Peutz-Jeghers syndrome
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
initially confirmed polyposis: symptomatic or asymptomatic
initial surveillance endoscopy + polyp excision
Small intestinal surveillance is recommended for all patients who meet the diagnostic criteria. This may be performed using video capsule endoscopy (VCE) or magnetic resonance enterography (MRE).
Guidelines differ with regard to the size threshold at which asymptomatic polyps of the small bowel should be removed, although all concur that any symptomatic polyps should be excised regardless of size. US guidelines recommend removal of asymptomatic polyps ≥10 millimetres in diameter, whereas European guidelines recommend a higher threshold of >15-20 millimetres.[13]Latchford A, Cohen S, Auth M, et al. Management of Peutz-Jeghers syndrome in children and adolescents: a position paper from the ESPGHAN Polyposis Working Group. J Pediatr Gastroenterol Nutr. 2019 Mar;68(3):442-52. https://journals.lww.com/jpgn/Fulltext/2019/03000/Management_of_Peutz_Jeghers_Syndrome_in_Children.31.aspx http://www.ncbi.nlm.nih.gov/pubmed/30585892?tool=bestpractice.com [14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com [19]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44. https://gut.bmj.com/content/69/3/411.long http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com [20]van Leerdam ME, Roos VH, van Hooft JE, et al. Endoscopic management of polyposis syndromes: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019 Sep;51(9):877-95. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-0965-0605 http://www.ncbi.nlm.nih.gov/pubmed/31342472?tool=bestpractice.com [22]Wagner A, Aretz S, Auranen A, et al. The management of Peutz-Jeghers syndrome: European Hereditary Tumour Group (EHTG) guideline. J Clin Med. 2021 Jan 27;10(3):473. https://www.mdpi.com/2077-0383/10/3/473/htm http://www.ncbi.nlm.nih.gov/pubmed/33513864?tool=bestpractice.com [33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436 Polypectomy is achieved via upper endoscopy or single or double balloon enteroscopy depending on the location of polyps. One series of 34 patients with small bowel hamartomatous polyposis found that double balloon enteroscopy was successful in more than 80% of patients and had an acceptable margin of safety.[39]Gorospe EC, Alexander JA, Bruining DH, et al. Performance of double-balloon enteroscopy for the management of small bowel polyps in hamartomatous polyposis syndromes. J Gastroenterol Hepatol. 2013 Feb;28(2):268-73. http://www.ncbi.nlm.nih.gov/pubmed/23190124?tool=bestpractice.com Surgery may be required in the presence of neoplasia, or if polyp size or number preclude endoscopic removal. It may also be required in patients with intussusception or small bowel obstruction. Some authorities recommend an attempt to clear the small intestine of polyps during laparotomy by means of intraoperative endoscopy with polypectomy or, for larger polyps, by means of enterotomy. This aggressive approach to the diagnosis and resection of small bowel polyps ('clean sweep') has been associated with a longer interval between subsequent surgeries and a decrease in total operations.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com [35]Oncel M, Remzi FH, Church JM, et al. Benefits of "clean sweep" in Peutz-Jegher's patients. Colorectal Dis. 2004 Sep;6(5):332-5. http://www.ncbi.nlm.nih.gov/pubmed/15335366?tool=bestpractice.com [36]Edwards DP, Khosraviani K, Stafferton R, et al. Long-term results of polyp clearance by intraoperative enteroscopy in the Peutz-Jeghers syndrome. Dis Colon Rectum. 2003 Jan;46(1):48-50. http://www.ncbi.nlm.nih.gov/pubmed/12544521?tool=bestpractice.com [37]Zanoni EC, Averbach M, Borges JL, et al. Laparoscopic treatment of intestinal intussusception in the Peutz-Jeghers syndrome: case report and review of the literature. Surg Laparosc Endosc Percutan Tech. 2003 Aug;13(4):280-2. http://www.ncbi.nlm.nih.gov/pubmed/12960794?tool=bestpractice.com
There are limited data to advise on the size of polyps which merit polypectomy in the stomach or colon.[13]Latchford A, Cohen S, Auth M, et al. Management of Peutz-Jeghers syndrome in children and adolescents: a position paper from the ESPGHAN Polyposis Working Group. J Pediatr Gastroenterol Nutr. 2019 Mar;68(3):442-52.
