Investigations
1st investigations to order
chest x-ray
Test
Enlarged main pulmonary artery is seen in 90%, enlarged hilar vessels in 80%, and pruning in 51% of patients with IPAH. All three abnormalities are seen 42% of the time.[6] The chest radiograph was normal in 6% of patients in the US National Institutes of Health (NIH) registry. In general, the chest radiograph is not sensitive or specific enough to establish the diagnosis.[39]
Result
attenuated peripheral vascular markings ('pruning'), enlarged pulmonary artery shadows, and opacification of the retrosternal space on the lateral view
ECG
Test
Findings of right ventricular hypertrophy (RVH): tall R wave and small S wave (R/S ratio >1) in lead V1, qR complex in V1, rSR' in V1, a large S wave and small R wave (R/S ratio <1) in V5 or V6, or a S1S2S3 pattern; right axis deviation: mean frontal plane QRS axis >100 degrees; right atrial enlargement: P wave ≥2.5 mm in leads II, III, and aVF.
Sensitivity of right axis deviation and RVH is only 73% and 55%, respectively, while specificity is 70% for both in patients with mean pulmonary artery pressure >50 mmHg.[41] Thus, a normal ECG does not rule out the presence of significant pulmonary hypertension. Subsequent ECGs should also be performed. [Figure caption and citation for the preceding image starts]: ECG showing a tall R wave and small S wave (R/S ratio >1) in lead V1, qR complex in V1, right axis deviation, and right atrial enlargement (P wave ≥2.5 mm in lead II)From the personal collection of the author, Gustavo A. Heresi, MD [Citation ends].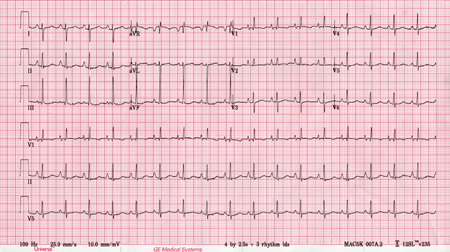
Result
RVH, right axis deviation, right atrial enlargement
transthoracic Doppler echocardiography
Test
Pulmonary artery systolic pressure (sPAP) is considered equal to right ventricular systolic pressure (RVSP) in the absence of pulmonic valve stenosis and outflow tract obstruction. RVSP is estimated on the basis of Doppler-acquired tricuspid regurgitation (TR) jet velocity plus estimated right atrial pressure from inferior vena cava (IVC) assessment. IVC-based estimation of right atrial pressure is prone to inaccuracy and can lead to amplification of measurement errors when calculating sPAP.[42] Correlation with right heart catheterisation measurements is variable (r from 0.57 to 0.93), and is more robust for sPAP >50 mmHg and <100 mmHg.[39] Sensitivity and specificity of the estimated sPAP in predicting pulmonary arterial hypertension ranges from 79% to 100%, and 60% to 98%.[43] TR velocity (TRV) should be used for screening for PH; a peak TRV of >2.8 m/s is suggestive of PH. TRV should be used with other transthoracic echocardiographic measures of RV function including the tricuspid annular plane systolic excursion (TAPSE), RV fractional area change (RV-FAC), RV free-wall strain, and tricuspid annulus velocity (S′ wave) derived from tissue Doppler imaging, and potentially RV ejection fraction (RVEF) derived from 3D echocardiography.[3] The TAPSE/sPAP ratio measures RV arterial coupling and may also aid diagnosis.[3][44] The pattern of RV outflow tract (RVOT) blood flow (mid-systolic 'notching') may suggest pre-capillary PH.[3] Echocardiography is a good screening test to detect pulmonary hypertension, but it always requires confirmation with right heart catheterisation. Should be repeated if required. [Figure caption and citation for the preceding image starts]: Transthoracic echocardiogram: apical 4-chamber view showing significant right atrial and right ventricular dilationFrom the personal collection of the author, Gustavo A. Heresi, MD [Citation ends].
Result
Peak TRV >2.8 m/s; RA area >18 cm²; TAPSE <18 mm; RVOT acceleration time <105 ms
right heart catheterisation
Test
Considered the definitive diagnostic test for pulmonary haemodynamic measurement and is required to confirm the presence of pulmonary hypertension, to establish the specific diagnosis, and to determine severity.[3][36] Should be repeated if required.
Result
mean pulmonary arterial pressure >20 mmHg at rest, with pulmonary arterial wedge pressure ≤15 mmHg and pulmonary vascular resistance (PVR) >2 Wood units
antinuclear antibodies (ANA)
pulmonary function tests
Test
Mild restrictive lung defect seen in 20% to 50% of patients.[41] Mild reduction in diffusion capacity seen in the majority of patients.
Result
normal or mild reductions in lung volumes; mild reduction in diffusion capacity
arterial blood gas (ABG)
Test
Used to differentiate between PAH groups, determine disease severity, and assess comorbidities.
Result
PaO₂: normal or reduced; PaCO₂: reduced
nocturnal oximetry
ventilation-perfusion (V/Q) scintigraphy
6-minute walk test
Test
Provides an estimation of exercise capacity and disease severity, as well as response to therapy and progression.[3] Should be repeated serially.
Result
absolute value of distance, per cent of predicted distance, oxygen saturation by pulse oximetry, heart rate, and Borg dyspnoea scale
B-type natriuretic peptide (BNP) or N-terminal proBNP (NT-proBNP)
Test
Is elevated in right ventricular pressure overload and correlates with severity of right ventricular dysfunction and mortality in IPAH.[3] Should be repeated subsequently.
Result
NT-proBNP >300 nanograms/L or BNP >50 nanograms/L
FBC
Test
Order as baseline and to exclude haemoglobinopathy as a cause of secondary pulmonary hypertension.
Result
normal
LFTs
Test
Order to exclude liver disease or portal hypertension as a cause of secondary pulmonary hypertension.
Result
normal
thyroid function tests
Test
Order to exclude thyroid disease as a cause of secondary pulmonary hypertension.
Result
normal
HIV serology
Test
Order to exclude HIV infection as a cause of secondary pulmonary hypertension.
Result
negative
Investigations to consider
high-resolution chest CT scan ± CT pulmonary angiography
Test
Useful to look for other causes of pulmonary hypertension such as emphysema and interstitial lung disease. Complementary CT pulmonary angiography can be used to rule out chronic thromboembolic pulmonary hypertension.
Result
may show central pulmonary artery dilation, narrowing of the peripheral pulmonary vessels, dilated bronchial arteries, right heart enlargement; hyperinflation will be seen in emphysema
cardiac MRI
Test
Assesses atrial and ventricular size, morphology, and function and can also provide additional information on right ventricular (RV)/left ventricular (LV) myocardial strain, and quantify stroke volume and intracardiac shunts for prognosis and monitoring.[3][36]
Result
RV volume, RV ejection fraction (EF), and stroke volume
vasodilator testing with inhaled nitric oxide, inhaled iloprost, or intravenous epoprostenol
Test
The primary objective is to identify a subset of IPAH patients who might be treated with oral calcium-channel blockers. Thus, it is not indicated in unstable patients or those who are in right heart failure.[35] Approximately 12% of patients are acute responders and only half of them will have a sustained response to calcium-channel blockers.[47]
Result
positive or negative; a positive acute vasodilator response is defined as a fall in mean pulmonary artery pressure of at least 10 mmHg to an absolute value ≤40 mmHg, with an increased or unchanged cardiac output
Use of this content is subject to our disclaimer