Tricyclic antidepressant overdose
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
suspected or confirmed TCA overdose
supportive care and monitoring
The patient should be rapidly stabilised. Assess airway, breathing, and circulation; obtain intravenous access; attach a cardiac monitor; and obtain an ECG to look for QRS prolongation.[Figure caption and citation for the preceding image starts]: Classic ECG changesFrom the collection of R.S. Hoffman; used with permission [Citation ends].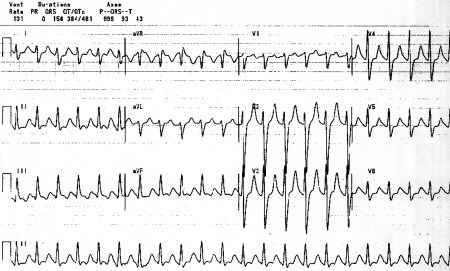
Acidosis, hypoxia, and electrolyte abnormalities should be corrected initially.
gastrointestinal decontamination
Treatment recommended for ALL patients in selected patient group
The aim is to bind any free drug in the gastrointestinal tract with activated charcoal before absorption occurs.[28]Dargan PI, Colbridge MG, Jones AL. The management of tricyclic antidepressant poisoning: the role of gut decontamination, extracorporeal procedures and fab antibody fragments. Toxicol Rev. 2005;24:187-194. http://www.ncbi.nlm.nih.gov/pubmed/16390220?tool=bestpractice.com
Attention to the airway is critical to avoid aspiration. Pulmonary aspiration of activated charcoal may be life-threatening.
Primary options
activated charcoal: 1 g/kg orally as a single dose, repeat every 2-4 hours if required
sodium bicarbonate
Treatment recommended for ALL patients in selected patient group
Sodium bicarbonate boluses should be given to narrow the QRS to <100 milliseconds, aiming for a maximum pH of between 7.5 and 7.55. There is some debate as to whether these initial boluses should be followed by a continuous infusion or additional boluses as needed; whichever is used, it is important to keep serum sodium <155 mEq/L and serum pH <7.55.[31]Lavonas EJ, Akpunonu PD, Arens AM, et al. 2023 American Heart Association focused update on the management of patients with cardiac arrest or life-threatening toxicity due to poisoning: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2023 Oct 17;148(16):e149-84. https://www.ahajournals.org/doi/10.1161/CIR.0000000000001161 http://www.ncbi.nlm.nih.gov/pubmed/37721023?tool=bestpractice.com
Two approaches that may be necessary to avoid excessive alkalemia include giving 3% sodium chloride without bicarbonate, or allowing for a small degree of permissive hypercapnia on the ventilator to allow for further bicarbonate boluses.
Primary options
sodium bicarbonate: consult specialist for guidance on dose
sodium bicarbonate plus anti-arrhythmic therapy
Treatment recommended for ALL patients in selected patient group
Major arrhythmias usually occur in association with other ECG changes or in the presence of complications such as coma, hypotension, or seizures. However, they may also occur in patients with only minor ECG abnormalities. Acidosis, hypoxia, and electrolyte abnormalities should be corrected initially.
Sodium bicarbonate may be effective at treating both tachyarrhythmias and bradyarrhythmias, even in the absence of metabolic acidosis.[21]Bradberry SM, Thanacoody HK, Watt BE, et al. Management of the cardiovascular complications of tricyclic antidepressant poisoning: role of sodium bicarbonate. Toxicol Rev. 2005;24:195-204. http://www.ncbi.nlm.nih.gov/pubmed/16390221?tool=bestpractice.com The incidence of ventricular arrhythmias requiring therapy other than sodium bicarbonate is very low. Anti-arrhythmic drugs should generally be avoided since they may lead to an exacerbation.
Sodium bicarbonate boluses should be given, aiming for a maximum pH of between 7.5 and 7.55. There is some debate as to whether these initial boluses should be followed by a continuous infusion or additional boluses as needed; whichever is used, it is important to keep serum sodium <155 mEq/L and serum pH <7.55.[31]Lavonas EJ, Akpunonu PD, Arens AM, et al. 2023 American Heart Association focused update on the management of patients with cardiac arrest or life-threatening toxicity due to poisoning: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2023 Oct 17;148(16):e149-84. https://www.ahajournals.org/doi/10.1161/CIR.0000000000001161 http://www.ncbi.nlm.nih.gov/pubmed/37721023?tool=bestpractice.com Aim to maintain QRS duration <100 milliseconds.
