Monitoring
Papillary, follicular, or oncocytic (previously known as Hürthle cell)
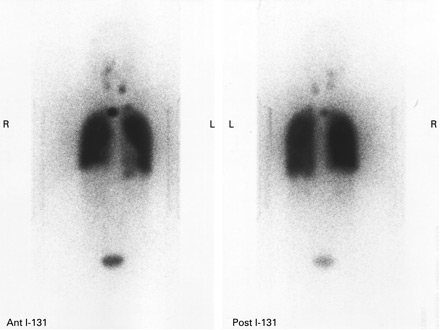
For patients treated with total thyroidectomy and adjuvant radioactive iodine (RAI) therapy, a whole-body RAI scan at 6 to 12 months after adjuvant RAI therapy is suggested for patients at high or intermediate risk of persistent disease.[1] Recombinant human thyroid-stimulating hormone (TSH) is used to increase the TSH levels, while the patient continues to be on thyroid hormone replacement. The scan detects residual thyroid tissue in the neck and also metastases.[Figure caption and citation for the preceding image starts]: Increased uptake of radioiodine in both pulmonary fields and the mediastinum due to miliary lung metastasis from papillary thyroid carcinomaGkountouvas A, Chatjimarkou F, Thomas D, et al. Miliary lung metastasis due to papillary thyroid carcinoma. BMJ Case Reports. 2009; doi:10.1136/bcr.06.2008.0322 [Citation ends].
During follow-up the best investigations are thyroglobulin, thyroglobulin antibody, and clinical examination. Thyroglobulin panel is an important investigation if the patient has undergone total thyroidectomy and radioiodine ablation. Any rise in thyroglobulin or thyroglobulin antibody is suggestive of recurrent thyroid carcinoma, most of which is recurrence in either the central compartment of the neck or the lateral neck.[29]
Although there is no definitive cut-off for thyroglobulin, >2 micrograms/L (2 nanograms/mL) is considered worrisome and >10 micrograms/L (10 nanograms/mL) suggests recurrent thyroid carcinoma. Thyroglobulin panel (including antibodies) may be performed twice yearly for the first 5 years and subsequently once yearly (if normal).
Ultrasound is done at baseline, and then annually combined with more frequent clinical examinations. Ultrasound may detect recurrent disease in the thyroid bed, the paratracheal area, or the lateral neck.
An elevated thyroglobulin or rising thyroglobulin antibodies are generally investigated with ultrasound and whole-body RAI scan. Recurrent disease or metastasis is ablated with I-131. Surgery may also be used for accessible disease.
Positron emission tomography/computed tomography (PET/CT) can be used to look for recurrent disease in patients with raised thyroglobulin and negative radioactive iodine scan.[95]
Medullary
Medullary cancer is monitored with serum calcitonin every 3 months for 2 years, followed by every 6 months for 3 years. If levels are undetectable they can then be followed annually. If serum calcitonin is elevated, ultrasound and CT of the neck/chest are indicated. If both are negative, PET scan may detect lesions missed by CT.[95]
Hypocalcaemia
Incidence of permanent hypocalcaemia due to parathyroid injury is extremely low. If post-operative hypocalcaemia persists for >3 weeks, it is more likely to be permanent. Treatment is with oral calcium and vitamin D.
Use of this content is subject to our disclaimer