Approach
The presence of a lens opacity or cataract on its own is not an indication for intervention. Treatment is indicated if:
The cataract is causing other ocular diseases
Opacification is sufficiently dense to cause functional impairment of the patient's vision, despite best-spectacle correction, and surgery is reasonably likely to improve quality of life
The fundus cannot otherwise be visualised in the setting of active posterior segment disease or planned posterior segment surgery.
Cataract surgery is the most effective intervention for cataracts. In one systematic review of systematic reviews, cataract surgery was consistently associated with improved vision-related quality of life, particularly if carried out immediately after diagnosis.[39]
Patient referral and initial measures
It should be stressed that the presence of a cataract in most circumstances does not affect the health of the eye. A patient should be referred to an ophthalmologist if cataract is the suspected diagnosis.[40]
Initial measures include optimisation of the patient’s refractive correction with glasses or contact lenses. In some cases, this may delay the patient’s need for surgery. Additional interventions to improve visual function include use of tinted lenses, increased illumination, and magnifiers. Currently, there are no pharmacological treatments known to eliminate existing cataracts or stop their progression.[35][40]
The decision to proceed to surgery is patient-specific and cannot be generalised to the population as a whole. Cataract surgery may increase the risk of progression of underlying wet age-related macular degeneration (AMD) and thus have deleterious effects on vision.[41][42] However, reliable conclusions cannot be drawn from the available data to determine whether cataract surgery is beneficial or harmful in people with cataracts and AMD, and decisions must be based on best clinical judgement.[43]
Cataract alone: without functional impairment of vision
No treatment is required in this group of patients. Annual eye examination is recommended to follow the progress of the lenticular opacity, and to detect the presence of functional visual complaint.
Cataract alone: with functional impairment of vision
In patients with both cataract and impaired vision, the obligation before embarking on cataract surgery is to ensure that vision loss is:
Sufficiently severe to result in a functional deficit
Due to the cataract and not some other ocular or neurological condition.
To proceed with treatment, the decrease in vision should affect the patient's ability to perform activities of daily living, and should interfere with the quality of the patient's life. A history will reveal the functional deficit (e.g., problems seeing street signs while driving, difficulty with glare, halos, and star-bursts from oncoming headlights making it difficult for the patient to drive at night). Most commonly, a best-corrected visual acuity of 20/40 or worse will result in difficulties sufficient to justify surgery, although each case must be individualised to the patient's lifestyle and visual needs. Vision of 20/40 is often required to pass driver's licence examinations in most states in the US. Decreased visual acuity can increase a patient's risk of fall, and may lead to greater morbidity in older people.
It is important to perform a complete ocular examination to rule out any other cause of decreased vision other than cataract.[44] If another cause is detected, it is necessary to determine that the cataract is resulting in sufficient vision loss so as to justify cataract surgery.
Preparing for cataract surgery
Clinical assessment should include eye examination, biometry and intra-ocular lens (IOL) selection, consent for one or both eyes, and any preoperative anaesthetic or medical health assessment that has not already been completed remotely (e.g., blood pressure check).[45]
Assess axial length, curvature and clarity of the cornea, refractive error, red reflex, and dilation size, lens stability and density, retinal health, and fellow eye status.[46] Additional checks include presence or absence of synechiae (adhesion of the iris to the cornea or lens), refractive error in the fellow eye (in terms of prevention of anisometropia), presence or absence of crystalline lens movement particularly in association with pseudo-exfoliation material on the iris or lens, and/or zonular weakness.[47] Pre-existing problems with the corneal endothelium, such as Fuchs dystrophy (in which there is a progressive loss of corneal endothelial cells), may increase the risk of postoperative corneal oedema.[48]
Ask the patient if they are taking an alpha-blocker (e.g., tamsulosin), as this is a risk factor for intraoperative floppy iris syndrome.[49][50][51] Preoperatively, if the patient is a contact lens wearer or has had prior refractive surgery or corneal scars, then additional biometry calculations need to be made to account for this. It is important to assess best visual potential before commencing cataract surgery. This may involve pinhole acuity potential, potential acuity meter, or a macular optical coherence tomography imaging test.
