Case history
Case history #1
A 68-year-old woman presents with word-finding difficulty, which comes on slowly and progresses over several weeks. Her family has noted some confusion, cognitive decline, blunted affect, and difficulty with gait. General blood tests are normal and evaluations are negative for HIV, Lyme disease, and bacterial, fungal, and viral infections.
Case history #2
A 50-year-old man presents with a relatively rapid two year decline in cognitive function. Symptoms began with behavioural changes and progressed to short-term memory loss, tremor in his left arm, and ataxia, and development of a shuffling gait. One year later, he developed depression, worsening bradykinesia, slurred hypophonic speech, and trouble swallowing. Family history includes a mother who died of an undiagnosed type of dementia with onset in her late 50s.
Other presentations
Some clinicians call Creutzfeldt-Jakob disease (CJD) the great imitator, as it can present like many other neurological/psychiatric conditions, depending where in the brain the prions are accumulating and causing neuronal dysfunction. Although typically of subacute onset (symptoms developing over days to weeks), sporadic CJD (sCJD) sometimes presents acutely, similar to a stroke.[15] Two variations of sCJD, the Heidenhain and Brownell-Oppenheimer variants, may also occur. In the Heidenhain variant of sCJD, patients present early on with predominantly visual symptoms, generally in the absence of other symptoms.[16][17] The Brownell-Oppenheimer variant is a cerebellar variant with first symptoms of profound ataxia.[18] The occurrence of a rapidly progressive dementia with motor signs (e.g., parkinsonism, incoordination, and myoclonus) and behavioural changes all progressing over several weeks, with generally normal CSF findings (mildly elevated protein is common) and a brain diffusion-weighted imaging MRI showing hyperintensity of the cortical gyri and basal ganglia is virtually pathognomonic for sCJD. [Figure caption and citation for the preceding image starts]: Changes in the basal ganglia seen in Creutzfeldt-Jakob disease. (A) Fluid-attenuated inversion recovery MRI and (B) diffusion-weighted MRI of the same patient demonstrate bilateral basal ganglia hyperintensities (arrows). There is also mild bilateral medial thalamus and pulvinar hyperintensityFrom the personal collection of Dr M. Geschwind [Citation ends].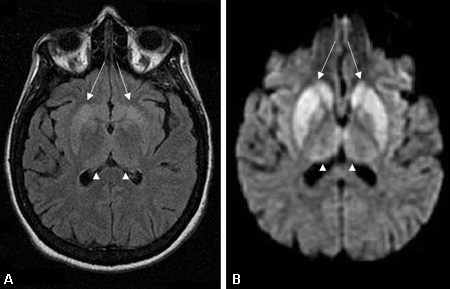 [Figure caption and citation for the preceding image starts]: Bilateral medial thalamus and pulvinar hyperintensity (arrowheads) on (A) fluid-attenuated inversion recovery and (B) diffusion-weighted MRI in a patient with Creutzfeldt-Jakob. This patient also has significant basal ganglia hyperintensity on both sequences (arrows)From the personal collection of Dr M. Geschwind [Citation ends].
[Figure caption and citation for the preceding image starts]: Bilateral medial thalamus and pulvinar hyperintensity (arrowheads) on (A) fluid-attenuated inversion recovery and (B) diffusion-weighted MRI in a patient with Creutzfeldt-Jakob. This patient also has significant basal ganglia hyperintensity on both sequences (arrows)From the personal collection of Dr M. Geschwind [Citation ends]. [Figure caption and citation for the preceding image starts]: Diffuse cortical ribboning (arrows) seen on (A) diffusion-weighted imaging (DWI) and less so on (B) fluid-attenuated inversion recovery (FLAIR) MRI. Both sequences show cerebral cortex gyral hyperintensitiesFrom the personal collection of Dr M. Geschwind [Citation ends].
[Figure caption and citation for the preceding image starts]: Diffuse cortical ribboning (arrows) seen on (A) diffusion-weighted imaging (DWI) and less so on (B) fluid-attenuated inversion recovery (FLAIR) MRI. Both sequences show cerebral cortex gyral hyperintensitiesFrom the personal collection of Dr M. Geschwind [Citation ends].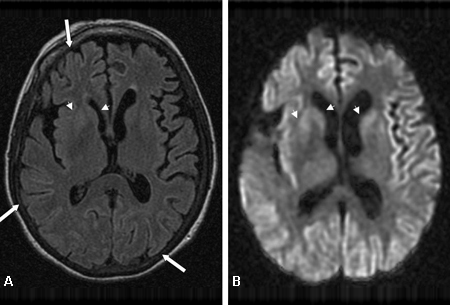
Use of this content is subject to our disclaimer