https://journals.lww.com/jpgn/Fulltext/2019/03000/Management_of_Peutz_Jeghers_Syndrome_in_Children.31.aspx
http://www.ncbi.nlm.nih.gov/pubmed/30585892?tool=bestpractice.com
The US Multi-Society Task Force on Colorectal Cancer is the only organisation to provide a specific recommendation, advising removal of polyps >5 millimetres in diameter and an attempt to remove all polyps if endoscopically feasible.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
Colectomy is sometimes necessary and should be considered if colonoscopic management is difficult and especially if neoplastic change is found in colonic polyps.[4]Syngal S, Brand RE, Church JM, et al; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62.
https://journals.lww.com/ajg/Fulltext/2015/02000/ACG_Clinical_Guideline__Genetic_Testing_and.8.aspx
http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Small bowel hamartomatous polyp identified on capsule endoscopyFrom the collection of Dr Carol A. Burke, used with permission [Citation ends].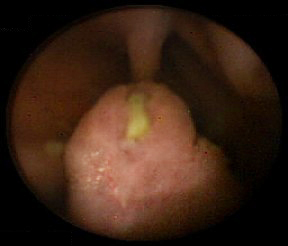 [Figure caption and citation for the preceding image starts]: Polypoid mass in the small bowelFrom the collection of Dr James Church, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Polypoid mass in the small bowelFrom the collection of Dr James Church, used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Characteristic serosal dimpling resulting from a pedunculated hamartoma in the small bowel of a patient with PJSFrom the collection of Dr James Church, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Characteristic serosal dimpling resulting from a pedunculated hamartoma in the small bowel of a patient with PJSFrom the collection of Dr James Church, used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Intra-operative endoscopyFrom the collection of Dr James Church, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Intra-operative endoscopyFrom the collection of Dr James Church, used with permission [Citation ends].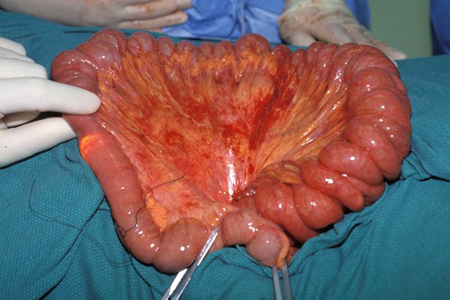 [Figure caption and citation for the preceding image starts]: Hamartomatous polyp harvest following 'clean sweep'From the collection of Dr James Church, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Hamartomatous polyp harvest following 'clean sweep'From the collection of Dr James Church, used with permission [Citation ends].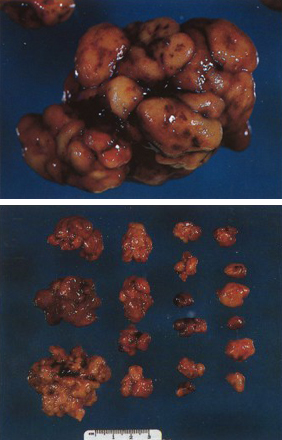
following initial surveillance colonoscopy
ongoing gastrointestinal surveillance ± polyp excision
Endoscopic surveillance is recommended to minimise the risk of complications such as obstruction, bleeding, or cancer. However, data are limited and the outcome on cancer incidence or mortality is unknown.
Surveillance protocols are determined by the risk of gastrointestinal cancer, based upon the presence, number, and size of polyps at index endoscopy; age and family history are also considerations.
