GF, et al. Medial arterial calcification in the feet of diabetic patients and matched non-diabetic control subjects. Diabetologia. 1993 Jul;36(7):615-21.
http://www.ncbi.nlm.nih.gov/pubmed/8359578?tool=bestpractice.com
[116]Cabezas-Cerrato J. The prevalence of clinical diabetic polyneuropathy in Spain: a study in primary care and hospital clinic groups. Neuropathy Spanish Study Group of the Spanish Diabetes Society (SDS). Diabetologia. 1998 Nov;41(11):1263-9.
http://www.ncbi.nlm.nih.gov/pubmed/9833931?tool=bestpractice.com
[117]Herman WH, Pop-Busui R, Braffett BH, et al; DCCT/EDIC Research Group. Use of the Michigan Neuropathy Screening Instrument as a measure of distal symmetrical peripheral neuropathy in Type 1 diabetes: results from the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications. Diabet Med. 2012 Jul;29(7):937-44.
http://www.ncbi.nlm.nih.gov/pubmed/22417277?tool=bestpractice.com
Electrophysiological testing or referral to a neurologist is rarely needed, except in situations where diagnosis is unclear or the clinical features are atypical:[1]Pop-Busui R, Boulton AJ, Feldman EL, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care. 2017 Jan;40(1):136-54.
https://diabetesjournals.org/care/article/40/1/136/37160/Diabetic-Neuropathy-A-Position-Statement-by-the
http://www.ncbi.nlm.nih.gov/pubmed/27999003?tool=bestpractice.com
[39]American Diabetes Association Professional Practice Committee. Introduction and methodology: standards of care in diabetes-2025. Diabetes Care. 2025 Jan 1;48(1 suppl 1):S1-5.
https://diabetesjournals.org/care/article/48/Supplement_1/S1/157562/Introduction-and-Methodology-Standards-of-Care-in
http://www.ncbi.nlm.nih.gov/pubmed/39651982?tool=bestpractice.com
Motor deficits greater than sensory deficits
Marked asymmetry of the neurological deficits
Initial symptoms in the upper extremities
Rapid progression.
Screening for autonomic neuropathy
The American Diabetes Association (ADA) recommends that clinicians assess symptoms and signs of autonomic neuropathy in people with diabetes starting at diagnosis of type 2 diabetes and 5 years after the diagnosis of type 1 diabetes, and at least annually thereafter and with evidence of other microvascular complications, particularly kidney disease and diabetic peripheral neuropathy. Screening can include asking about orthostatic dizziness, syncope, or dry cracked skin in the extremities. Signs of autonomic neuropathy include orthostatic hypotension, a resting tachycardia, or evidence of peripheral dryness or cracking of skin.[39]American Diabetes Association Professional Practice Committee. Introduction and methodology: standards of care in diabetes-2025. Diabetes Care. 2025 Jan 1;48(1 suppl 1):S1-5.
https://diabetesjournals.org/care/article/48/Supplement_1/S1/157562/Introduction-and-Methodology-Standards-of-Care-in
http://www.ncbi.nlm.nih.gov/pubmed/39651982?tool=bestpractice.com
In practice, further testing may not be needed, as it may not affect management or outcome. However, according to the ADA, further testing can be considered if symptoms are present and will depend on the end organ involved but might include cardiovascular autonomic testing, sweat testing, urodynamic studies, gastric emptying, or endoscopy/colonoscopy.[39]American Diabetes Association Professional Practice Committee. Introduction and methodology: standards of care in diabetes-2025. Diabetes Care. 2025 Jan 1;48(1 suppl 1):S1-5.
https://diabetesjournals.org/care/article/48/Supplement_1/S1/157562/Introduction-and-Methodology-Standards-of-Care-in
http://www.ncbi.nlm.nih.gov/pubmed/39651982?tool=bestpractice.com
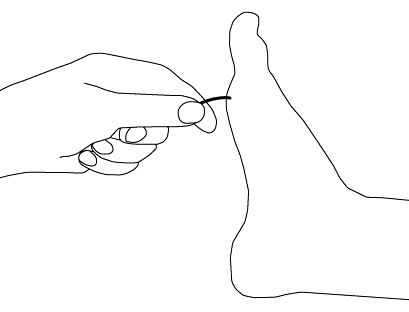
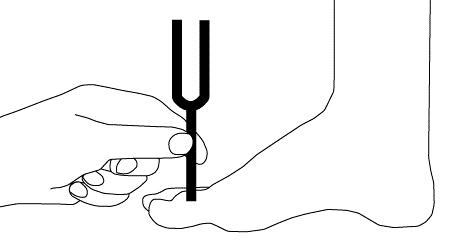
[Figure caption and citation for the preceding image starts]: Vibratory testingCreated by the BMJ Group [Citation ends].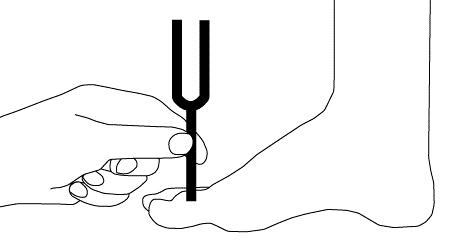 [Figure caption and citation for the preceding image starts]: Light touch testing with monofilamentCreated by the BMJ Group [Citation ends].
[Figure caption and citation for the preceding image starts]: Light touch testing with monofilamentCreated by the BMJ Group [Citation ends].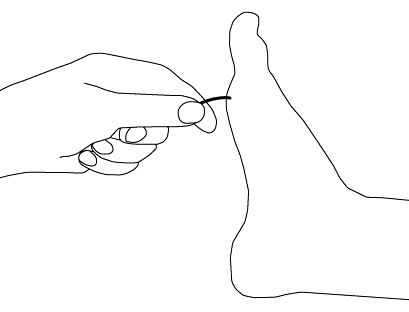
 [Figure caption and citation for the preceding image starts]: Light touch testing with monofilamentCreated by the BMJ Group [Citation ends].
[Figure caption and citation for the preceding image starts]: Light touch testing with monofilamentCreated by the BMJ Group [Citation ends].