Consider use of magnesium sulfate for tachyarrhythmias that persist despite correction of acidosis and administration of sodium bicarbonate. Magnesium infusion or atrial overdrive pacing may also be of benefit in torsades de pointes. There is some limited clinical evidence of the benefit of lidocaine.[31]Lavonas EJ, Akpunonu PD, Arens AM, et al. 2023 American Heart Association focused update on the management of patients with cardiac arrest or life-threatening toxicity due to poisoning: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2023 Oct 17;148(16):e149-84. https://www.ahajournals.org/doi/10.1161/CIR.0000000000001161 http://www.ncbi.nlm.nih.gov/pubmed/37721023?tool=bestpractice.com [39]Foianini A, Wiegand TJ, Benowitz N. What is the role of lidocaine or phenytoin in tricyclic antidepressant-induced cardiotoxicity? Clin Toxicol (Phila). 2010;48:325-330. http://www.ncbi.nlm.nih.gov/pubmed/20507243?tool=bestpractice.com
For significant bradyarrhythmias (such as Mobitz Type II or complete heart block) that are unresponsive to treatment with sodium bicarbonate, consider use of isoprenaline as a temporary measure until temporary pacing is established. For severe life-threatening arrhythmias that are resistant to sodium bicarbonate, consider the use of intravenous lipid emulsion.[40]Cave G, Harvey M. Intravenous lipid emulsion as antidote beyond local anesthetic toxicity: a systematic review. Acad Emerg Med. 2009;16:815-824. http://www.ncbi.nlm.nih.gov/pubmed/19845549?tool=bestpractice.com [41]Cave G, Harvey M, Graudins A. Review article: intravenous lipid emulsion as antidote: a summary of published human experience. Emerg Med Australas. 2011;23:123-141. http://onlinelibrary.wiley.com/doi/10.1111/j.1742-6723.2011.01398.x/full http://www.ncbi.nlm.nih.gov/pubmed/21489160?tool=bestpractice.com [42]Jamaty C, Bailey B, Larocque A, et al. Lipid emulsions in the treatment of acute poisoning: a systematic review of human and animal studies. Clin Toxicol (Phila). 2010;48:1-27. http://www.ncbi.nlm.nih.gov/pubmed/20095812?tool=bestpractice.com
Primary options
sodium bicarbonate: consult specialist for guidance on dose
Secondary options
magnesium sulfate: consult specialist for guidance on dose
OR
lidocaine: consult specialist for guidance on dose
OR
isoprenaline: consult specialist for guidance on dose
intravenous fluids plus sodium bicarbonate
Treatment recommended for ALL patients in selected patient group
TCA poisoning can cause severe refractory hypotension as a result of impaired myocardial contractility, reduced cardiac output, and decreased peripheral vascular resistance. Sodium bicarbonate should be given to reduce cardiotoxicity.
Hypotension should be treated with intravenous crystalloid/colloid initially.
Sodium bicarbonate rapid intravenous boluses may correct acidosis and improve myocardial contractility. The risk of this therapy is making the patient too alkalotic. Patients on intravenous sodium bicarbonate need regular monitoring of pH and electrolytes. Serum pH should not exceed 7.5 to 7.55 and serum sodium should be <155 mEq/L. QRS duration should also be aimed to be kept <100 milliseconds.
Central venous pressure monitoring is likely to be required in patients whose blood pressure is unresponsive to intravenous fluids and sodium bicarbonate.
Primary options
sodium bicarbonate: consult specialist for guidance on dose
vasopressor or glucagon or extracorporeal membrane oxygenation
Additional treatment recommended for SOME patients in selected patient group
Vasopressors, such as noradrenaline (norepinephrine) or phenylephrine, should only be commenced in discussion with a medical toxicologist and intensive care physician.
