Last reviewed: 16 Mar 2025
Last updated: 30 Aug 2024
Summary
Definition
History and exam
Key diagnostic factors
- presence of risk factors
- headache
- palpitations
- diaphoresis
- hypertension
- hypertensive retinopathy
- pallor
- impaired glucose tolerance/diabetes mellitus
- family history of endocrine disorders
- history of prior phaeochromocytoma
- tachyarrhythmias and myocardial infarction
- panic attacks or a 'sense of doom'
Other diagnostic factors
- orthostatic hypotension
- hypercalcaemia
- Cushing syndrome
- diarrhoea
- fever
- papilloedema
- abdominal masses
- tremors
Risk factors
- Multiple endocrine neoplasia type 2 (MEN2)
- Von Hippel-Lindau (VHL) disease
- succinate dehydrogenase (SDH) subunit B, C, and D gene mutations
- neurofibromatosis type 1 (NF1)
Diagnostic investigations
1st investigations to order
- plasma free metanephrines or 24-hour urine fractionated metanephrines and normetanephrines
- genetic testing
Investigations to consider
- FBC
- serum calcium
- serum potassium
- chromogranin A
- clonidine suppression test
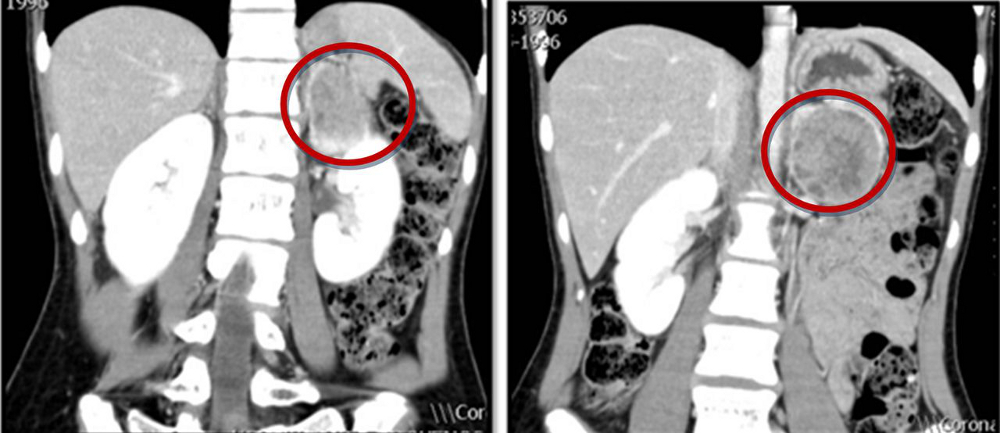
- CT scan of the abdomen and pelvis
- MRI of the abdomen and pelvis
- I-123 metaiodobenzylguanidine (MIBG) scintigraphy
- 18F-fluoro-2 deoxy-D-glucose (18F-FDG) positron emission tomography (PET)
Treatment algorithm
Contributors
Authors
Bridget Sinnott, MD

Professor of Medicine
Medical College of Georgia
Augusta
GA
Disclosures
BS declares that she has no competing interests.
Acknowledgements
Dr Bridget Sinnott would like to gratefully acknowledge Dr Sidhbh Gallagher, a previous contributor to this topic. SG declares that she has no competing interests.
Peer reviewers
Betul A. Hatipoglu, MD
Clinical Endocrinologist and Research Scientist
Department of Endocrinology, Diabetes, and Metabolism
Cleveland Clinic
Cleveland
OH
Disclosures
BAH declares that she has no competing interests.
Use of this content is subject to our disclaimer