Investigations
1st investigations to order
clinical diagnosis
Test
Routine screening tests may exclude other common conditions.
Result
diagnosis of peripheral neuropathy is often made on clinical grounds
fasting blood glucose
Test
Many patients who present with painful neuropathy may have diabetes without knowing it. In this circumstance, a fasting blood glucose may be performed.
The American Diabetes Association recommends any of four screening tests to diagnose diabetes: fasting blood glucose, random plasma glucose, HbA1c, or 2-hour post-load glucose after 75 g oral glucose. Random plasma glucose is typically reserved for those with classic symptoms of hyperglycaemia or a hyperglycaemic crisis.[39] In the absence of unequivocal hyperglycaemia, diagnosis requires two abnormal test results.[39]
Result
diagnosis of diabetes mellitus (if not already known to be present)
HbA1c
Test
Many patients who present with painful neuropathy may have diabetes without knowing it. In this circumstance, HbA1c may be performed.
The American Diabetes Association recommends any of four screening tests to diagnose diabetes: fasting blood glucose, random plasma glucose, HbA1c, or 2-hour post-load glucose after 75 g oral glucose.[39] In the absence of unequivocal hyperglycaemia, diagnosis requires two abnormal test results.[39]
Poorly controlled hyperglycaemia is associated with increased risk of neuropathy.[39]
Result
correlates with degree of glycaemic control
serum thyroid-stimulating hormone
Test
To exclude thyroid dysfunction.
Result
normal
serum vitamin B12
Test
To exclude deficiency.
Result
normal
renal function tests
Test
Renal function tests are recommended to exclude renal disease as a treatable cause of neuropathy.
Additionally, all patients with diabetes receive regular monitoring of renal function.
Evaluation includes electrolytes, urea, creatinine, urinary microalbumin, and measurement of estimated glomerular filtration rate.
Result
normal or may show renal insufficiency
serum lipid profile
Test
To exclude abnormalities in low-density lipoprotein, high-density lipoprotein, triglycerides, and total cholesterol.
Result
may show lipid abnormalities
LFTs
Test
To exclude hepatic disease.
Result
normal
FBC and erythrocyte sedimentation rate
Test
To exclude anaemia and inflammatory disorders.
Result
normal
serum/urine immunoelectrophoresis
Test
To exclude multiple myeloma.
Result
normal
Investigations to consider
2-hour plasma glucose
Test
Many patients who present with painful neuropathy may have diabetes without knowing it. In this circumstance, plasma glucose may be measured 2 hours after a 75 g oral glucose load.
Patients should be advised to consume a varied diet with at least 150 g of carbohydrate on the 3 days prior to testing, as fasting and carbohydrate restriction can falsely increase plasma glucose levels.[39]
The American Diabetes Association recommends any of four screening tests to diagnose diabetes: fasting blood glucose, random plasma glucose, HbA1c, or 2-hour post-load glucose after 75 g oral glucose.[39] In the absence of unequivocal hyperglycaemia, diagnosis requires two abnormal test results.[39]
Result
diagnosis of diabetes mellitus (if not already known to be present)
nerve conduction studies (nerve conduction velocity [NCV])
Test
Indicated in situations where the clinical features are atypical (such as asymmetrical symptoms and signs or weakness).
Whole nerve electrophysiological procedures (e.g., NCV, F-waves, sensory, and/or motor amplitudes) are performed.[Figure caption and citation for the preceding image starts]: Nerve conduction testing of the lower legCreated by the BMJ Group [Citation ends].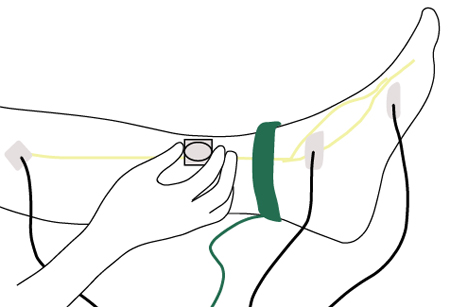
In very mild or asymptomatic cases, the only change may be distal slowing of conduction or none.
