Differentials
Interstitial cystitis/primary bladder pain syndrome
SIGNS / SYMPTOMS
The patient may describe a history of pelvic pain which worsens on bladder filling or emptying, alongside increasingly low voiding volumes. Patients may also experience urinary urgency that can lead to urinary incontinence. Patients may report anal pain and urethral itching. Symptoms may be exacerbated by specific foods and emotional or physical stress.
INVESTIGATIONS
Cystoscopy: may reveal reddened mucosal areas often associated with small vessels radiating towards a central scar, sometimes covered by a small clot or fibrin deposit (Hunner lesions) in interstitial cystitis/primary bladder pain syndrome type 3C.[42]
[Figure caption and citation for the preceding image starts]: Cystoscopy in a 65-year old patient with bladder pain syndrome type 3C - corresponding to "classical'' interstitial cystitis - larger mucosal haemorrhages (Hunner's lesions) seen after diagnostic cystoscopic hydrodistensionFrom the personal collection of Serge P. Marinkovic, MD; used with permission [Citation ends].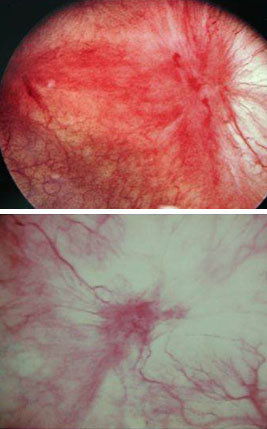
Urinary tract infection
SIGNS / SYMPTOMS
Symptoms may include acute onset of dysuria, urgency, frequency, and suprapubic pain. There may also be urinary hesitancy and a tender and enlarged prostate, along with fever and rigors. Urethral discharge may be present.[62]
INVESTIGATIONS
Urinalysis: positive leukocyte esterase and/or nitrite.
Urine microscopy: leukocytes and/or bacteria.
Urine culture: ≥10² CFU/mL.
Acute prostatitis
SIGNS / SYMPTOMS
Acute onset of lower urinary tract symptoms (such as urinary frequency, dysuria, and symptoms of obstructed flow), variable systemic signs (such as fever, rigors, and malaise), and evidence of recent or ongoing bacterial infection with a duration of <3 months. Tender, enlarged prostate gland on rectal examination is consistent with prostatitis.[63]
INVESTIGATIONS
Urinalysis: presence of leukocytes, bacteria.
Urine culture: positive for bacteria.
Epididymitis
SIGNS / SYMPTOMS
Typically presents with unilateral scrotal pain and swelling that develops over the course of a few days. Hot, erythematous, swollen hemiscrotum with diffuse enlargement of the testis in epididymo-orchitis. In severe cases, patients may have a fever and be systemically unwell.
INVESTIGATIONS
Colour duplex ultrasonography: may show an enlarged and hyperaemic epididymis.
Pyelonephritis
SIGNS / SYMPTOMS
Often a complication of a urinary tract infection (UTI), but can occur without history of UTI. Patients may report fever and chills and flank pain. Other key symptoms include nausea, vomiting, and dehydration.[64][65]
May be indicated by costovertebral angle pain with tenderness on examination.
INVESTIGATIONS
Urinalysis: pyuria, bacteriuria, and varying degrees of haematuria
Urine culture: positive for bacteria
Urethritis
SIGNS / SYMPTOMS
Urethral discharge, usually occurring between 4 days and 2 weeks after contact with an infected partner. An unexplained sensation of itching or irritation may be present between voids.[66]
INVESTIGATIONS
Gram stain of urethral discharge and/or urine sediment: ≥2 polymorphonuclear leukocytes per high power field plus documented urethral discharge is diagnostic for urethritis; presence of gram-negative diplococci is diagnostic for gonorrhoeal infection.
Culture of urethral discharge: chocolate agar positive for Neisseria gonorrhoeae; inoculate cell monolayers such as McCoy or Buffalo green monkey kidney for Chlamydia trachomatis.
Nucleic acid amplification tests: positive for causative organisms such as Neisseria gonorrhoeae, Chlamydia trachomatis, or Mycoplasma genitalium.
Prostate cancer
SIGNS / SYMPTOMS
Most patients are asymptomatic at presentation and are diagnosed after screening with prostate-specific antigen or discovered during digital rectal examination, in which there may be an asymmetric and/or indurated or nodular prostate, suggestive of malignancy.
Where symptoms of obstructed urine flow are present in malignant disease (such as nocturia and hesitancy), these are are usually progressive, whereas in PPPS there is most often (97%) an undulating course with symptom flares.[44]
INVESTIGATIONS
Serum prostate-specific antigen: elevated.
