The most common presentation is an asymptomatic thyroid nodule in women in their 30s or 40s.
Risk factors for thyroid cancer include a history of head and neck irradiation, which is a strong but uncommon factor. Thyroid cancer is more common in women, but men have a higher risk of malignancy in thyroid nodules.[29]Gharib H, Papini E, Garber JR, et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules - 2016 update. Endocr Pract. 2016 May;22(5):622-39.
https://www.endocrinepractice.org/article/S1530-891X(20)42954-4/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27167915?tool=bestpractice.com
Rarely, thyroid cancer occurs as part of a familial syndrome such as a multiple endocrine neoplasia (MEN) syndrome. See Multiple endocrine neoplasia syndromes.
Examination and detection of thyroid nodule
A thyroid nodule might be found on physical examination or incidentally on imaging studies.
18F-FDG positron emission tomography/computed tomography (PET/CT)-positive thyroid nodules found incidentally may have a higher risk of malignancy and should be investigated appropriately.[12]Bertagna F, Treglia G, Piccardo A, et al. Diagnostic and clinical significance of F-18-FDG-PET/CT thyroid incidentalomas. J Clin Endocrinol Metab. 2012 Nov;97(11):3866-75.
https://academic.oup.com/jcem/article/97/11/3866/2836408
http://www.ncbi.nlm.nih.gov/pubmed/22904176?tool=bestpractice.com
Papillary thyroid carcinoma is the most common malignant histological type in this setting.[12]Bertagna F, Treglia G, Piccardo A, et al. Diagnostic and clinical significance of F-18-FDG-PET/CT thyroid incidentalomas. J Clin Endocrinol Metab. 2012 Nov;97(11):3866-75.
https://academic.oup.com/jcem/article/97/11/3866/2836408
http://www.ncbi.nlm.nih.gov/pubmed/22904176?tool=bestpractice.com
[39]de Leijer JF, Metman MJH, van der Hoorn A, et al. Focal thyroid incidentalomas on (18)F-FDG PET/CT: a systematic review and meta-analysis on prevalence, risk of malignancy and inconclusive fine needle aspiration. Front Endocrinol (Lausanne). 2021;12:723394.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8564374
http://www.ncbi.nlm.nih.gov/pubmed/34744999?tool=bestpractice.com
Clinical examination may be unremarkable, or cervical lymphadenopathy may be palpable. Locally advanced cancer may present with hoarseness due to a paralysed ipsilateral vocal cord, or with dyspnoea or dysphagia. The trachea may be deviated to the opposite side, and the nodule itself may be firm to hard in consistency. Rapid neck enlargement is unusual, but suggests lymphoma (usually in the setting of Hashimoto's thyroiditis), haemorrhage into a nodule, or anaplastic thyroid cancer.[3]Jannin A, Escande A, Al Ghuzlan A, et al. Anaplastic thyroid carcinoma: an update. Cancers (Basel). 2022 Feb 19;14(4):1061.
https://www.mdpi.com/2072-6694/14/4/1061
http://www.ncbi.nlm.nih.gov/pubmed/35205809?tool=bestpractice.com
[5]Stein SA, Wartofsky L. Primary thyroid lymphoma: a clinical review. J Clin Endocrinol Metab. 2013 Aug;98(8):3131-8.
https://academic.oup.com/jcem/article/98/8/3131/2833346
http://www.ncbi.nlm.nih.gov/pubmed/23714679?tool=bestpractice.com
[29]Gharib H, Papini E, Garber JR, et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules - 2016 update. Endocr Pract. 2016 May;22(5):622-39.
https://www.endocrinepractice.org/article/S1530-891X(20)42954-4/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27167915?tool=bestpractice.com
Initial laboratory tests
Thyroid-stimulating hormone (TSH) level should be ordered initially.[1]Haugen BR, Alexander EK, Bible KC, et al; American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2016 Jan;26(1):1-133.
https://www.liebertpub.com/doi/10.1089/thy.2015.0020
http://www.ncbi.nlm.nih.gov/pubmed/26462967?tool=bestpractice.com
If TSH is suppressed, thyroid hormone levels and a radioactive iodine scan are the next steps. The scan may identify a hyperfunctioning (hot) nodule, which is almost always benign.