Video capsule endoscopy (VCE) or magnetic resonance enterography (MRE) of the small bowel should begin by age 8 years (or earlier if the patient is symptomatic).[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com [19]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44. https://gut.bmj.com/content/69/3/411.long http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com [20]van Leerdam ME, Roos VH, van Hooft JE, et al. Endoscopic management of polyposis syndromes: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019 Sep;51(9):877-95. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-0965-0605 http://www.ncbi.nlm.nih.gov/pubmed/31342472?tool=bestpractice.com [33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436 Capsule endoscopy is safe to use in individuals with PJS and small bowel polyposis who do not have obstructive symptoms. If a concern for capsule retention is present, a patency capsule should be utilised. If no polyps are found at the initial examination, US guidelines recommend that small bowel surveillance should resume at age 18 years and continue every 2-3 years throughout life, whereas European guidelines advise repeating it every 3 years from the outset.[13]Latchford A, Cohen S, Auth M, et al. Management of Peutz-Jeghers syndrome in children and adolescents: a position paper from the ESPGHAN Polyposis Working Group. J Pediatr Gastroenterol Nutr. 2019 Mar;68(3):442-52. https://journals.lww.com/jpgn/Fulltext/2019/03000/Management_of_Peutz_Jeghers_Syndrome_in_Children.31.aspx http://www.ncbi.nlm.nih.gov/pubmed/30585892?tool=bestpractice.com [14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com [19]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44. https://gut.bmj.com/content/69/3/411.long http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com [20]van Leerdam ME, Roos VH, van Hooft JE, et al. Endoscopic management of polyposis syndromes: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019 Sep;51(9):877-95. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-0965-0605 http://www.ncbi.nlm.nih.gov/pubmed/31342472?tool=bestpractice.com [22]Wagner A, Aretz S, Auranen A, et al. The management of Peutz-Jeghers syndrome: European Hereditary Tumour Group (EHTG) guideline. J Clin Med. 2021 Jan 27;10(3):473. https://www.mdpi.com/2077-0383/10/3/473/htm http://www.ncbi.nlm.nih.gov/pubmed/33513864?tool=bestpractice.com [33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Oesophagogastroduodenoscopy (OGD) and colonoscopy to look for upper gastrointestinal and colorectal polyps should be done by age 8 years. If polyps are found, both examinations are repeated every 3 years; if no polyps are detected, a subsequent baseline examination is conducted at age 18 years, and every 3 years thereafter.[13]Latchford A, Cohen S, Auth M, et al. Management of Peutz-Jeghers syndrome in children and adolescents: a position paper from the ESPGHAN Polyposis Working Group. J Pediatr Gastroenterol Nutr. 2019 Mar;68(3):442-52. https://journals.lww.com/jpgn/Fulltext/2019/03000/Management_of_Peutz_Jeghers_Syndrome_in_Children.31.aspx http://www.ncbi.nlm.nih.gov/pubmed/30585892?tool=bestpractice.com [14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com [19]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44. https://gut.bmj.com/content/69/3/411.long http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com
Guidelines differ with regard to the size threshold at which asymptomatic polyps of the small bowel should be removed, although all concur that any symptomatic polyps should be excised regardless of size. US guidelines recommend removal of asymptomatic polyps ≥10 millimetres in diameter, whereas European guidelines recommend a higher threshold of >15-20 millimetres.[13]Latchford A, Cohen S, Auth M, et al. Management of Peutz-Jeghers syndrome in children and adolescents: a position paper from the ESPGHAN Polyposis Working Group. J Pediatr Gastroenterol Nutr. 2019 Mar;68(3):442-52. https://journals.lww.com/jpgn/Fulltext/2019/03000/Management_of_Peutz_Jeghers_Syndrome_in_Children.31.aspx http://www.ncbi.nlm.nih.gov/pubmed/30585892?tool=bestpractice.com [14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com [19]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44. https://gut.bmj.com/content/69/3/411.long http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com [20]van Leerdam ME, Roos VH, van Hooft JE, et al. Endoscopic management of polyposis syndromes: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019 Sep;51(9):877-95. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-0965-0605 http://www.ncbi.nlm.nih.gov/pubmed/31342472?tool=bestpractice.com [22]Wagner A, Aretz S, Auranen A, et al. The management of Peutz-Jeghers syndrome: European Hereditary Tumour Group (EHTG) guideline. J Clin Med. 2021 Jan 27;10(3):473. https://www.mdpi.com/2077-0383/10/3/473/htm http://www.ncbi.nlm.nih.gov/pubmed/33513864?tool=bestpractice.com [33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Polypectomy is achieved via upper endoscopy or single or double balloon enteroscopy depending on the location of polyps. One series of 34 patients with small bowel hamartomatous polyposis found that double balloon enteroscopy was successful in more than 80% of patients and had an acceptable margin of safety.[39]Gorospe EC, Alexander JA, Bruining DH, et al. Performance of double-balloon enteroscopy for the management of small bowel polyps in hamartomatous polyposis syndromes. J Gastroenterol Hepatol. 2013 Feb;28(2):268-73. http://www.ncbi.nlm.nih.gov/pubmed/23190124?tool=bestpractice.com Surgery may be required in the presence of neoplasia, or if polyp size or number preclude endoscopic removal. It may also be required in patients with intussusception or small bowel obstruction. Some authorities recommend an attempt to clear the small intestine of polyps during laparotomy by means of intraoperative endoscopy with polypectomy or, for larger polyps, by means of enterotomy. This aggressive approach to the diagnosis and resection of small bowel polyps ('clean sweep') has been associated with a longer interval between subsequent surgeries and a decrease in total operations.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com [35]Oncel M, Remzi FH, Church JM, et al. Benefits of "clean sweep" in Peutz-Jegher's patients. Colorectal Dis. 2004 Sep;6(5):332-5. http://www.ncbi.nlm.nih.gov/pubmed/15335366?tool=bestpractice.com [36]Edwards DP, Khosraviani K, Stafferton R, et al. Long-term results of polyp clearance by intraoperative enteroscopy in the Peutz-Jeghers syndrome. Dis Colon Rectum. 2003 Jan;46(1):48-50. http://www.ncbi.nlm.nih.gov/pubmed/12544521?tool=bestpractice.com [37]Zanoni EC, Averbach M, Borges JL, et al. Laparoscopic treatment of intestinal intussusception in the Peutz-Jeghers syndrome: case report and review of the literature. Surg Laparosc Endosc Percutan Tech. 2003 Aug;13(4):280-2. http://www.ncbi.nlm.nih.gov/pubmed/12960794?tool=bestpractice.com
There are limited data to advise on the size of polyps which merit polypectomy in the stomach or colon.[13]Latchford A, Cohen S, Auth M, et al. Management of Peutz-Jeghers syndrome in children and adolescents: a position paper from the ESPGHAN Polyposis Working Group. J Pediatr Gastroenterol Nutr. 2019 Mar;68(3):442-52.
https://journals.lww.com/jpgn/Fulltext/2019/03000/Management_of_Peutz_Jeghers_Syndrome_in_Children.31.aspx
http://www.ncbi.nlm.nih.gov/pubmed/30585892?tool=bestpractice.com
The US Multi-Society Task Force on Colorectal Cancer is the only organisation to provide a specific recommendation, advising removal of polyps >5 millimetres in diameter and an attempt to remove all polyps if endoscopically feasible.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
Colectomy is sometimes necessary and should be considered if colonoscopic management is difficult and especially if neoplastic change is found in colonic polyps.[4]Syngal S, Brand RE, Church JM, et al; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62.
