Case history
Case history
A 67-year-old man, with a long-standing history of smoking (>100 pack-years), coronary artery disease, chronic renal insufficiency, hypertension, and chronic obstructive pulmonary disease, in his routine follow-up appointment is found to have a haematocrit of 19%. He had a haematocrit of 36% the previous year. He reports fatigue, night sweats, 4.5 kg (10 lb) weight loss, abdominal discomfort, and progressive dyspnoea on exertion. He denies fever, chest pain, or upper or lower gastrointestinal bleeding. On examination, he is cachectic but not in acute distress. His conjunctivae are pale. He has mild-to-moderate hearing loss. There is no lymphadenopathy. Chest examination reveals distant heart sounds with bilateral expiratory wheezes. Cardiac examination reveals no murmurs. Abdominal examination reveals a moderately enlarged spleen without hepatomegaly. There is no peripheral oedema or clubbing. Full blood count shows a white blood cell count of 6.2 × 10⁹/L (6200/microlitre) with an absolute neutrophil count of 2.2 × 10⁹/L (2200/microlitre), an absolute lymphocyte count of 2.4 × 10⁹/L (2400/microlitre), and 0.36 × 10⁹/L monocytes (360 monocytes/microlitre); a haemoglobin (Hb) of 60 g/L (6 g/dL) with a mean corpuscular volume of 86; and a platelet count of 96 × 10⁹/L (96 × 10³/microlitre) and a reticulocyte count of 0.6%, with an absolute reticulocyte count of 14.1 × 10⁹/L (14.1 × 10³/microlitre). Peripheral blood smear shows occasional teardrop-shaped red blood cells, and erythroblasts and myelocytes. Lactate dehydrogenase is 245 U/L. Iron studies, serum B12, and red blood cell folate levels, as well as a serum and urine protein electrophoresis, are within normal limits. Computed tomographic scans of the chest, abdomen, and pelvis reveal moderate mediastinal lymphadenopathy and splenomegaly. Upper gastrointestinal endoscopy and colonoscopy are normal. A bone marrow aspirate is a 'dry tap'. Bone marrow biopsy reveals an entirely fibrotic marrow with a few scattered plasma cells, lymphocytes, and maturing myeloid cells. Megakaryocytes are scattered and sometimes clustered and atypical with large hyperchromic nuclei. Haemoglobin staining reveals a few erythrocyte precursors. A CD34 stain reveals no increase in blasts. Mutation testing is positive for MPL, but negative for JAK2 V617F and calreticulin (CALR).[Figure caption and citation for the preceding image starts]: Peripheral blood smear showing teardrop red blood cells (black arrows), 2 nucleated red blood cells (red arrows), and a myelocyte (blue arrow)From the collection of A. Emadi and J.L. Spivak; used with permission [Citation ends].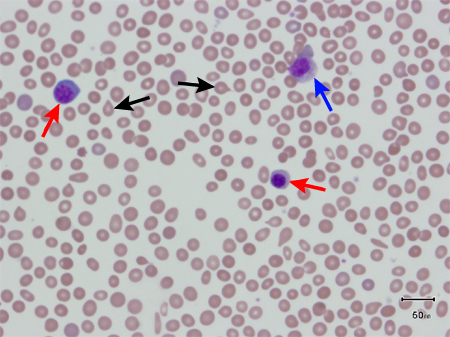
Other presentations
Autoimmune phenomena (e.g., autoimmune thrombocytopenia) are characteristic of primary myelofibrosis.
Use of this content is subject to our disclaimer