If TSH is normal or elevated, the next diagnostic step is ultrasound and fine-needle aspiration (FNA) of the thyroid nodule.[1]Haugen BR, Alexander EK, Bible KC, et al; American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2016 Jan;26(1):1-133.
https://www.liebertpub.com/doi/10.1089/thy.2015.0020
http://www.ncbi.nlm.nih.gov/pubmed/26462967?tool=bestpractice.com
Imaging studies and FNA
An ultrasound should be performed in all patients with a thyroid nodule to confirm its presence, and assess size, location, and cystic component(s).[1]Haugen BR, Alexander EK, Bible KC, et al; American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2016 Jan;26(1):1-133.
https://www.liebertpub.com/doi/10.1089/thy.2015.0020
http://www.ncbi.nlm.nih.gov/pubmed/26462967?tool=bestpractice.com
[29]Gharib H, Papini E, Garber JR, et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules - 2016 update. Endocr Pract. 2016 May;22(5):622-39.
https://www.endocrinepractice.org/article/S1530-891X(20)42954-4/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27167915?tool=bestpractice.com
[40]American College of Radiology. ACR-AIUM-SPR-SRU practice parameter for the performance and interpretation of diagnostic ultrasound of the extracranial head and neck. 2022 [internet publication].
https://www.acr.org/-/media/ACR/Files/Practice-Parameters/ExtracranialHeadandNeck.pdf
[41]American College of Radiology. ACR appropriateness criteria: thyroid disease. 2019 [internet publication].
https://acsearch.acr.org/docs/3102386/narrative
Ultrasound evaluation of the cervical lymph nodes should also be performed.[1]Haugen BR, Alexander EK, Bible KC, et al; American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2016 Jan;26(1):1-133.
https://www.liebertpub.com/doi/10.1089/thy.2015.0020
http://www.ncbi.nlm.nih.gov/pubmed/26462967?tool=bestpractice.com
[41]American College of Radiology. ACR appropriateness criteria: thyroid disease. 2019 [internet publication].
https://acsearch.acr.org/docs/3102386/narrative
[42]Zhao H, Li H. Meta-analysis of ultrasound for cervical lymph nodes in papillary thyroid cancer: diagnosis of central and lateral compartment nodal metastases. Eur J Radiol. 2019 Mar;112:14-21.
http://www.ncbi.nlm.nih.gov/pubmed/30777203?tool=bestpractice.com
Most cystic nodules are in fact solid-cystic, for which the risk of malignancy is the same as for solid nodules. However, ultrasound can help to guide aspiration of any solid component. In multi-nodular goitres, FNA of cold (hypofunctioning) nodules should be performed based on features suspicious for malignancy rather than size.[29]Gharib H, Papini E, Garber JR, et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules - 2016 update. Endocr Pract. 2016 May;22(5):622-39.
https://www.endocrinepractice.org/article/S1530-891X(20)42954-4/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27167915?tool=bestpractice.com
FNA of thyroid nodules <1 cm is not recommended unless ultrasound findings are suspicious for malignancy or the patient has a high-risk history.[1]Haugen BR, Alexander EK, Bible KC, et al; American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2016 Jan;26(1):1-133.
https://www.liebertpub.com/doi/10.1089/thy.2015.0020
http://www.ncbi.nlm.nih.gov/pubmed/26462967?tool=bestpractice.com
[29]Gharib H, Papini E, Garber JR, et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules - 2016 update. Endocr Pract. 2016 May;22(5):622-39.
https://www.endocrinepractice.org/article/S1530-891X(20)42954-4/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27167915?tool=bestpractice.com
Ultrasound-based risk stratification systems can be used to inform decisions on when to perform an FNA.[11]Tessler FN, Middleton WD, Grant EG, et al. ACR thyroid imaging, reporting and data system (TI-RADS): white paper of the ACR TI-RADS Committee. J Am Coll Radiol. 2017 May;14(5):587-95.
https://www.jacr.org/article/S1546-1440(17)30186-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/28372962?tool=bestpractice.com
[43]Hoang JK, Middleton WD, Tessler FN. Update on ACR TI-RADS: successes, challenges, and future directions, from the AJR Special Series on Radiology Reporting and Data Systems. AJR Am J Roentgenol. 2021 Mar;216(3):570-8.
https://www.ajronline.org/doi/10.2214/AJR.20.24608
http://www.ncbi.nlm.nih.gov/pubmed/33112199?tool=bestpractice.com
[44]Russ G, Bonnema SJ, Erdogan MF, et al. European Thyroid Association Guidelines for ultrasound malignancy risk stratification of thyroid nodules in adults: the EU-TIRADS. Eur Thyroid J. 2017 Sep;6(5):225-37.