As the neuropathy progressively worsens, findings of axonal degeneration predominate, including decreased amplitude of sensory nerve action potentials (SNAPs); decreased amplitude of compound muscle action potentials; relative preservation of proximal conduction velocities; and evidence of fibrillation potentials.
NCV is usually gradually diminished by DN.[106] However, it may be completely normal in patients with predominantly small-fibre neuropathy. Several prospective clinical trials describe slower worsening of NCV end points in the current standard of care for patients with diabetes.[10][107]
Longitudinal studies suggest an average loss of SNAP amplitude at a rate of approximately 5% per year over a 10-year period.[106] In patients with type 1 diabetes participating in the Epidemiology of Diabetes Interventions and Complications (EDIC) study, the average loss rate was around 3% per year over a 13-14-year period.[10]
Motor nerve studies may demonstrate some slowing, even when patients have no symptoms or signs of neuropathy, with a greater slowing in symptomatic patients.
Motor amplitudes may be decreased in more advanced DN.
A key role for electrophysiological assessment is to rule out other causes of neuropathy (e.g., unilateral conditions, such as entrapments) and to identify neuropathies superimposed on DN.
Result
reduced sensory nerve conduction velocity and decreased amplitude is the most sensitive and earliest result among the NCV studies
electromyography (EMG)
Test
Indicated in situations where the clinical features are atypical (such as asymmetrical symptoms and signs, or weakness).
Result
may be normal in mild or neurologically asymptomatic patients, but demonstrates denervation in more severe DN
quantitative sensory testing (QST)
Test
Focuses on the vibration perception threshold (VPT) and thermal perception threshold.
Used in people with diabetes, in addition to routine clinical examination, as a subsequent assessment of loss of protective sensation and axonal pathology when all the other examinations are normal to detect small-fibre neuropathy.[86]
A high sensitivity and specificity for VPT has been confirmed in patients with type 1 diabetes relative to NCV and neurological evaluation.
Probably more reproducible than the subjective assessment by the patient of the strength of stimulus.[86]
There is a documented relationship between elevated VPT tested in the 50-300 Hz range and DN.[106]
Abnormal thermal thresholds have been reported in 75% of patients with moderate to severe diabetic peripheral neuropathy, and elevated heat pain thresholds were detected in 39% of these patients.[106]
Generally, there is a high correlation between elevated thermal and vibration thresholds, but these measures can be dissociated, suggesting a predominant small or large fibre neuropathy in individual patients.
Result
may be normal, or deficits in vibration and/or thermal perception threshold may be detected
skin biopsy
Test
A validated technique for determining intra-epidermal nerve fibre density. May be considered for the diagnosis of DN, particularly small-fibre neuropathy, when electrophysiology does not match clinical presentation.[82]
Result
may be normal or show abnormalities of intra-epidermal nerve fibre density
cardiovascular reflex testing
Test
Includes ECG recordings of respiratory rate (RR) at rest and several standard clinical challenges.
The following are the ideal standard tests for clinical autonomic testing: heart rate response to deep breathing, standing, and Valsalva manoeuvre; and BP response to standing.[68][69][88]
HR response to deep breathing is measured while the patient is supine and then resting, breathing at 6 breaths per minute. The value of expiration-to-inspiration ratio of the RR interval varies with age but is decreased compared with normal for the specific age band.
Various mathematical calculations may be used but age-adjusted normative ranges are strictly required for the interpretation of these tests.
The Valsalva manoeuvre is not advisable in the presence of proliferative retinopathy and when there is an increased risk of retinal haemorrhage.
Heart rate response to standing is measured by continuous ECG monitoring. The RR interval is measured at 15 and 30 beats after standing.
These tests mainly demonstrate impaired parasympathetic tone in people with cardiovascular autonomic neuropathy.
