Approach
The main goal for treatment of tricyclic antidepressant (TCA) overdose is to provide respiratory and cardiovascular supportive care until the absorbed medicine can be metabolised and eliminated fully. Management of arrhythmias involves correction of acidosis, hypoxia, and electrolyte imbalance. Anti-arrhythmic drugs should generally be avoided.
Initial resuscitation
The patient should be rapidly stabilised. Assess airway, breathing, and circulation; obtain intravenous access; attach a cardiac monitor; and obtain an ECG to look for QRS prolongation.[Figure caption and citation for the preceding image starts]: Classic ECG changesFrom the collection of R.S. Hoffman; used with permission [Citation ends].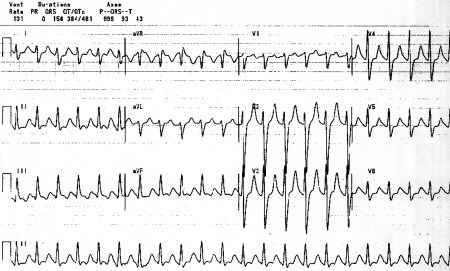
In suspected or confirmed TCA overdose with QRS >100 milliseconds, sodium bicarbonate boluses should be given to narrow the QRS to <100 milliseconds, provided blood pH is no greater than 7.55.
Admission
Patients who are asymptomatic 6 or more hours after accidental ingestion of a TCA dose that is unlikely to be toxic can be monitored at home. All other patients should be assessed in hospital.[22]
After initial stabilisation, patients who show signs of significant toxicity (e.g., hypotension, wide complex tachycardia, and anticholinergic signs) should be admitted to the intensive care unit.
Patients at risk of developing major complications are likely to have 1 or more of the following at the time of assessment:[23][24]
Heart rate 120 bpm or greater
Glasgow Coma Scale <14
QRS duration >100 milliseconds
Cardiac arrhythmias or conduction defects
Seizures
Respiratory rate <8 breaths/minute
Systolic blood pressure <90 mmHg
A widened QRS is generally regarded as a good predictor of subsequent complications, although one study has suggested that the presence of coma may be a better predictor of such complications.[25][26]
Patients who rapidly regain a normal mental status and whose ECG shows sinus tachycardia without QRS widening may be suitable for psychiatric assessment and discharge after gastrointestinal (GI) decontamination and a minimum observation of 6 hours.[27]
Gastric decontamination and extracorporeal procedures
For an early overdose (<2 hours after ingestion), GI decontamination should be considered by administering activated charcoal, providing that the airway can be protected.[28] There is no clear benefit from repeated doses of activated charcoal, but this may be considered if a slow release preparation has been ingested.
Clinical studies have not demonstrated any significant effect on outcome using orogastric lavage, and there is a risk that increased absorption of tablet matter may occur from the small intestine. In addition, orogastric lavage may worsen tachycardia and hypoxia; therefore, its routine use is not recommended. Extracorporeal procedures (such as haemoperfusion, haemofiltration, and haemodialysis) are unlikely to be of benefit because of the large volume of distribution and high protein binding capacity of TCAs, although extracorporeal circulation membrane oxygenation (ECMO) has been successfully used to treat refractory hypotension.[28][29][30][31]
Role of sodium bicarbonate in management of ECG changes and acidosis
System alkalinisation and the sodium load provided by hypertonic sodium bicarbonate reduces TCA-induced cardiotoxicity. Experimental and clinical studies have shown that both alkalinisation and sodium loading (with or without hyperventilation) improve ECG parameters, consciousness level, and hypotension.[21]
Sodium bicarbonate boluses should be given to narrow the QRS to <100 milliseconds, aiming for a maximum pH of between 7.5 and 7.55. There is some debate as to whether these initial boluses should be followed by a continuous infusion or additional boluses as needed; whichever is used, it is important to keep serum sodium <155 mEq/L and serum pH <7.55.[31] There is no evidence for prophylactic administration of sodium bicarbonate in the absence of cardiotoxicity or metabolic acidosis.
Boluses of hypertonic sodium bicarbonate serve three purposes for treating TCA overdoses:
To provide enough sodium substrate to allow for greater sodium entry into the myocardial cells, despite the sodium channel blockade. The result is a narrowed QRS and improved cardiac output.
To alkalinise the blood, which decreases the affinity of the TCA for the sodium channel.
This alkalinisation provides a buffer that helps to prevent, or limit, acidosis that might follow a seizure or hypoperfusion. Acidosis exacerbates cardiotoxicity by enhancing TCA binding to sodium channels.
The risk of this therapy is alkalaemia (pH >7.55), but the benefits generally outweigh this risk. Together, the sodium and bicarbonate seem to act synergistically to enhance their individual effects.[32]
In severe overdose, the amount of sodium bicarbonate needed to maintain an adequate QRS may be too large and could cause a severe alkalaemia. In these cases, hypertonic saline (3%) without bicarbonate can be used, or the patient can be allowed to become mildly hypercapnic to provide some acid buffer for required sodium bicarbonate boluses. In patients who cannot tolerate the volume associated with sodium bicarbonate therapy, consider a trial of hyperventilation.[31]
Management of hypotension
Hypotension should be treated with correction of hypoxia, intravenous fluids, and bicarbonate.
Use of inotropic agents and direct-acting vasopressors, such as noradrenaline (norepinephrine), is controversial and should only be done in consultation with a medical toxicologist and intensive care physician. Their use may cause hypoperfusion and increased acidosis which further worsens the toxicity of TCA overdose as it enhances the affinity of the TCA for the sodium channel and the degree of channel blockade. The result is wide complex rhythms with decreased cardiac output leading to further hypoperfusion and acidosis.
Glucagon has both inotropic and chronotropic effects on myocardial tissue. Case reports suggest that refractory hypotension has been treated successfully using high-dose intravenous glucagon, however, guidelines have not made a recommendation for or against its use in TCA overdose.[31][33][34] Other reports suggest successful use of vasopressin and the vasopressin analogue terlipressin in catecholamine-resistant hypotension.[35][36]
ECMO has also been successfully used to treat refractory hypotension.[29][30][31]
Management of arrhythmias
Major arrhythmias usually occur in association with other ECG changes or in the presence of complications such as coma, hypotension, or seizures. However, they may also occur in patients with only minor ECG abnormalities. Arrhythmias should be treated by correcting hypoxia, acidosis, and electrolyte abnormalities. Sodium bicarbonate boluses may be effective in treating arrhythmias, even in the absence of metabolic acidosis, and this should be the first-line treatment. Anti-arrhythmic drugs should generally be avoided since they may lead to an exacerbation.[21]
Tachyarrhythmias
Magnesium sulfate has been reported to treat ventricular tachycardia and ventricular fibrillation refractory to other treatment.[37][38] Magnesium infusion or atrial overdrive pacing may be of use to treat torsades de pointes. Class Ia (quinidine, disopyramide, procainamide) and Ic (flecainide, propafenone) anti-arrhythmic drugs should not be used since they have the same effects of sodium blockade as TCAs.[31] Class Ia drugs also have the potential to increase the risk of torsades de pointes. Theoretically, class Ib anti-arrhythmics (such as lidocaine and phenytoin) have less effect on myocardial contractility; however, evidence of clinical benefit with lidocaine in clinical studies is limited.[39] While phenytoin may reduce conduction defects, it may also increase the frequency and duration of ventricular tachycardia, and is therefore not recommended. Class II anti-arrhythmics (beta-blockers) may cause severe bradycardia and hypotension, and have been associated with cardiac arrest. Their use should be restricted to treatment of broad complex tachyarrhythmias in the context of cardiac arrest, where other treatments have been ineffective. There are no studies to support the use of class III (amiodarone) or class IV (calcium-channel blockers) anti-arrhythmics.
Bradyarrhythmias
Sodium bicarbonate should be used to treat bradycardia or heart block. Atropine is thought to be largely ineffective, since tricyclic-induced AV conduction failures usually occur distal to the AV node. Development of Mobitz type II or complete heart block may require insertion of a temporary pacing wire. In these circumstances the use of isoprenaline may be used as a temporising measure until temporary pacing is established.
Lipid emulsion
Animal studies and case reports suggest that life-threatening arrhythmias that are not corrected with sodium bicarbonate may respond to an infusion of lipid emulsion. Lipid emulsion may work by providing an intravascular lipid compartment into which lipid-soluble drugs may be sequestered by enhancing free fatty acid availability for cardiac metabolism, or by improving myocardial function by increasing intracellular calcium. This therapy has been used to treat life-threatening arrhythmias caused by highly lipid-soluble drugs, and it has been suggested for the management of severe TCA cardiotoxicity, although evidence of its efficacy is limited.[31][40][41][42]
Cardiac arrest
Cardiac arrest caused by TCAs should be treated by systemic alkalinisation with sodium bicarbonate and hyperventilation. Standard cardiac resuscitation efforts should be implemented. Attempts at resuscitation should continue for at least 1 hour.
Management of coma and seizures
Changes in consciousness level can occur rapidly, and coma is strongly associated with the risk of developing further complications of toxicity. Coma is also often associated with respiratory depression requiring intubation and ventilatory support. Flumazenil should not be given to reverse benzodiazepine toxicity in mixed overdoses since this can precipitate seizures. Seizures usually occur as an early complication and are unlikely to develop more than 12 hours post-ingestion. Though the majority of seizures are brief and self-terminating, even brief episodes can cause broadening of the QRS complex and hypotension by worsening acidosis, exacerbating the cardiotoxic effects of TCAs. There is no evidence to support the use of prophylactic treatment for patients thought to be at risk of developing seizures. Seizures that are not self-terminating should be treated with benzodiazepines, followed by barbiturates or propofol, if required.[25] Phenytoin is contraindicated as it does not improve seizures and may worsen cardiac toxicity.[43]
Use of this content is subject to our disclaimer