Aetiology
The two major aetiologic factors responsible for peptic ulceration are infection by the gram-negative gastric pathogen Helicobacter pylori and the use of aspirin and non-steroidal anti-inflammatory drugs (NSAIDs). There is some synergy between these two major causes.[12]
Rarer causes include gastric ischaemia (responsible for the 'stress ulcers' that can occur in patients with multiple organ failure in intensive care units), Zollinger-Ellison syndrome (a syndrome of gastric acid hypersecretion caused by a gastrin secreting neuro-endocrine tumour), certain medications (e.g., potassium chloride, bisphosphonates), infections (cytomegalovirus in patients with HIV, and occasionally herpes simplex virus), and Crohn's disease. A small but increasing proportion of peptic ulcers seem truly idiopathic.[13][14]
Psychological stress may play a role in some patients. A population-based prospective study in Denmark that included 3379 individuals demonstrated that psychological stress increased the incidence of peptic ulcer in part by influencing health risk behaviours.[15] A higher incidence of ulcer disease is also reported after acute traumatic events such as bombing raids during World War 2 and following the Japanese tsunami.[16]
Pathophysiology
Peptic ulcers result from an imbalance between factors that can damage the gastroduodenal mucosal lining and defence mechanisms that normally limit the injury. Aggressive factors include gastric juice (including hydrochloric acid, pepsin, and bile salts refluxed from the duodenum), Helicobacter pylori, and non-steroidal anti-inflammatory drugs (NSAIDs).[17] Mucosal defences comprise a mucus bicarbonate layer secreted by surface mucus cells forming a viscous gel over the gastric mucosa. Also key is the integrity of tight junctions between adjacent epithelial cells, and the process of restitution, whereby any break in the epithelial lining is rapidly filled by adjacent epithelial and mucosal stromal cells that migrate to fill the gap. Mucosal defences rely heavily on an adequate blood supply.
In general, duodenal ulcers are the result of hypersecretion of gastric acid related to H pylori infection (the majority of patients), whereas secretion is normal or low in patients with gastric ulcers.[17]
[Figure caption and citation for the preceding image starts]: Helicobacter pylori bacterium, transmission electron micrograph (TEM)Heather Davies/Science Photo Library [Citation ends].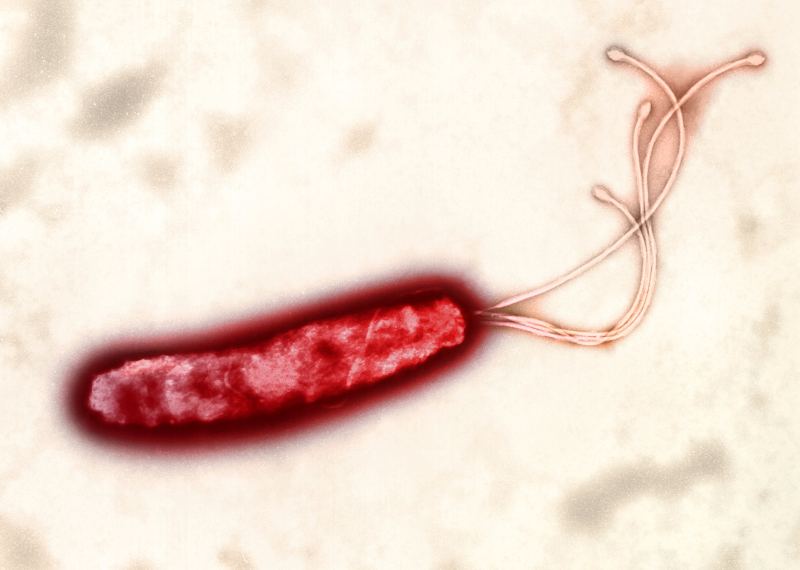
In duodenal ulcers, chronic H pylori infection confined mainly to the gastric antrum leads to impaired secretion of somatostatin and consequently increased gastrin release, resulting in gastric acid hypersecretion. In Zollinger-Ellison syndrome, a gastrin-secreting neuro-endocrine tumour is the stimulus for high rates of gastric acid secretion.
In gastric ulcers, longstanding H pylori infection throughout the stomach accompanied by severe inflammation results in gastric mucin degradation, disruption of tight junctions between gastric epithelial cells, and the induction of gastric epithelial cell death. NSAIDs cause injury directly (involving trapping hydrogen ions) and indirectly (a systemic effect involving the inhibition of cyclo-oxygenases, especially COX-1) and increase bleeding risk through antiplatelet actions.[12][18]
Classification
General
Peptic ulcers are generally categorised as gastric or duodenal.
Use of this content is subject to our disclaimer