Investigations
1st investigations to order
endoscopy
Test
All patients should undergo oesophagogastroduodenoscopy (OGD), colonoscopy, and video capsule endoscopy (VCE) or magnetic resonance enterography (MRE), starting by age 8 years.[13][14][19][20][22] Capsule endoscopy is safe to use in individuals with PJS and small bowel polyposis who lack obstructive symptoms. If a concern for capsule retention is present, a patency capsule should be utilised. In general, adverse events associated with diagnostic EGD are rare (reported rates: infection <0.3%, bleeding <0.1%, cardiopulmonary events <0.1%, perforation <0.01%).[21]
Gastric, small bowel, and colorectal polyposis occur in 88% to 100% of patients, with the majority appearing in the small bowel (60% to 90%) and colon (50% to 64%).[14]
In rare cases, polyps have also occurred in the renal pelvis, urinary bladder, lungs, and nares.
Multiple polyps are typical; usually the total number is <20. Individual polyps vary in size from a few millimetres to several centimetres.
Result
intestinal polyps of variable number
magnetic resonance enterography
Test
All patients should undergo oesophagogastroduodenoscopy (OGD), colonoscopy, and video capsule endoscopy (VCE) or magnetic resonance enterography (MRE), starting by age 8 years.[13][14][19][20][22]
Gastric, small bowel, and colorectal polyposis occur in 88% to 100% of patients, with the majority appearing in the small bowel (60% to 90%) and colon (50% to 64%).[14]
In rare cases, polyps have also occurred in the renal pelvis, urinary bladder, lungs, and nares.
Multiple polyps are typical; usually the total number is <20. Individual polyps vary in size from a few millimetres to several centimetres.
Result
intestinal polyps of variable number
polyp histology
Test
Polyp histology is used to guide diagnosis and genetic testing.[11]
Polyps may be small or large, sessile or pedunculated. They often have a characteristic cerebriform appearance due to smooth muscle arborisation within the polyps. Pathologically, Peutz-Jeghers polyps are unique in that there is an overgrowth of the muscularis mucosae, apparent as arborising bundles of smooth muscle underlying the epithelium. This smooth muscle core is covered by lamina propria and mature glandular epithelium.[Figure caption and citation for the preceding image starts]: Histology of a hamartomatous polypFrom the collection of Dr Carol A. Burke, used with permission [Citation ends].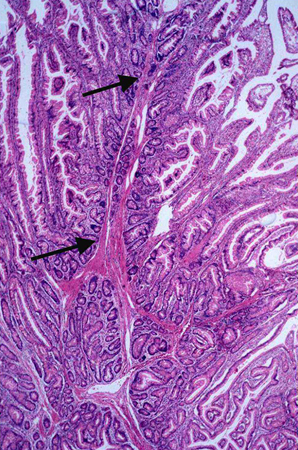
When determining diagnosis or genetic testing strategy, polyps should be reviewed by a dedicated gastrointestinal pathologist, as significant discrepancies have been identified when hamartomatous polyps are re-reviewed.[23]
Result
hamartomatous polyp
STK11 genetic testing
Test
Germline genetic testing (performed on a blood sample) should be utilised to confirm the clinical diagnosis in those patients who satisfy the diagnostic criteria for PJS.[14] Sequencing of STK11 will detect 30% to 69% of mutations, and deletion/duplication analysis will find another 30% of germline alterations.[12][17][18] Detection of a pathogenic variant confirms the diagnosis. A negative result significantly reduces the likelihood that the patient has PJS, although pathogenic variants may be missed. A variant mutation of uncertain significance (VUS) could also be identified.
If a patient has a negative or VUS result on genetic testing and meets the clinical criteria, then he or she should be managed as though they have PJS, or evaluated further for another genetic syndrome.[14]
Result
positive for a deleterious mutation
Use of this content is subject to our disclaimer