History and exam
Key diagnostic factors
common
presence of risk factors
Key risk factors include underlying liver disease (particularly cirrhosis), chronic hepatitis B infection, chronic hepatitis C cirrhosis, chronic heavy alcohol use, diabetes mellitus, obesity, and family history of liver cancer.
uncommon
hepatomegaly
Liver may be enlarged due to hypervascularity of tumour or continued inflammation from chronic liver disease.
Other diagnostic factors
common
abdominal distension
Patients typically present with abdominal fullness or ascites in association with cirrhosis.[Figure caption and citation for the preceding image starts]: This female Cambodian patient presented with a distended abdomen due to HCC resulting from chronic hepatitis B infectionCenters for Disease Control and Prevention / Patricia Walker, MD, Regions Hospital, MN; used with permission [Citation ends].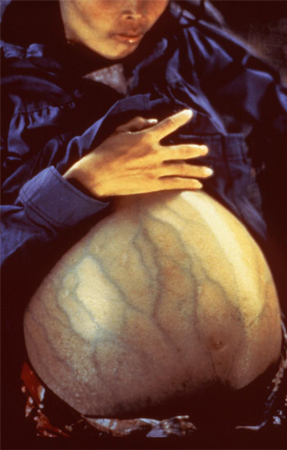
oesophageal or gastric variceal bleeding
More common in patients with decompensated cirrhosis.
right upper quadrant abdominal pain
Due to enlarged liver, liver inflammation, and stretching of the liver capsule.
early satiety
Occurs due to compression of the stomach by ascites.
weight loss
Non-specific but a typical clinical feature.
lower extremity oedema
Non-specific feature.
hepatic encephalopathy
More common in patients with decompensated cirrhosis.
cachexia
May be associated with cirrhosis and/or HCC.
jaundice
Indicative of progressive decompensated cirrhosis.
splenomegaly
Indicative of portal hypertension secondary to cirrhosis.
asterixis
Much more common in decompensated cirrhosis and suggestive of hepatic encephalopathy.
spider naevi
Indicative of chronic liver disease or cirrhosis.
palmar erythema
Indicative of chronic liver disease or cirrhosis.
periumbilical collateral veins
Mainly present in patients with decompensated cirrhosis.
fetor hepaticus
In patients with hepatic encephalopathy.
uncommon
diarrhoea
Maybe a feature indicating paraneoplastic syndrome in patients with HCC.
paraneoplastic syndrome
Hypoglycaemia may be a part of paraneoplastic syndrome. Several other paraneoplastic syndromes have been associated with HCC, including hypercalcaemia, erythrocytosis, watery diarrhoea (due to vasoactive intestinal peptide or gastrin), dermatomyositis, pemphigus foliaceus, and acanthosis nigricans.
bone pain
Indicative of metastases.
severe abdominal pain
In association with spontaneous rupture of the tumour into the peritoneal cavity.
obstructive jaundice
May be due to tumour obstructing the bile ducts.
enlarged haemorrhoidal veins
These are present in the rectum of patients with advanced or decompensated cirrhosis.
vascular bruit
Occurs secondary to hypervascularity of the tumour.
Risk factors
strong
cirrhosis
Considered the major predisposing risk factor, as HCC is a primary cancer arising from hepatocytes in predominantly cirrhotic liver. More than 80% of patients with HCC have cirrhosis.[3]
chronic hepatitis B (HBV) infection
One of the most prevalent aetiological risk factors worldwide, except in areas with dedicated virus elimination programmes.[3][29]
HBV infection at an early age and HBV carrier stage increases the risk of HCC.[30]
The risk increases in patients who have hepatitis Be antigen (HBeAg), high HBV DNA level, pre-core/basal core promoter mutation, older age, cirrhosis, elevated aminotransferase levels, high alcohol consumption, and co-infection with hepatitis C virus.[18][30][31][32][33][34][35]
One US study in adults aged ≥30 years found that 6.6% of HCC cases could be attributed to HBV infections.[36]
chronic hepatitis C (HCV) infection
One of the most prevalent aetiological risk factors worldwide, except in areas with dedicated virus elimination programmes.[3][29]
Unlike HBV, patients with HCV infection almost always develop cirrhosis before developing HCC.[37] 2% to 20% of people with chronic HCV infection develop cirrhosis, usually over a period of approximately 20-25 years.[38] Viral co-infection (e.g., HBV or HIV), duration of infection and high alcohol consumption increase the risk of development of cirrhosis and HCC in patients with HCV.[35][39]
The length of time patients have the virus correlates with the risk of HCC development.
One US study in adults aged ≥30 years found that 24% of HCC cases could be attributed to HCV infections.[36]
chronic heavy alcohol use
diabetes
obesity
family history of liver cancer
There is a close correlation between family history of HCC in a first-degree relative and the development of HCC. However, the exact nature of this relationship is not yet fully understood.[19]
weak
aflatoxin exposure
The toxin usually contaminates corn, soya beans, and peanuts and causes mutation of the p53 tumour-suppressor gene, which leads to the development of HCC.[43]
thorium dioxide radioactive contrast exposure
Thorium dioxide was a radioactive contrast used in the early 1920s to 1950s. It has a prolonged half-life and is taken up by liver, spleen, and bone marrow, and causes HCC with a latent period of 15-25 years.[44]
Thorium dioxide is no longer used for imaging, and it is unlikely that any further cases of HCC due to this contrast agent will occur.
haemochromatosis
Iron overload in patients with hepatitis C virus increases the risk for HCC. Patients with genetic haemochromatosis are at an increased risk for HCC.[45] Furthermore, first-degree relatives of patients with hereditary haemochromatosis (HH) have a high chance of inheriting HH and, therefore, have an increased risk for HCC.[45]
cigarette smoking
Smoking damages hepatocytes by direct or indirect effect, and by oncogenic or immunological effect. It produces the chemicals that cause necro-inflammation and fibrosis and can also cause iron overload in the liver by secondary polycythaemia.[46][47]
One US study in adults aged ≥30 years found that 23% of HCC cases could be attributed to smoking.[36]
alpha-1-antitrypsin deficiency
An inherited disorder caused by mutation in the SERPINA1 gene, which results in destruction of lung and liver cells by neutrophil elastase due to the deficiency or abnormal formation of alpha-1 antitrypsin.[48] These patients are at risk of developing liver cirrhosis as well as lung emphysema.
porphyria cutanea tarda
primary biliary cholangitis (PBC)
HCC is a complication of long-standing PBC. Older age, male sex, and portal hypertension are the clinical predictors for HCC in patients with PBC.[51]
primary sclerosing cholangitis (PSC)
Patients with late-stage cirrhosis due to PSC may be at increased risk of HCC. The incidence of HCC in PSC has not been well studied, but limited data suggest a lifetime incidence of 0.3% to 2.8%.[52]
use of androgenic steroids
Long-term use of anabolic androgenic steroids increases the risk for both benign and malignant liver tumours. Hepatocytes express androgen and oestrogen receptors. Experimentally, both androgens and oestrogens have been implicated in stimulating hepatocyte proliferation and may act as liver tumour inducers or promoters.[53][54]
use of oral contraceptives
Long-term use of oral contraceptives increases the risk for both benign and malignant liver tumours. Hepatocytes express androgen and oestrogen receptors. Experimentally, both androgens and oestrogens have been implicated in stimulating hepatocyte proliferation and may act as liver tumour inducers or promoters.[53][54]
Use of this content is subject to our disclaimer