Approach
Diagnosis is based on clinical assessment and/or screening of patients who are at high risk for developing HCC.
HCC presents with a liver mass (or masses) on abdominal imaging. Elevated serum alpha fetoprotein (AFP) may be corroborative, and diagnosis is confirmed by arterial hypervascularisation or hyperenhancement and venous/late-phase washout of mass or masses on dynamic imaging.[6][7][59]
Liver biopsy of the mass is not required to confirm the diagnosis of HCC in the majority of patients, but may be considered if the mass does not show typical imaging characteristics of an HCC and is of indeterminate nature on imaging. The American Association for the Study of Liver Diseases (AASLD) states that for patients with cirrhosis or chronic hepatitis B virus (HBV) infection, HCC diagnosis may be based on non-invasive imaging criteria and/or pathology. For other patients, the AASLD recommends that histological confirmation of HCC is required.[3]
Clinical presentation
The typical clinical features of HCC are right upper quadrant abdominal pain, jaundice, abdominal distension, lower extremity oedema, early satiety, and weight loss. If a patient has decompensated cirrhosis, they may present with variceal bleeding. [Figure caption and citation for the preceding image starts]: This female Cambodian patient presented with a distended abdomen due to HCC resulting from chronic hepatitis B infectionCenters for Disease Control and Prevention / Patricia Walker, MD, Regions Hospital, MN; used with permission [Citation ends].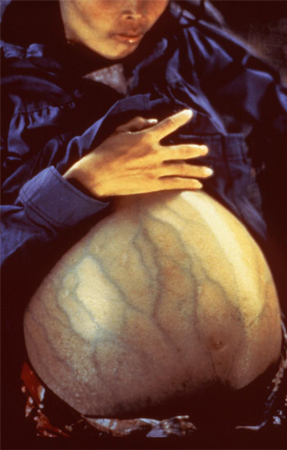
There may be a personal history of conditions leading to cirrhosis or metabolic dysfunction associated steatotic liver disease, for example, heavy alcohol use, hepatitis B and C infection, obesity, diabetes mellitus, primary biliary cholangitis, previous exposure to thorium dioxide radioactive contrast, prolonged use of androgens/oestrogens, haemochromatosis, or primary sclerosing cholangitis.
There may be a family history of HCC or haemochromatosis predisposing to development of HCC and haemochromatosis, respectively.
Risk factors for viral hepatitis include blood transfusions, tattoos, unprotected sexual intercourse, intravenous drug use, heavy alcohol use, and household contact (HBV infection).
Many patients who are diagnosed during screening abdominal ultrasound of the liver are asymptomatic.
Other rare presentations are severe abdominal pain (spontaneous rupture of the tumour into the peritoneal cavity), obstructive jaundice, diarrhoea, paraneoplastic syndrome, and bone pain in metastatic cases.
Clinical examination
Physical examination findings may reflect the underlying chronic liver disease. Therefore, the physician should look for spider naevi, palmar erythema, ascites, hepatomegaly, splenomegaly, asterixis, jaundice, cachexia, hepatic encephalopathy, fetor hepaticus, periumbilical collateral veins, enlarged haemorrhoidal veins, and vascular bruit.
Ultrasound
Ultrasound is the initial imaging test of choice and is used to screen for HCC in high-risk populations, such as people with a high risk of cirrhosis or known cirrhosis.
Laboratory investigations
Recommended routine tests for all patients with lesions suggestive of HCC on ultrasound include evaluation of liver function, full blood count, basic metabolic panel, and coagulation profile to determine the severity of chronic liver disease, including cirrhosis. It is also important to screen these patients for hepatitis B and C infection.
