Investigations
1st investigations to order
upper gastrointestinal endoscopy
Test
Refer any patient who presents with dyspepsia together with significant acute gastrointestinal bleeding, immediately (on the same day) to a specialist for endoscopy.[46]
Refer any patient ≥55 years who has weight loss together with any one of dyspepsia, reflux, or upper abdominal pain for upper gastrointestinal endoscopy within 2 weeks.[47]
Endoscopy is used to exclude malignancy in patients ≥55 years who present with dyspepsia, upper abdominal pain, or reflux together with weight loss, low haemoglobin level, or raised platelet count.[47]
Endoscopy is the definitive diagnostic test for peptic ulcer disease. It is the most specific and sensitive test. If an ulcer is present, test biopsies for H pylori via histology and/or urease testing (rapid urease test). Both tests can detect H pylori; however, histology can determine if the ulcer is neoplastic (very rarely) and/or if there is evidence of a non-steroidal anti-inflammatory drug (NSAID) being the likely cause.
Note that in practice, the rapid urease test can be falsely negative if:
There is acute upper gastrointestinal bleeding
The patient is being treated with a PPI
The patient has received antibiotics that might reduce the density of H pylori colonisation.
Consider endoscopy subsequent to treatment if the patient fails to respond.
Repeat endoscopy after 6 to 8 weeks in patients with gastric ulcer to ensure ulcer healing and to rule out malignancy (unless excluded at initial endoscopy).
Anti-thrombotic treatment with either warfarin or a direct oral anticoagulant (DOAC) or dual antiplatelet therapy is not a contraindication to endoscopy. Upper gastrointestinal endoscopy with or without diagnostic biopsies is regarded as a low-risk procedure for bleeding, and no or minimal alterations in the antithrombotic regimen are required for non-emergency diagnostic endoscopy.
For low-risk endoscopic procedures such as diagnostic endoscopy with or without biopsy, the 2021 update to the British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guideline on endoscopy in patients on antiplatelet or anticoagulant therapy recommends:[50]
Continuing P2Y12 receptor antagonists as single or dual antiplatelet therapy (DAPT)
Continuing warfarin therapy
Check international normalised ratio (INR) 1 week before endoscopy
If the INR result is within the therapeutic range then continue with the usual daily dose
If the INR is above the therapeutic range but <5 then reduce daily dose until INR returns to the therapeutic range
If the INR is greater than 5 then defer the endoscopy and contact the anticoagulation clinic, or an appropriate specialist, for advice.
Omitting the morning dose of DOACs.
Result
peptic ulcer; may also detect cause (e.g., H pylori)
Helicobacter pylori carbon-13 urea breath test or stool antigen test
Test
If, after endoscopy, the patient’s H pylori status is uncertain, establish whether the patient is infected with H pylori using the urea breath test or stool antigen test; if these are unavailable, laboratory-based serology can be used provided its performance has been locally validated.[46][48]
Serology (antibody) testing gives less accurate results than urea breath testing or stool antigen testing and is unable to distinguish between active and historical infection.[46][53][54][55]
Proton-pump inhibitors (PPIs), bismuth, or other medications can interfere with the performance of diagnostic tests for H pylori.
Leave a 2-week washout period after PPI use and a 4-week washout after antibiotic use before testing for H pylori with a breath test or a stool antigen test, as these drugs supress bacteria and can lead to false negatives.[46][48]
Re-test to confirm successful eradication ofH pylori using a carbon-13 urea breath test 6 to 8 weeks after starting treatment.[46]
There is insufficient evidence to recommend the stool antigen test as a test of eradication.[46]
[Figure caption and citation for the preceding image starts]: Helicobacter pylori bacterium, transmission electron micrograph (TEM)Heather Davies/Science Photo Library [Citation ends].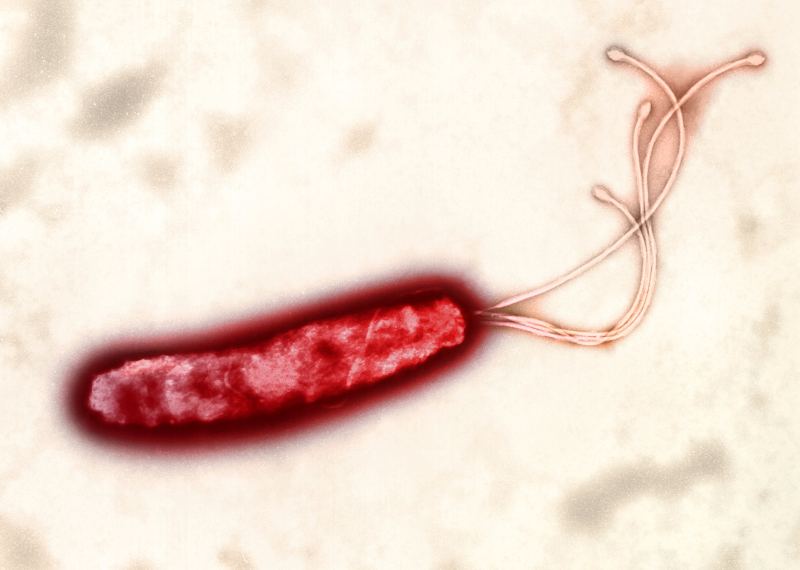
Result
positive result if H pylori present
FBC
Test
Order only if the patient seems clinically anaemic or has evidence of gastrointestinal bleeding.
Aids in evaluating the urgency with which the patient requires further work-up, but does not definitively diagnose peptic ulcer disease.
High platelet count or anaemia may indicate malignancy.[47]
Result
microcytic anaemia or high platelet count
Investigations to consider
fasting serum gastrin level
Test
Order if there are multiple duodenal ulcers (especially postbulbar) or in a patient with ulcers and diarrhoea.
The patient must be fasting and PPI therapy stopped.
Elevated levels in pernicious anaemia and other hypochlorhydric states results in low specificity.
Result
hypergastrinaemia in Zollinger-Ellison syndrome
urine NSAID screen
Test
Consider the possibility of surreptitious use of NSAIDs if the patient has recurrent or refractory ulcers.
Result
may be positive
Use of this content is subject to our disclaimer