Preoperative medical ancillary testing prior to cataract surgery is recommended only if indicated by the patient’s medical condition and the physician’s assessment.[52] Preoperative testing for comorbid medical conditions in patients about to undergo cataract surgery does not reduce the risk of adverse events perioperatively or postoperatively.[53]
[  ]
Nonetheless, adverse medical events precipitated by cataract surgery remain a concern, because of the large number of older patients with multiple medical comorbidities who have cataract surgery.[53]
]
Nonetheless, adverse medical events precipitated by cataract surgery remain a concern, because of the large number of older patients with multiple medical comorbidities who have cataract surgery.[53]
Consider anaesthetic requirements
Surgery for cataract is generally performed in an outpatient setting under local anaesthesia or topical anaesthesia alone.[54]
[  ]
One Cochrane systematic review of 13 trials including 2388 eyes found moderate-quality evidence that intracameral lidocaine in addition to topical anaesthesia reduced intraoperative pain compared with topical anaesthesia alone, although pain scores were low with both methods. No additional benefit was found for postoperative pain.[55]
]
One Cochrane systematic review of 13 trials including 2388 eyes found moderate-quality evidence that intracameral lidocaine in addition to topical anaesthesia reduced intraoperative pain compared with topical anaesthesia alone, although pain scores were low with both methods. No additional benefit was found for postoperative pain.[55]
Opioids are commonly used to increase pain relief during phacoemulsification and postoperatively. A further option is the use of ketorolac, a non-steroidal anti-inflammatory drug (NSAID), which is available in combination with phenylephrine, the mydriatic agent, as an addition to irrigation solution to reduce postoperative pain and the number of patients requiring analgesia.[56] In specific complex cataract cases or in patients with comorbidities, other anaesthetic methods may be added, such as sub-Tenon’s anaesthesia, peribulbar block, or general anaesthesia.[57]
Surgical procedure
Routine surgery usually requires about 5 to 15 minutes of intraoperative time; longer operating times are required for more complex procedures (e.g., no view, poor dilation, weak zonules) and/or management of perioperative complications. Phacoemulsification is commonly employed to extract the cataract through a small surgical excision (typically 1.8-2.8 mm). This approach uses a rapidly vibrating (ultrasonic) tip combined in a single hand-piece co-axially (or separated bi-axially), with both irrigation inflow and aspiration outflow to maintain the pressures within the eye and to flush out the fragmented cataract.
In the vast majority of surgeries performed in developed countries, an artificial IOL is implanted within the eye to restore the optical converging power lost with the removal of the cataractous crystalline lens.[35] The power of the IOL is calculated from preoperative or intraoperative measurements of the corneal curvature and the axial length of the eye. The refractive target for the IOL is normally emmetropia. However, this should be adjusted for each individual patient; for example, those with lifelong hyperopia may prefer exactly plano (20/20) while those with lifelong myopia may prefer a slight myopia. Around 90% of patients having routine surgery achieve ±1 dioptre of target refraction, with higher success rates in patients without pre-existing ocular pathology or prior intra-ocular surgery.[58][59]
Monofocal IOLs
In general, the implanted lens is a monofocal optically spherical (simple convex) lens set to correct distance vision. Any remaining refractive error following cataract surgery is corrected either by spectacles or by contact lenses fitted postoperatively after typically waiting at least 1 month for healing.
Toric IOLs
These lenses have a built-in astigmatic correction and are used in patients with corneal regular astigmatic refractive errors as determined by topography. Toric IOLs are implanted in a specific orientation aligning the astigmatic axis of the IOL with the patient's steep axis, with the goal being to reduce the patient's postoperative spectacle dependence at a single focal length. Marking of the correct axis and measurements of corneal topography have undergone significant improvements, including new imaging tools and overlay iris tracking devices during surgery, to ensure power accuracy and to minimise the effect of ocular cyclotorsion when the patient lies flat for surgery.
One Cochrane systematic review of 10 studies of 626 eyes concluded that toric IOLs are more likely to achieve astigmatism within 0.5 dioptre after cataract surgery compared with limbal relaxing incisions (LRIs; circumferential incisions made at the limbus at each end of the steep meridian).[60]
[  ]
[Evidence B] This is likely due to the nomogram variation of incision length and depth, and the drift of LRI effect over time. Using image-guided marking methods improves toric IOL alignment accuracy compared with using manual marking methods, resulting in less axis misalignment, a smaller difference vector, and less postoperative astigmatism.[61]
]
[Evidence B] This is likely due to the nomogram variation of incision length and depth, and the drift of LRI effect over time. Using image-guided marking methods improves toric IOL alignment accuracy compared with using manual marking methods, resulting in less axis misalignment, a smaller difference vector, and less postoperative astigmatism.[61]
Multi-focal and accommodating IOLs
Standard and toric IOLs correct the patient's vision at one distance only (e.g., near, intermediate [corresponding to driving, reading, or computer visual tasks], or distant).
Multi-focal (pseudo-accommodating) or accommodating IOLs provide improved vision at several focal distances, simultaneously targeting good uncorrected distance vision and improved uncorrected near and intermediate vision. Examples included low-add, extended range of correction (depth of focus), multi-focal toric, and light-adjustable IOLs.[62][63][64] The success of multi-focal or accommodating IOLs mostly depends on proper patient selection, particularly concerning the patient’s expectations for spectacle independence.[65]
[  ]
Although many patients report good vision with these IOLs when used for their approved indication, each design has drawbacks (e.g., glare, halos, reduced contrast sensitivity, insufficient near vision).[63][64][66][67][68][69]
]
Although many patients report good vision with these IOLs when used for their approved indication, each design has drawbacks (e.g., glare, halos, reduced contrast sensitivity, insufficient near vision).[63][64][66][67][68][69]
Monovision and mini-monovision
An alternative to multi-focal IOLs, monovision cataract surgery implants a different monofocal IOL in each eye. It generally targets best distance focus in the dominant eye and best close focus in the non-dominant eye. The trade-offs with monovision are the loss of stereo vision and reduced depth perception, which some patients may not tolerate.
Mini-monovision involves a smaller dioptre difference between the eyes compared with traditional monovision. It can achieve spectacle independence without the risk of photic phenomena, and is associated with high patient satisfaction rates.[70][71]
Cataract surgery in low-income settings
In developing countries, cataract surgery may be performed using a larger incision to remove the cataract in one piece. Low-cost IOLs are increasingly available and their use is becoming routine in developing countries. If no IOL is available aphakic glasses are prescribed postoperatively or a secondary IOL may be placed, sutured, or glued in at a later date.
[Figure caption and citation for the preceding image starts]: Foldable intra-ocular lens starting to unfold in the empty lens capsule after insertionAdapted from BMJ (2006), used with permission; copyright 2009 by the BMJ Group [Citation ends].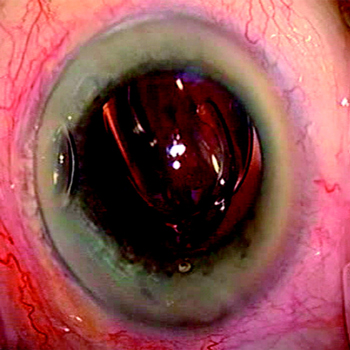
One Cochrane review that compared manual small incision cataract surgery with extracapsular cataract surgery in India and Nepal concluded that there were insufficient data on cost-effectiveness, and that neither procedure was superior to the other.[72]
Correction of residual refractive error
If an implant lens is not used or a refractive error remains (e.g., astigmatism uncorrected by the implant lens), the patient may need to wear contact lenses or spectacles to achieve good postoperative vision.
Adjunctive procedures to correct residual refractive errors can be performed during or after surgery.[73]
Concomitant eye pathology: previous refractive surgery
Patients who have previously undergone refractive surgery may have high expectations of spectacle-free vision after cataract surgery and should be counselled about the risk of excess residual refractive error. If there is a history of laser-assisted in situ keratomileusis (LASIK), pre-surgical planning includes topography to look for decentred or irregular ablations; if present, multi-focal or extended depth of focus IOLs are usually avoided due to the risk of visual disturbances.
Patients with a history of photorefractive keratectomy or radial keratotomy (RK) are likely to have more epithelial remodelling than patients with previous LASIK. Prior RK surgery is also associated with an increased risk of postoperative irregular astigmatism and hyperopic drift. Any surgical incisions should avoid previous incision sites to prevent epithelial ingrowth. An alternative in those with a history of RK is the scleral tunnel approach.
Concomitant eye pathology: angle-closure glaucoma
Sometimes in an eye with a predisposed shallow anterior chamber, cataracts can worsen narrowing of the filtration angle sufficiently to predispose to acute angle-closure glaucoma. In these cases, an opening is created in the iris (a peripheral iridotomy).
Cataract surgery may be performed as an additional procedure in people who continue to have raised intra-ocular pressure and/or residual visual impairment, independent of the degree of lenticular opacity.
One Cochrane review reported moderate-certainty evidence that lens extraction has an advantage over laser peripheral iridotomy for chronic primary angle-closure glaucoma over 3 years of follow-up. It also concluded that there was low-certainty evidence that combining phacoemulsification with either viscogonioplasty or goniosynechialysis does not add any benefit over phacoemulsification alone.[74]
Concomitant eye pathology: uveitis
In cases of long-standing and mature cataract, the cortex can become liquefied resulting in a morgagnian cataract. In this setting, lens proteins can leak from the capsular bag and cause chronic inflammation and elevated pressures within the eye.
Treatment is the surgical removal of the cataract with or without IOL implant, regardless of the degree of visual loss. Before surgery, ocular inflammation must be brought under control (which may involve systemic therapy) and raised intra-ocular pressure reduced.[Figure caption and citation for the preceding image starts]: Morgagnian cataract: a late end-stage cataractFrom the personal collection of M. Bowes Hamill, MD [Citation ends].
Concomitant eye pathology: traumatic cataract with rupture of the lens capsule
Following blunt or penetrating injury to the globe, the lens capsule can be ruptured, resulting in exposure of the lens cortex to aqueous fluid. The normally clear lens cortex then becomes fluffy and opaque, and the fluid may enter the anterior chamber.
Initially, the eye should be assessed for penetrating trauma. Open wounds should be sutured, focusing on anterior segment structures. Prophylactic antibiotics should be considered and tetanus status assessed. Subsequent inflammation is treated with corticosteroid eye drops. Elective lens removal is performed in the following days to weeks. [Figure caption and citation for the preceding image starts]: Traumatic cataract and iris traumaFrom the personal collection of M. Bowes Hamill, MD [Citation ends].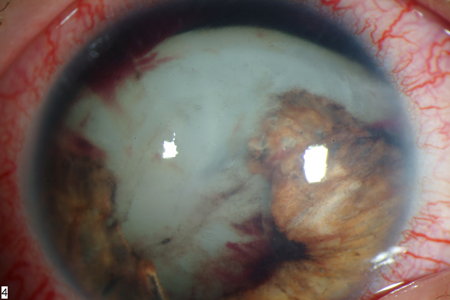
Concomitant eye pathology: diabetic retinopathy
Cataract surgery in patients with diabetes can be technically challenging if the pupil does not dilate well and because the endothelium is more susceptible to surgical trauma. Postoperatively, there is an increased risk of infection, macular oedema, posterior capsule opacification, and diabetic retinopathy exacerbation.[75]
Therefore, patients with mild cataract should be assessed carefully. Those without visual loss and with a clear fundus view may not require cataract removal.
Prior to cataract surgery, patients with moderate cataract should:
have laser pan-retinal photocoagulation, to treat any severe non-proliferative or proliferative diabetic retinopathy, and
focal/grid laser or anti-vascular endothelial growth factor (anti-VEGF) therapy, to treat any diabetic macular oedema.
Patients with severe cataract where poor fundus view prevents adequate assessment of diabetic retinopathy should have early cataract surgery followed by assessment and treatment of the retinopathy. If diabetic macular oedema is present, perioperative anti-VEGF therapy can be considered.[76] One meta-analysis of six studies of 283 eyes found that intravitreal bevacizumab injection significantly reduced progression of diabetic retinopathy and maculopathy at 6 months after cataract surgery.[77]
There is an increased risk of postoperative macular oedema in patients with diabetic retinopathy undergoing cataract surgery, particularly in those with more severe retinopathy.[78] This risk can be reduced by perioperative NSAIDs and corticosteroids.[79][80]
See Diabetic retinopathy.
Subsequent treatment
The natural crystalline lens will not regenerate after cataract surgery. In most cases, the capsular bag of the crystalline lens is left in situ to support the IOL implant. Some lens epithelial cells that remain on the internal surface of the retained capsular bag will proliferate. This may result in a gradual opacification of the posterior capsule that can reduce the patient's vision. This capsular opacification is termed a secondary cataract.
If the vision reduction is significant, an opening can be made in the posterior capsule with a neodymium-doped yttrium aluminium garnet (Nd:YAG) laser.
This treatment is generally done in the clinic and results in almost immediate restoration of vision. Once a capsular opening has been made, the capsule will not regenerate and a second treatment is rarely necessary.
Use of this content is subject to our disclaimer