Multiparametric pelvic MRI: may identify clinically significant lesions on the prostate.
Prostate biopsy: may detect malignant cells in one or more biopsy specimens.
Bladder cancer
SIGNS / SYMPTOMS
Typically presents with painless gross or microscopic haematuria, which may be intermittent.[67] Patients may also present with symptoms such as frequency and dysuria, although these symptoms are usually progressive, whereas in PPPS there is usually (97%) an undulating course with symptom flares.[44]
INVESTIGATIONS
Urinalysis: haematuria is typical but may be absent; pyuria may also be seen.
Urine cytology: positive in up to 90% of patients with carcinoma in situ or high-grade tumours; positive in <33% of patients with low-grade transitional cell cancer.
Cystoscopy: visualises bladder tumours.
Colorectal cancer
SIGNS / SYMPTOMS
Typically presents with a change in bowel habit and in some patients with rectal bleeding. Patients may also present with weight loss. In malignant disease, symptoms are usually progressive, rather than following an undulating course with episodes of symptom flares which is more typical of PPPS.[44] Many pelvic malignancies present without pain, or are diagnosed after screening of asymptomatic patients.
INVESTIGATIONS
CBC: anaemia may be present.
Colonoscopy/CT colonoscopy: ulcerating or exophytic mucosal lesion that may narrow the bowel lumen.
Double-contrast barium enema: mass lesion in the colon; a characteristic 'apple core' lesion may be seen with cancers that encircle the bowel.
Benign prostatic hyperplasia (BPH)
SIGNS / SYMPTOMS
Typically may have symptoms such as weak urinary stream, straining, incomplete emptying and post-void dribbling. Patients may also present with acute retention of urine.
INVESTIGATIONS
Clinical diagnosis with negative urinalysis.
Histological examination of the prostate reveals BPH.
Nephrolithiasis
SIGNS / SYMPTOMS
Typically presents with acute, severe flank pain that radiates to the ipsilateral groin. However, some patients will have no radiation and some stones are asymptomatic. Nausea and vomiting are commonly associated with acute episodes. The patient may have a history of stone formation.[68][69]
INVESTIGATIONS
Urinalysis: may be normal; dipstick positive for leukocytes, nitrates, blood; microscopic analysis positive for WBCs, RBCs, or bacteria.
Non-contrast helical CT scan: calcification seen in renal collecting system or ureter; hydronephrosis; perinephric stranding (indicative of inflammation or infection).
Plain abdominal radiograph: calcification seen within urinary tract.
Neurogenic bladder
SIGNS / SYMPTOMS
This is a storage abnormality in patients with involuntary bladder contractions, usually seen in patients with vascular disease, Parkinson’s disease, multiple sclerosis, or diabetes mellitus with neuropathy.
INVESTIGATIONS
Urodynamic studies: abnormal with increased residual volume or catheterisation following voiding.
Urethral stricture
SIGNS / SYMPTOMS
There may be a history of straddle injury or prior urological surgery.
INVESTIGATIONS
Retrograde urethrogram: abnormal.
Uroflowmetry: diminished peak flow.
Cystoscopy: identification of stricture location and length.
Irritable bowel syndrome
SIGNS / SYMPTOMS
Patients may experience chronic changes in stool frequency, form, or appearance. Commonly associated with abdominal bloating and passing mucus per rectum. Spasmodic abdominal pain is often relieved by defecation.[70]
Be aware that the condition may coexist with chronic prostatitis.
INVESTIGATIONS
Clinical diagnosis: no differentiating tests.
Pudendal neuralgia (Alcock’s canal syndrome, pudendal canal syndrome, pudendal nerve entrapment)
SIGNS / SYMPTOMS
Unilateral or bilateral burning, prickling, stabbing, or numbness in the perineum, external genitalia, or scrotum may be present. Pain is usually worse with sitting and there may be a sense of a foreign object in the urethra or rectum.
INVESTIGATIONS
This is a clinical diagnosis; however, diagnostic nerve block via anaesthetic infiltration within the pudendal canal results in pain relief for the duration of anaesthesia.
Prostatic abscess
SIGNS / SYMPTOMS
Usually a complication of acute bacterial prostatitis, with an increased risk of development in patients with an indwelling catheter, instrumentation of the lower urinary tract, and immunosuppression (e.g., diabetes, HIV infection).[71] The patient may be febrile, report severe perineal pain, and may have difficulty passing urine. Rectal examination may reveal a fluctuant area in the prostate.
INVESTIGATIONS
Transrectal ultrasound: reveals one or more hypoechoic areas that contain thick pus.
Use of this content is subject to our disclaimer