Serum AFP levels can be helpful, although they are elevated in only 60% of patients with HCC (typically those with the most advanced disease), hence a normal AFP level does not rule out HCC.[60] Further, elevated AFP levels can also be seen in other cancers (e.g., intrahepatic cholangiocarcinoma, gastric cancer, and germ cell tumours).[3] A rise in serum AFP in a patient with cirrhosis should raise the suspicion for HCC. Mild elevations may occur in patients with chronic hepatitis without HCC. Sensitivity ranges from 41% to 65%, and specificity ranges from 80% to 94%.[61] Specificity increases with higher AFP levels.[62] AFP may be used in conjunction with abdominal ultrasound when screening for HCC. The AASLD advises against using AFP alone to diagnose HCC and advises that patients with non-characteristic imaging should undergo a biopsy, irrespective of the AFP level.[3]
Subsequent imaging
If there is an elevated AFP and/or abnormal ultrasound with focal liver lesion(s), then multidetector computed tomography or dynamic contrast-enhanced magnetic resonance imaging (MRI) should be ordered to confirm the diagnosis.[3][63] The National Comprehensive Cancer Network (NCCN) suggests liver dynamic computed tomography or dynamic MRI as an alternative to ultrasound if ultrasound is unable to detect nodules or if visualisation is poor.[64] Lesions that are hypervascular on arterial phase imaging, with washout in the portal venous or delayed phase, are typical of HCC. [Figure caption and citation for the preceding image starts]: MRI: hypervascularity on the arterial phaseFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends].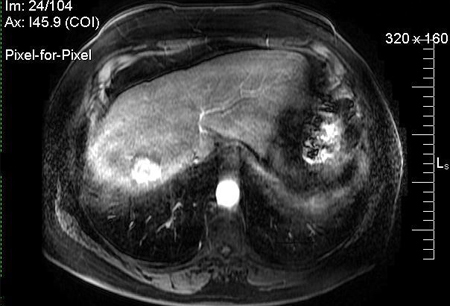 [Figure caption and citation for the preceding image starts]: MRI: washout portal phaseFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: MRI: washout portal phaseFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends].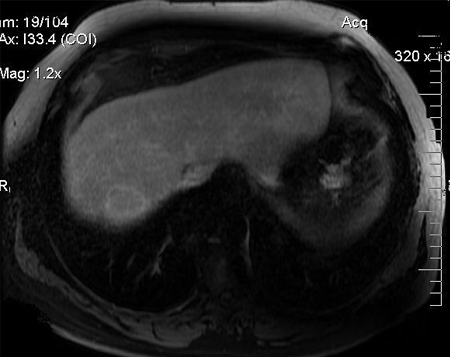 [Figure caption and citation for the preceding image starts]: MRI: following transarterial chemo-embolisation treatmentFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: MRI: following transarterial chemo-embolisation treatmentFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends].
One Cochrane review found that magnetic resonance imaging may miss up to 16% of people with HCC, and 6% of patients without HCC may be treated unnecessarily.[65]
[  ]
]
Pulmonary metastases should then be excluded with a chest computed tomography scan. If a patient complains of bone pain, a bone scan may be warranted to evaluate for bone metastases.
Liver biopsy
Most of the time, the diagnosis of HCC can be made radiologically in patients with cirrhosis without the need for liver biopsy. However, biopsy should be considered if the lesion remains indeterminate and in order to establish the diagnosis of HCC in patients without cirrhosis. The AASLD advises biopsy over repeat imaging if an immediate diagnosis would impact management decisions.[3]
An ultrasound-guided percutaneous liver biopsy is favoured.[Figure caption and citation for the preceding image starts]: Medium power microscopic view of a haematoxylin and eosin stained section depicting normal liver on the right and HCC on the left. A sharp boundary separates the distinct zones of normal liver and tumourFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends].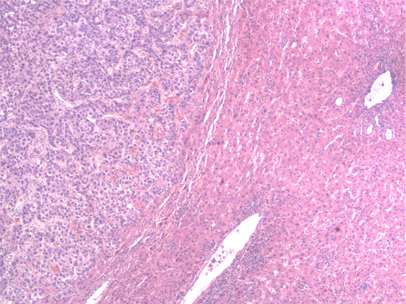 [Figure caption and citation for the preceding image starts]: High-power view of haematoxylin and eosin stained section of a well-differentiated HCC. Predominantly a solid pattern of growth with some nesting of malignant cells, separated by compressed sinusoids; some cells have clearing of the cytoplasmFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: High-power view of haematoxylin and eosin stained section of a well-differentiated HCC. Predominantly a solid pattern of growth with some nesting of malignant cells, separated by compressed sinusoids; some cells have clearing of the cytoplasmFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends].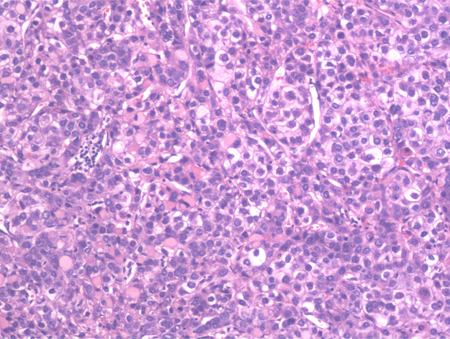
Core needle biopsy may be considered in certain clinical scenarios.[64]
Biopsy of liver lesions may also be necessary if clinical features suggest the possibility of metastatic liver disease or cholangiocarcinoma.
Use of this content is subject to our disclaimer