https://pmc.ncbi.nlm.nih.gov/articles/PMC5652895
http://www.ncbi.nlm.nih.gov/pubmed/29167761?tool=bestpractice.com
The American College of Radiology Thyroid Imaging, Reporting, and Data System (ACR TI-RADS) classifies nodules based on ultrasound features as benign, not suspicious, mildly suspicious, moderately suspicious, or highly suspicious for malignancy (TR1 to TR5).[11]Tessler FN, Middleton WD, Grant EG, et al. ACR thyroid imaging, reporting and data system (TI-RADS): white paper of the ACR TI-RADS Committee. J Am Coll Radiol. 2017 May;14(5):587-95.
https://www.jacr.org/article/S1546-1440(17)30186-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/28372962?tool=bestpractice.com
See Classification section. Each risk stratification system has its own guidance on the threshold for FNA.
Reporting of cytology findings in FNA specimens
The Bethesda System for Reporting Thyroid Cytopathology (BSRTC) is commonly used to report FNA cytology findings, and is recommended by the American Thyroid Association.[1]Haugen BR, Alexander EK, Bible KC, et al; American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2016 Jan;26(1):1-133.
https://www.liebertpub.com/doi/10.1089/thy.2015.0020
http://www.ncbi.nlm.nih.gov/pubmed/26462967?tool=bestpractice.com
The Bethesda system includes six diagnostic categories with an implied cancer risk that recommends the next clinical management step.[8]Ali SZ, Baloch ZW, Cochand-Priollet B, et al. The 2023 Bethesda system for reporting thyroid cytopathology. Thyroid. 2023 Sep;33(9):1039-44.
https://www.liebertpub.com/doi/10.1089/thy.2023.0141
http://www.ncbi.nlm.nih.gov/pubmed/37427847?tool=bestpractice.com
See Classification section.
Approximately 70% of thyroid nodules are benign, with only 5% to 10% reported as 'malignant', and with the remainder having an indeterminate diagnosis with risk of malignancy; for this last group, molecular testing is beneficial.[45]Rossi ED, Pantanowitz L, Faquin WC. The role of molecular testing for the indeterminate thyroid FNA. Genes (Basel). 2019 Sep 23;10(10):736.
https://www.mdpi.com/2073-4425/10/10/736
http://www.ncbi.nlm.nih.gov/pubmed/31547603?tool=bestpractice.com
Cytology may identify the thyroid cancer type.[46]Filetti S, Durante C, Hartl DM, et al. ESMO clinical practice guideline update on the use of systemic therapy in advanced thyroid cancer. Ann Oncol. 2022 Jul;33(7):674-84.
https://www.annalsofoncology.org/article/S0923-7534(22)00694-9/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35491008?tool=bestpractice.com
However, for follicular or oncocytic neoplasms, cytology does not distinguish between adenoma (benign) and carcinoma.[47]Ahn HS, Kim HS, Hong MJ. Ultrasonographic and cytologic assessments of follicular neoplasms of the thyroid: predictive features differentiating follicular carcinoma from follicular adenoma. PLoS One. 2022 Jul 21;17(7):e0271437.
https://www.doi.org/10.1371/journal.pone.0271437
http://www.ncbi.nlm.nih.gov/pubmed/35862471?tool=bestpractice.com
[48]McHenry CR, Phitayakorn R. Follicular adenoma and carcinoma of the thyroid gland. Oncologist. 2011;16(5):585-93.
https://academic.oup.com/oncolo/article/16/5/585/6400768?login=false
http://www.ncbi.nlm.nih.gov/pubmed/21482585?tool=bestpractice.com
In these cases, molecular testing or surgery (e.g., lobectomy) to look for capsular or vascular invasion is required to confirm a diagnosis.[29]Gharib H, Papini E, Garber JR, et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules - 2016 update. Endocr Pract. 2016 May;22(5):622-39.
https://www.endocrinepractice.org/article/S1530-891X(20)42954-4/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27167915?tool=bestpractice.com
[49]Cibas ES, Ali SZ. The 2017 Bethesda system for reporting thyroid cytopathology. Thyroid. 2017 Nov;27(11):1341-6.