Result
may be impaired heart rate response to deep breathing, Valsalva manoeuvre, and/or standing
corneal confocal microscopy
Test
A non-invasive ophthalmic technique to image the corneal sub-basal nerve plexus. It has been shown to detect small sensory corneal nerve fibre loss in DN.[108][109][110] Studies have found high reproducibility, sensitivity, and specificity.[108][110] One systematic review and meta-analysis confirmed that corneal confocal microscopy can detect both early sub-clinical and established DN.[111]
Result
corneal nerve fibre damage correlates with intra-epidermal nerve fibre loss and severity of neuropathy
heart rate variability (HRV)
Test
HRV can be assessed either by calculating indices based on statistical analysis of respiratory rate intervals (time-domain analysis) or by spectral analysis (frequency-domain analysis) of an array.[68][69][70][88]
QT prolongation is an independent predictor of death in diabetic patients and is weakly associated with measures of HRV.[89][112]
Result
may be abnormal; QT prolongation may be present
gastric emptying studies
Test
Performed with double isotope scintigraphy.
Indicated in people who have symptoms and/or signs suggesting diabetic gastroparesis when the diagnosis is still in doubt.
Result
delayed solid phase emptying
gastroduodenoscopy
Test
Recommended along with other gastrointestinal investigations (e.g., gastric emptying studies or gastric electrography) to exclude pyloric or other mechanical obstructions in people with suspected diabetic gastroparesis when the diagnosis is in doubt.
Result
may be normal or may demonstrate solid food residues
barium meal
Test
Barium meal has a place in evaluating mucosal lesions or obstruction.
Result
excludes mucosal lesions or obstruction
gastrointestinal manometry
Test
Manometry should be considered as a research technique to investigate gastric and intestinal motility.
Result
may indicate delay in gastric and intestinal motility
hydrogen breath tests
Test
Diarrhoea is evident in 20% of patients with diabetes, particularly those with known autonomic dysfunction.[67]
Diarrhoea in patients with diabetes is often due to bacterial overgrowth, which can be diagnosed with hydrogen breath tests.
Using non-radioactive 13C-acetate or -octanoic acid as a label; these are safe, inexpensive tests that correlate well with scintigraphy results.
Result
may be normal or may suggest bacterial overgrowth
gastric ultrasonography
Test
A non-invasive diagnostic method.
Two-dimensional ultrasound has been validated for measuring emptying of liquids and semi-solids. However, 3-dimensional ultrasound offers a more comprehensive imaging of the total stomach.
Result
may demonstrate delayed gastric emptying
gastric MRI
Test
Has been used to measure gastric emptying and motility with excellent reproducibility, but its use is limited to research purposes.
Result
may demonstrate delayed gastric emptying
anorectal manometry
Test
Indicated for evaluating sphincter tone and the rectal-anal-inhibitory reflex.
Distinguishes colonic hypomotility from rectosigmoid dysfunction causing outlet obstructive symptoms.
Result
may be normal or may suggest hypomotility
faecal fat
Test
For patients with large-volume diarrhoea, faecal fat should be checked and further studied with a 72-hour collection to rule out malabsorptive disorders.
If significant steatorrhoea, pancreatic function tests should be performed.
If coeliac disease is suspected (e.g., anaemia, chronic diarrhoea, distended abdomen, young age, history of type 1 diabetes), serum levels of coeliac disease antibody profile, including anti-transglutaminase and endomysial, are measured.
Result
may be normal or elevated (steatorrhoea)
d-xylose test
Test
Alternative or additional test to the faecal fat measurement that can be used to rule out malabsorptive disorders in people with large-volume diarrhoea.
Result
normal
urine culture
Test
Part of the assessment of people with symptoms of bladder dysfunction.
Result
normal
cystometry, voiding cystometrogram
Test
Used in addition to post-void urinary tract ultrasound to evaluate diabetic bladder dysfunction.
Residual volume and upper urinary tract dilation are assessed.
Result
may be normal or may suggest bladder dysfunction
post-void urinary tract ultrasound
Test
Used in addition to cystometry and voiding cystogram to evaluate diabetic bladder dysfunction.
Residual volume and upper urinary tract dilation are assessed.
Result
may be normal or may suggest bladder dysfunction
video-urodynamics
Test
The preferred investigation for invasive urodynamics in patients with neurogenic lower urinary tract dysfunction.[91]
Result
may be normal or may suggest bladder dysfunction
Testosterone (morning)
Test
Indicated in men with erectile dysfunction to rule out hypogonadism.[39]
Serum testosterone should be a morning sample.
Further specialised testing may also be necessary. See Erectile dysfunction.
Result
normal
Use of this content is subject to our disclaimer