https://journals.lww.com/ajg/Fulltext/2015/02000/ACG_Clinical_Guideline__Genetic_Testing_and.8.aspx
http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Small bowel hamartomatous polyp identified on capsule endoscopyFrom the collection of Dr Carol A. Burke, used with permission [Citation ends].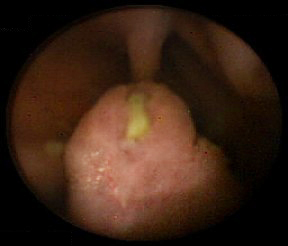
surveillance for associated extra-intestinal malignancy
Treatment recommended for ALL patients in selected patient group
In patients with PJS the lifetime risk for developing cancer of any form is estimated to be up to 93%.[1]van Lier MG, Wagner A, Mathus-Vliegen EM, et al. High cancer risk in Peutz-Jeghers syndrome: a systematic review and surveillance recommendations. Am J Gastroenterol. 2010 Jun;105(6):1258-64. http://www.ncbi.nlm.nih.gov/pubmed/20051941?tool=bestpractice.com Lifetime risks for specific cancers include breast (40% to 85%), pancreas (11% to 36%), ovary (21%), lung (7% to 17%), cervical (10% to 23%), and uterus (9%).[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com Male children and adolescents, and less commonly younger adults, are also at risk for testicular cancer.[16]Giardiello FM, Bresinger JD, Tersmette AC, et al. Very high risk of cancer in familial Peutz-Jeghers syndrome. Gastroenterology. 2000 Dec;119(6):1447-53. http://www.ncbi.nlm.nih.gov/pubmed/11113065?tool=bestpractice.com Surveillance guidelines for extra-intestinal cancers in patients with Peutz-Jeghers syndrome have been published.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com [19]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44. https://gut.bmj.com/content/69/3/411.long http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com [20]van Leerdam ME, Roos VH, van Hooft JE, et al. Endoscopic management of polyposis syndromes: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019 Sep;51(9):877-95. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-0965-0605 http://www.ncbi.nlm.nih.gov/pubmed/31342472?tool=bestpractice.com [33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Breast cancer: The risk of breast cancer in women with PJS is similar to carriers of BRCA1 or BRCA2 mutations (40% to 85% lifetime risk).[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com The US Multi-Society Task Force on Colorectal Cancer advises monthly breast self-examination starting at age 18 years, biannual clinical breast examination starting at age 25 years, annual breast magnetic resonance imaging (MRI) from age 25-29 years, and mammography with consideration of tomosynthesis (3-dimensional mammography) alternating every 6 months with breast MRI with contrast from age 30-75 years.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com The National Comprehensive Cancer Network (NCCN) recommends mammogram and MRI) annually along with a clinical breast examination every 6 months, starting at approximately age 30 years.[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436 Prophylactic mastectomy can be considered on a case-by-case basis.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
Pancreatic cancer: Pancreatic cancer is the third most common malignancy (after breast and colorectal) in people with PJS, with an 11% to 36% lifetime risk of pancreatic ductal adenocarcinoma.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com [33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436 Surveillance via endoscopic ultrasound (EUS) and/or MRI or magnetic resonance cholangiopancreatography (MRCP) is recommended. The International Cancer of the Pancreas Screening Consortium recommends pancreatic imaging every 1-2 years starting from age 40 years.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com [34]Canto MI, Harinck F, Hruban RH, et al. International Cancer of the Pancreas Screening (CAPS) Consortium summit on the management of patients with increased risk for familial pancreatic cancer. Gut. 2013 Mar;62(3):339-47. https://gut.bmj.com/content/62/3/339.long http://www.ncbi.nlm.nih.gov/pubmed/23135763?tool=bestpractice.com The NCCN recommends annual imaging of the pancreas with either EUS or MRI/MRCP beginning at age 30-35 years.[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Gynaecological cancers: The lifetime risks for ovarian, uterine, and cervical cancer are estimated at 21%, 9%, and 10% to 23%, respectively.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com Guidelines differ with regard to the recommended age at which screening with pelvic examination, cervical smear, and transvaginal ultrasound should start, with the NCCN advising a starting age of approximately 18-20 years and other societies a later starting age of 25 years.[4]Syngal S, Brand RE, Church JM, et al; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62. https://journals.lww.com/ajg/Fulltext/2015/02000/ACG_Clinical_Guideline__Genetic_Testing_and.8.aspx http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com [33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436 Almost all ovarian cancers in patients with PJS are sex cord tumours with annular tubules (SCTAT). These tumours can cause irregular menstruation and precocious puberty. Annual physical examination to check for precocious puberty is recommended, starting at age 8 years, as well as yearly pelvic examination and pelvic ultrasound from the age of 18-25 years.