https://www.liebertpub.com/doi/10.1089/thy.2017.0500
http://www.ncbi.nlm.nih.gov/pubmed/29091573?tool=bestpractice.com
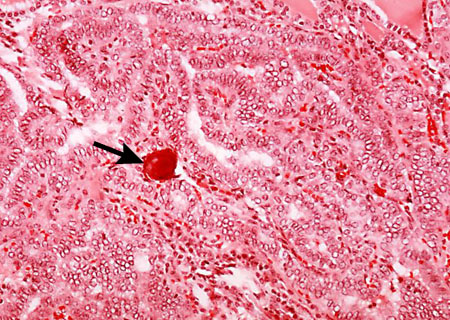
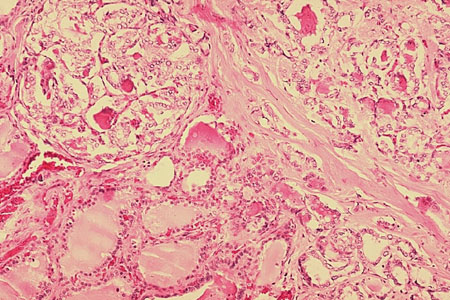
[Figure caption and citation for the preceding image starts]: Histopathology of follicular carcinoma, thyroidCDC Image Library/Dr Edwin P. Ewing, Jr [Citation ends].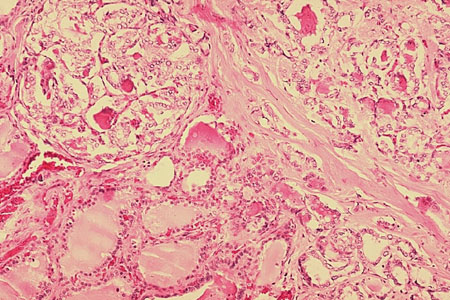 [Figure caption and citation for the preceding image starts]: Histopathology of papillary carcinoma, thyroid: a psammoma body is visible (arrow)CDC Image Library/Dr Edwin P. Ewing, Jr [Citation ends].
[Figure caption and citation for the preceding image starts]: Histopathology of papillary carcinoma, thyroid: a psammoma body is visible (arrow)CDC Image Library/Dr Edwin P. Ewing, Jr [Citation ends].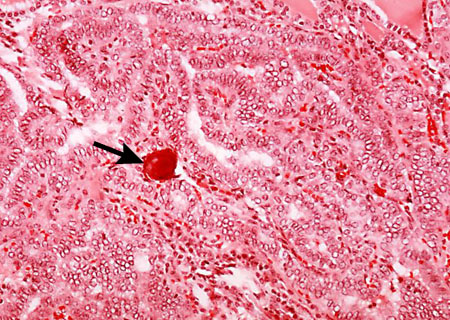
Additional tests to consider
Molecular testing of FNA specimens may be performed to detect genomic mutations/alterations (e.g., BRAF V600, MET, RET/PTC, NTRK, RAS, PAX8::PPARG) to enhance interpretation of indeterminate cytology findings (including follicular or oncocytic neoplasms) and to help guide treatment decisions (e.g., use of targeted therapies).[37]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: thyroid carcinoma [internet publication].
https://www.nccn.org/professionals/physician_gls/default.aspx
If FNA is suspicious for lymphoma, a core biopsy may be used for confirmation.[50]Zhang L, Castellana M, Virili C, et al. Fine-needle aspiration to diagnose primary thyroid lymphomas: a systematic review and meta-analysis. Eur J Endocrinol. 2019 Mar;180(3):177-87.
https://eje.bioscientifica.com/view/journals/eje/180/3/EJE-18-0672.xml
http://www.ncbi.nlm.nih.gov/pubmed/30566902?tool=bestpractice.com
However, core biopsy is not recommended for the initial identification and evaluation of thyroid lesions.[51]Novoa E, Gürtler N, Arnoux A, et al. Role of ultrasound-guided core-needle biopsy in the assessment of head and neck lesions: a meta-analysis and systematic review of the literature. Head Neck. 2012 Oct;34(10):1497-503.
http://www.ncbi.nlm.nih.gov/pubmed/22127851?tool=bestpractice.com
[52]Durante C, Hegedüs L, Czarniecka A, et al. 2023 European Thyroid Association clinical practice guidelines for thyroid nodule management. Eur Thyroid J. 2023 Oct 1;12(5):e230067.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10448590
http://www.ncbi.nlm.nih.gov/pubmed/37358008?tool=bestpractice.com
Serum calcitonin level should be checked if medullary thyroid carcinoma is confirmed or suspected (e.g., on cytology or when there is a family history suggestive of familial medullary cancer or a multiple endocrine neoplasia [MEN] syndrome).[4]Wells SA Jr, Asa SL, Dralle H, et al. Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid. 2015 Jun;25(6):567-610.
https://www.liebertpub.com/doi/10.1089/thy.2014.0335
http://www.ncbi.nlm.nih.gov/pubmed/25810047?tool=bestpractice.com
[37]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: thyroid carcinoma [internet publication].
https://www.nccn.org/professionals/physician_gls/default.aspx
Genetic testing is required for patients with a family history of MEN syndromes or a cytological diagnosis of medullary thyroid cancer.[4]Wells SA Jr, Asa SL, Dralle H, et al. Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid. 2015 Jun;25(6):567-610.
https://www.liebertpub.com/doi/10.1089/thy.2014.0335
http://www.ncbi.nlm.nih.gov/pubmed/25810047?tool=bestpractice.com
[37]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: thyroid carcinoma [internet publication].
https://www.nccn.org/professionals/physician_gls/default.aspx
Almost all patients with MEN type 2A (MEN2A), MEN2B, or isolated familial medullary thyroid cancer have germline RET (REarranged during Transfection) mutations, and around 50% of sporadic medullary thyroid cancers have somatic RET mutations.[4]Wells SA Jr, Asa SL, Dralle H, et al. Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid. 2015 Jun;25(6):567-610.
https://www.liebertpub.com/doi/10.1089/thy.2014.0335
http://www.ncbi.nlm.nih.gov/pubmed/25810047?tool=bestpractice.com
Different types of RET mutation account for different biological behaviour and may guide future management (such as screening for, and treatment of, phaeochromocytoma and hyperparathyroidism).[53]Viola D, Elisei R. Management of medullary thyroid cancer. Endocrinol Metab Clin North Am. 2019 Mar;48(1):285-301.
http://www.ncbi.nlm.nih.gov/pubmed/30717909?tool=bestpractice.com
RAS mutations are present in up to 23% of sporadic medullary thyroid cancer cases.[28]Prete A, Borges de Souza P, Censi S, et al. Update on fundamental mechanisms of thyroid cancer. Front Endocrinol (Lausanne). 2020 Mar 13;11:102.
https://www.frontiersin.org/articles/10.3389/fendo.2020.00102/full
http://www.ncbi.nlm.nih.gov/pubmed/32231639?tool=bestpractice.com
Patients with medullary cancer should undergo pre-operative neck imaging studies (ultrasound, CT) to evaluate cervical lymph node.[4]Wells SA Jr, Asa SL, Dralle H, et al. Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid. 2015 Jun;25(6):567-610.
https://www.liebertpub.com/doi/10.1089/thy.2014.0335
http://www.ncbi.nlm.nih.gov/pubmed/25810047?tool=bestpractice.com
Vocal cord mobility should be examined in patients with voice change/hoarseness.[1]Haugen BR, Alexander EK, Bible KC, et al; American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2016 Jan;26(1):1-133.
https://www.liebertpub.com/doi/10.1089/thy.2015.0020
http://www.ncbi.nlm.nih.gov/pubmed/26462967?tool=bestpractice.com
Laryngoscopy, which may show a paralysed vocal cord, is recommended in patients with pre-operative voice abnormalities and in patients with gross extrathyroidal extension of cancer posteriorly or extensive nodal involvement, even if the voice is normal.[1]Haugen BR, Alexander EK, Bible KC, et al; American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2016 Jan;26(1):1-133.
https://www.liebertpub.com/doi/10.1089/thy.2015.0020
http://www.ncbi.nlm.nih.gov/pubmed/26462967?tool=bestpractice.com
Serum thyroglobulin is useful for post-treatment monitoring of papillary or follicular (including oncocytic) thyroid cancer, but not for diagnosis of thyroid malignancy. It is also useful for predicting future disease-free status before post-operative radioiodine therapy for remnant ablation, whereby low pre-ablation thyroglobulin levels may be considered a favourable risk factor in patients with differentiated thyroid cancer.[54]Webb RC, Howard RS, Stojadinovic A, et al. The utility of serum thyroglobulin measurement at the time of remnant ablation for predicting disease-free status in patients with differentiated thyroid cancer: a meta-analysis involving 3947 patients. J Clin Endocrinol Metab. 2012 Aug;97(8):2754-63.
https://academic.oup.com/jcem/article/97/8/2754/2823340
http://www.ncbi.nlm.nih.gov/pubmed/22639291?tool=bestpractice.com
 [Figure caption and citation for the preceding image starts]: Histopathology of papillary carcinoma, thyroid: a psammoma body is visible (arrow)CDC Image Library/Dr Edwin P. Ewing, Jr [Citation ends].
[Figure caption and citation for the preceding image starts]: Histopathology of papillary carcinoma, thyroid: a psammoma body is visible (arrow)CDC Image Library/Dr Edwin P. Ewing, Jr [Citation ends].