High-dose glucagon or terlipressin can be considered, although clinical evidence is limited.[31]Lavonas EJ, Akpunonu PD, Arens AM, et al. 2023 American Heart Association focused update on the management of patients with cardiac arrest or life-threatening toxicity due to poisoning: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2023 Oct 17;148(16):e149-84. https://www.ahajournals.org/doi/10.1161/CIR.0000000000001161 http://www.ncbi.nlm.nih.gov/pubmed/37721023?tool=bestpractice.com [33]Sensky PR, Olczak SA. High-dose intravenous glucagon in severe tricyclic poisoning. Postgrad Med J. 1999;75:611-612. http://pmj.bmj.com/content/75/888/611.long http://www.ncbi.nlm.nih.gov/pubmed/10621904?tool=bestpractice.com [34]Sener EK, Gabe S, Henry JA. Response to glucagon in imipramine overdose. J Toxicol Clin Toxicol. 1995;33:51-53. http://www.ncbi.nlm.nih.gov/pubmed/7837313?tool=bestpractice.com [35]Zuidema X, Dünser MW, Wenzel V, et al. Terlipressin as an adjunct vasopressor in refractory hypotension after tricyclic antidepressant intoxication. Resuscitation. 2007;72:319-323. http://www.ncbi.nlm.nih.gov/pubmed/17123689?tool=bestpractice.com [36]Barry JD, Durkovich DW, Williams SR. Vasopressin treatment for cyclic antidepressant overdose. J Emerg Med. 2006;31:65-68. http://www.ncbi.nlm.nih.gov/pubmed/16798158?tool=bestpractice.com
Extracorporeal membrane oxygenation can be considered for severe cases of refractory hypotension.[29]Williams JM, Hollingshed MJ, Vasilakis A, et al. Extracorporeal circulation in the management of severe tricyclic antidepressant overdose. Am J Emerg Med. 1994;12:456-458. http://www.ncbi.nlm.nih.gov/pubmed/8031434?tool=bestpractice.com [30]Goodwin DA, Lally KP, Null DM Jr. Extracorporeal membrane oxygenation support for cardiac dysfunction from tricyclic antidepressant overdose. Crit Care Med. 1993;21:625-627. http://www.ncbi.nlm.nih.gov/pubmed/8472584?tool=bestpractice.com [31]Lavonas EJ, Akpunonu PD, Arens AM, et al. 2023 American Heart Association focused update on the management of patients with cardiac arrest or life-threatening toxicity due to poisoning: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2023 Oct 17;148(16):e149-84. https://www.ahajournals.org/doi/10.1161/CIR.0000000000001161 http://www.ncbi.nlm.nih.gov/pubmed/37721023?tool=bestpractice.com
Primary options
noradrenaline (norepinephrine): consult specialist for guidance on dose
OR
phenylephrine injection: consult specialist for guidance on dose
Secondary options
glucagon: consult specialist for guidance on dose
OR
terlipressin: consult specialist for guidance on dose
hyperventilation plus sodium bicarbonate
Treatment recommended for ALL patients in selected patient group
Cardiac arrest caused by TCAs should be treated by systemic alkalinisation with sodium bicarbonate and hyperventilation.
Standard cardiac resuscitation efforts should be implemented. Attempts at resuscitation should continue for at least 1 hour.
Primary options
sodium bicarbonate: consult specialist for guidance on dose
sodium bicarbonate plus benzodiazepine or barbiturate or propofol
Treatment recommended for ALL patients in selected patient group
Although most seizures are brief and self-terminating, they can cause worsening of acidosis and cardiotoxicity. Acidosis, hypoxia, and electrolyte abnormalities should be corrected initially. Rapid intravenous bolus of hypertonic sodium bicarbonate should be given as long as serum pH does not exceed 7.5 to 7.55. There is some debate as to whether these initial boluses should be followed by a continuous infusion or additional boluses as needed; whichever is used, it is important to keep serum sodium <155 mEq/L and serum pH <7.55.[31]Lavonas EJ, Akpunonu PD, Arens AM, et al. 2023 American Heart Association focused update on the management of patients with cardiac arrest or life-threatening toxicity due to poisoning: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2023 Oct 17;148(16):e149-84. https://www.ahajournals.org/doi/10.1161/CIR.0000000000001161 http://www.ncbi.nlm.nih.gov/pubmed/37721023?tool=bestpractice.com Aim to maintain QRS duration <100 milliseconds.[25]Body R, Bartram T, Azam F, et al. Guidelines in Emergency Medicine Network (GEMNet): guideline for the management of tricyclic antidepressant overdose. Emerg Med J. 2011;28:347-368. http://www.ncbi.nlm.nih.gov/pubmed/21436332?tool=bestpractice.com
Persistent seizures should be treated with a benzodiazepine, such as diazepam or lorazepam. Administration of benzodiazepines may cause further impairment of consciousness level and respiratory depression.
Consider the use of barbiturates or propofol if seizures are not controlled with benzodiazepines.
Phenytoin is contraindicated as it does not improve seizures and may worsen cardiac toxicity.[43]Callaham M, Schumaker H, Pentel P. Phenytoin prophylaxis of cardiotoxicity in experimental amitriptyline poisoning. J Pharmacol Exp Ther. 1988;245:216-220. http://www.ncbi.nlm.nih.gov/pubmed/3361443?tool=bestpractice.com
Primary options
sodium bicarbonate: consult specialist for guidance on dose
Secondary options
diazepam: consult specialist for guidance on dose
OR
lorazepam: consult specialist for guidance on dose
Tertiary options
phenobarbital: consult specialist for guidance on dose
OR
propofol: consult specialist for guidance on dose

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer