Investigations
1st investigations to order
plasma free metanephrines or 24-hour urine fractionated metanephrines and normetanephrines
Test
Measurement of plasma free metanephrines (also known as metadrenalines), or 24-hour urine fractionated metanephrines and normetanephrines (also known as normetadrenaline), is recommended in patients with suspected phaeochromocytoma.[2][27][43]
Blood sampling should be performed in the supine position.[2][26] Some drugs may interfere with testing results (e.g., buspirone, cocaine, labetalol, levodopa, methyldopa, monoamine oxidase inhibitors [MAOIs], paracetamol, phenoxybenzamine, sotalol, sulfasalazine, sympathomimetics, tricyclic antidepressants); review patient medications accordingly.[2][43]
When measuring 24-hour urinary excretion, creatinine is measured to ensure the adequacy of the collection.
Result
elevations 3 times above the upper limit of normal are diagnostic
genetic testing
Test
All patients with phaeochromocytomas should undergo genetic testing to identify potential hereditary tumour disorders that would necessitate more detailed evaluation and follow-up.[1][2][43] Patient engagement in a shared decision-making process is essential.[2][43]
Genetic testing may be considered in patients with phaeochromocytoma with positive family history (premised upon pedigree or identification of a PPGL-susceptibility gene mutation); syndromic features; multifocal, bilateral, or metastatic disease.[2]
Result
may reveal familial disorders responsible for phaeochromocytoma such as Von Hippel-Lindau syndrome (VHL), multiple endocrine neoplasia type 2 (MEN2), or neurofibromatosis type 1 (NF1); other described gene mutations include SDHB, SDH complex assembly factor 2 (SDHAF2), transmembrane protein 127 (TMEM 127), SDH subunit A, MYC-associated factor X (MAX), and hypoxia-inducible factor 2-alpha (HIF2A)
Investigations to consider
FBC
Test
Erythrocytosis is a rare finding, secondary to overproduction of erythropoietin.[54]
Result
may reveal erythrocytosis
serum calcium
Test
Hypercalcaemia may be seen in patients with multiple endocrine neoplasia 2 (MEN2) who have concomitant primary hyperparathyroidism.
Result
may reveal hypercalcaemia
serum potassium
Test
Hypokalaemia can be seen in the setting of high catecholamines.
Result
may reveal hypokalaemia
chromogranin A
Test
Chromogranin A is an acidic monomeric protein that is stored with and secreted with catecholamine release.
Chromogranin A plus urinary fractionated metanephrines have been suggested as follow-up tests for elevations of plasma metanephrines.[48]
Reported sensitivity of 83% and specificity of 96% for identifying a phaeochromocytoma.[55]
Chromogranin A can be used as a screening tool to detect recurrence, especially in patients with normal preoperative metanephrine and normetanephrine levels.[56]
Result
elevated in patients with phaeochromocytomas and multiple other neuroendocrine tumours
clonidine suppression test
Test
Discriminates patients with mildly elevated test results for plasma normetanephrine (attributable to increased sympathetic activity) from those with elevated test results due to a PPGL.[2]
Used when potential for false-positive urine or serum studies (metanephrines/ normetanephrines) is high (e.g., patients with decreased renal excretory function, in acute alcohol withdrawal, or if the patient is taking hydralazine or minoxidil).
Clonidine is a centrally acting alpha-2-adrenergic receptor agonist that suppresses the release of catecholamines from neurons; however, it does not affect catecholamine secretion from a phaeochromocytoma.
Catecholamine levels are taken both before and after administration of clonidine.[2][57] Consult your local drug information source for guidance on dose.
Result
lack of suppression of catecholamines
CT scan of the abdomen and pelvis
Test
Recommended given its excellent spatial resolution in the abdomen.[2]
Anatomical imaging with computed tomography (CT), magnetic resonance imaging (MRI), or both is critical for surgical planning and should be performed for every patient.[25]
CT can detect adrenal phaeochromocytomas as small as 0.5 cm and extra-adrenal disease >1 cm in diameter.[Figure caption and citation for the preceding image starts]: Abdominal CT scan with mass in the left adrenal gland, compatible with a phaeochromocytomaAlface MM et al. BMJ Case Rep. 2015 Aug 4;2015:bcr2015211184; used with permission [Citation ends].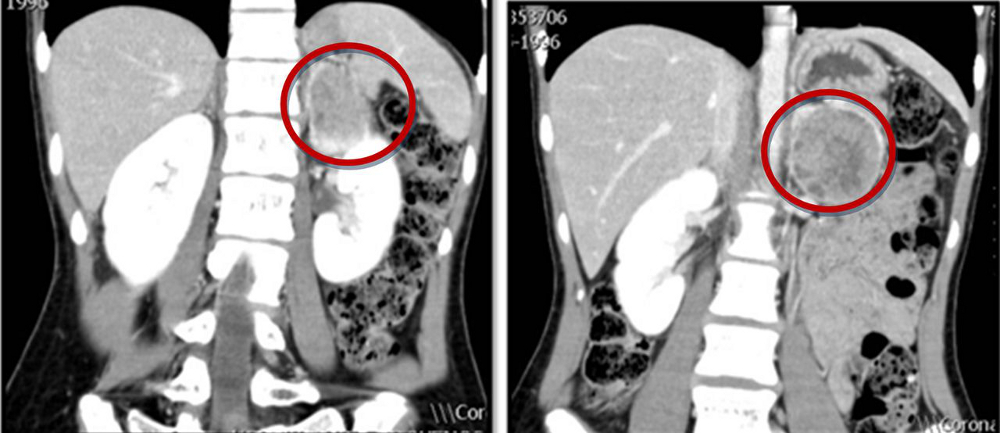
Localisation studies should only be undertaken after a biochemical abnormality is demonstrated.
Result
inhomogeneous masses, often with a central area of low attenuation that represents haemorrhage or necrosis; the attenuation values are greater than 10 HU on unenhanced images
MRI of the abdomen and pelvis
Test
Anatomical imaging (with CT, MRI, or both) is critical for surgical planning and should be performed for every patient.[25]
MRI is an option for patients in whom CT imaging is contraindicated (e.g., children, pregnant women).[2][16] It is recommended in metastatic disease.[2]
Localisation studies should only be undertaken after a biochemical abnormality is demonstrated.
Result
typically appear hyper-intense to the liver on T2-weighted images because of their high water content
I-123 metaiodobenzylguanidine (MIBG) scintigraphy
Test
Guidelines recommend I-123 MIBG imaging in patients with an increased risk for metastatic disease related to a large phaeochromocytoma, patients with recurrent disease, or patients in whom radiotherapy with iobenguane I-131 (also known as I-131 MIBG) is planned.[2][Figure caption and citation for the preceding image starts]: Metaiodobenzylguanidine (MIBG) scintigraphy identified hyperfixation in the left adrenal gland compatible with phaeochromocytomaAlface MM et al. BMJ Case Rep. 2015 Aug 4;2015:bcr2015211184; used with permission [Citation ends].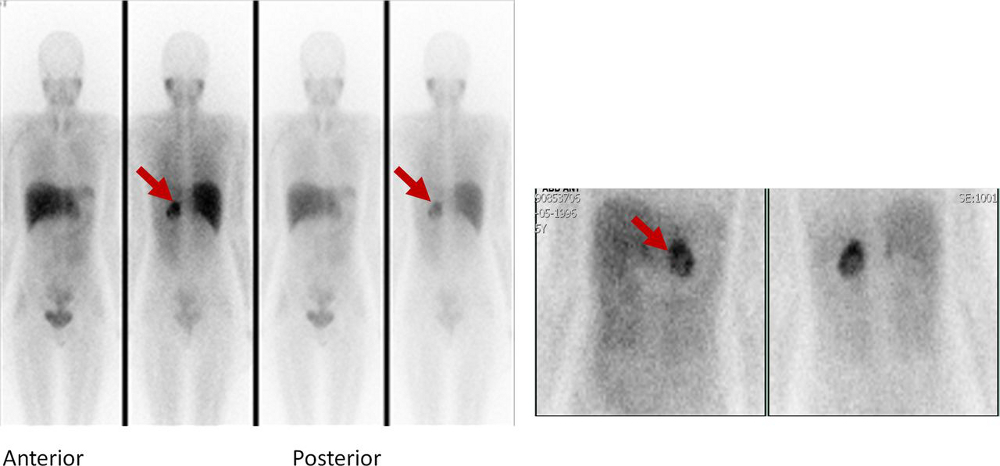
One meta-analysis found I-123 to have both sensitivity and specificity >90% for detection of phaeochromocytoma.[58]
Can be utilised to improve detection when anatomical localisation is inconclusive, to identify additional lesions in the setting of hereditary disease, or to evaluate for metastatic disease.[59]
Result
I-123 MIBG uptake intensity is high in catecholamine-producing tissues
18F-fluoro-2 deoxy-D-glucose (18F-FDG) positron emission tomography (PET)
Test
The use of PET helps to distinguish benign and malignant neuroendocrine tumours.[60]
Performed, as appropriate, in the presence of metastatic or multifocal disease.[43] 18F-FDG PET/CT is preferred to MIBG scintigraphy in this scenario.[2][43]
Can be utilised to improve detection when anatomical localisation is inconclusive, to identify additional lesions in the setting of hereditary disease, or to evaluate for metastatic disease.[59]
Result
uptake of 18F-FDG is high in catecholamine-producing tissues
Use of this content is subject to our disclaimer