[4]Syngal S, Brand RE, Church JM, et al; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62. https://journals.lww.com/ajg/Fulltext/2015/02000/ACG_Clinical_Guideline__Genetic_Testing_and.8.aspx http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com [33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436 For uterine cancer surveillance, annual pelvic examination is recommended from age 18-25 years. The American College of Gastroenterology (ACG) advises annual transvaginal ultrasound beginning at age 25 years.[4]Syngal S, Brand RE, Church JM, et al; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62. https://journals.lww.com/ajg/Fulltext/2015/02000/ACG_Clinical_Guideline__Genetic_Testing_and.8.aspx http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com The NCCN does not recommend routine ultrasound screening, but advises endometrial biopsy in the presence of abnormal bleeding.[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436 A high proportion of cervical cancers in patients with PJS are minimal deviation adenocarcinoma (formerly known as adenoma malignum), a rare, well differentiated adenocarcinoma that is difficult to detect with liquid-based cytology and has a poor prognosis. Guidelines recommend annual pelvic examination and liquid-based cytology from the age of 18-25 years (again, guidelines differ with regard to the age at which this should start).[4]Syngal S, Brand RE, Church JM, et al; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62. https://journals.lww.com/ajg/Fulltext/2015/02000/ACG_Clinical_Guideline__Genetic_Testing_and.8.aspx http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com [14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com [33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436 The NCCN also advocates consideration of total hysterectomy once a woman has completed her family.[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Testicular cancer: Male patients with PJS have a 9% lifetime risk of developing Sertoli cell tumours, with a mean age at diagnosis of 9 years.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com [33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436 Annual testicular examination and observation for feminising changes is recommended, with follow-up testicular ultrasound if abnormalities are detected. The age at which this should start is controversial; the US Multi-Society Task Force on Colorectal Cancer advises screening from birth, whereas the NCCN recommends a higher starting age of approximately 10 years.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com [33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Lung cancer: The estimated lifetime risk of lung cancer in patients with PJS is 7% to 17%.[4]Syngal S, Brand RE, Church JM, et al; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62. https://journals.lww.com/ajg/Fulltext/2015/02000/ACG_Clinical_Guideline__Genetic_Testing_and.8.aspx http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com Guidelines differ in recommendations for surveillance. The US Multi-Society Task Force on Colorectal Cancer and NCCN simply recommend educating patients about symptoms and smoking cessation.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com [33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication]. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436 However, the American College of Chest Physicians, American Society of Clinical Oncology, and American Cancer Society advise low-dose computed tomography (CT) annually from age 55-74 years (based on the level of cumulative risk in patients with PJS, which is similar to people with a more than 30 pack-year history of smoking who have quit for 10-15 years).[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85. https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com The evidence to support these recommendations is not robust. It is the opinion of the authors that surveillance should be individualised based on phenotype, expected age and incidence of disease, and family history.
laser/light therapy for mucocutaneous pigmentation
Additional treatment recommended for SOME patients in selected patient group
Where cosmetic appearance is significant or distressing, mucocutaneous pigmentation may be treated with laser or intense light source therapy.[5]Beggs AD, Latchford AR, Vasen HF, et al. Peutz-Jeghers syndrome: a systematic review and recommendations for management. Gut. 2010 Jul;59(7):975-86. http://www.ncbi.nlm.nih.gov/pubmed/20581245?tool=bestpractice.com [40]Kato S, Takeyama J, Tanita Y, et al. Ruby laser therapy for labial lentigines in Peutz-Jeghers syndrome. Eur J Pediatr. 1998 Aug;157(8):622-4. http://www.ncbi.nlm.nih.gov/pubmed/9727843?tool=bestpractice.com [41]Remington BK, Remington TK. Treatment of facial lentigines in Peutz-Jeghers syndrome with intense pulsed light source. Dermatol Surg. 2002 Nov;28(11):1079-81. http://www.ncbi.nlm.nih.gov/pubmed/12460308?tool=bestpractice.com

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer