Differentials
Common
Hepatitis C virus infection
History
may be history of risk factors, (e.g., intravenous drug use, blood transfusion before 1992 in the US, high-risk sexual history); acute infection: usually asymptomatic, may be fatigue, jaundice; chronic infection: may be asymptomatic, but possible symptoms related to cirrhosis and its complications, such as pruritus, abdominal swelling, haematemesis, melaena, confusion, lethargy, weight loss, weakness, bruising
Exam
early disease: normal examination; late disease with chronic infection: may be jaundice, muscle wasting, gynaecomastia, palmar erythema, spider angiomata, petechiae, ascites, distended abdominal veins, hepatosplenomegaly, signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver tests:
modestly elevated or normal aspartate aminotransferase and alanine aminotransferase
- prothrombin time/INR:
normal; cirrhosis: may be increased
- FBC:
may be normal; cirrhosis: may be low platelet count
- serum hepatitis C virus (HCV) antibody by enzyme immunoassay:
usually positive
More - abdominal ultrasound scan:
non-specific findings
More - non-invasive tests of liver fibrosis with transient elastography:
quantify degree of fibrosis and estimates stage of disease
More
Hepatitis B virus infection
History
may be history of risk factor (e.g., travel to endemic part of the world, high-risk sexual history, intravenous drug use); may have minimal or no symptoms; may have lethargy, nausea, vomiting, abdominal pain; acute presentation (uncommon): worsening jaundice and lethargy, confusion; chronic infection with late complications: pruritus, abdominal swelling, haematemesis, melaena, confusion, lethargy, weight loss, weakness, bruising
Exam
acute infection: usually normal, but may have jaundice, tender hepatomegaly, and if severe: risk of acute liver failure with signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma); chronic infection: may have jaundice, muscle wasting, gynaecomastia, palmar erythema, spider angiomata, petechiae, ascites, distended abdominal veins, hepatosplenomegaly, signs of encephalopathy
1st investigation
- serum liver tests:
aspartate aminotransferase and alanine aminotransferase (ALT) may be elevated or normal, bilirubin and alkaline phosphatase may be elevated, albumin may be low
More - prothrombin time/INR:
normal; cirrhosis or acute liver failure: may be increased
- FBC:
may be normal; cirrhosis: may be low platelet count or microcytic anaemia
More - serum hepatitis B core antibody (IgM + IgG):
acute infection: positive IgM; chronic infection: positive IgG
More - serum HBsAg:
positive
More - serum hepatitis B surface antibody:
positive
More - serum hepatitis B e antigen (HBeAg):
positive
More - serum hepatitis B e antibody:
positive
More - serum hepatitis B virus (HBV) DNA:
undetectable or elevated
More
Other investigations
- abdominal ultrasound:
may show poorly defined margins and coarse, irregular internal echoes
More - liver biopsy:
may be evidence of inflammation or fibrosis depending on level of disease activity
More - non-invasive tests of liver fibrosis with transient elastography:
quantify degree of fibrosis and estimates stage of disease
More
Hepatitis A virus infection
History
may be history of risk factors (e.g., travel to endemic part of the world, close contact with known infected person, known food-borne outbreak), anorexia, nausea, vomiting, diarrhoea, abdominal pain, weight loss
Exam
abdominal tenderness, tender hepatosplenomegaly, lymphadenopathy, jaundice; fulminant infection: worsening jaundice, ascites, signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver tests:
elevated liver enzymes, (predominantly aspartate aminotransferase and alanine aminotransferase); elevated bilirubin (conjugated)
More - prothrombin time/INR:
may be mildly prolonged; more marked prolongation with acute liver failure
- serum urea and creatinine:
elevated in acute liver failure
More - serum anti-hepatitis A virus IgM:
positive
Other investigations
- serum anti-hepatitis A virus IgG:
positive
More
Alcohol-related liver disease
History
excess prolonged alcohol intake, CAGE score >2 (C: Have you ever felt you needed to CUT down on your drinking?, A: Have people ANNOYED you by criticising your drinking?, G: Have you ever felt GUILTY about drinking?, E: Have you ever felt you needed a drink first thing in the morning ('EYE-OPENER') to steady your nerves or get rid of a hangover?), indicative AUDIT-C score; abdominal pain, abdominal distention, pruritus, generalised malaise, weight loss, fatigue, anorexia, withdrawal symptoms; with acute hepatitis: confusion, sudden and rapid onset of symptoms
Exam
cachexia, may smell of alcohol, Dupuytren's contractures; chronic, late signs, or with acute hepatitis: may have jaundice, muscle wasting, gynaecomastia, palmar erythema, spider angiomata, petechiae, scratch marks, ascites, distended abdominal veins, caput medusae, hepatosplenomegaly, signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma), bleeding varices, decreased deep tendon reflexes
1st investigation
- serum liver tests:
aspartate aminotransferase (AST) and alanine aminotransferase (ALT) elevation, bilirubin may be elevated, gamma glutamyl transferase (gamma-GT) may be elevated
More - prothrombin time/INR:
normal; cirrhosis or acute alcoholic hepatitis: may be increased
- FBC:
anaemia, leukocytosis, thrombocytopenia, high mean corpuscular volume, WBC count elevated in acute alcoholic hepatitis
More - serum urea and creatinine:
normal or elevated
- serum electrolytes, magnesium, phosphorus:
normal or low sodium, potassium, magnesium, phosphorus
More - abdominal ultrasound scan:
may show hepatomegaly, fatty liver, liver cirrhosis, liver mass, splenomegaly, ascites, evidence of portal hypertension
Other investigations
- transient elastography:
decreased liver elasticity may show fibrosis/cirrhosis/advanced fibrosis
- upper gastrointestinal endoscopy:
varices may be visualised
- liver biopsy:
findings correlate with severity and stage, steatosis frequently present; alcoholic hepatitis: shows inflammation and necrosis, most prominent in centrilobular region of hepatic acinus with neutrophils and monocytes
More
Paracetamol overdose
History
may be a history of self-harm or of medicating for a painful condition; early presentation: may be asymptomatic, nausea, vomiting, abdominal pain; later presentation: jaundice, nausea, vomiting, right upper quadrant pain; risk of acute liver failure with onset of encephalopathy, may progress to confusion and coma
Exam
early presentation: examination may be normal; later presentation: may have right upper quadrant tenderness, jaundice, evidence of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma), poor urine output
1st investigation
- serum liver tests:
predominant alanine aminotransferase and aspartate aminotransferase elevation, depending on time from ingestion
- serum paracetamol levels:
may be positive
More - prothrombin time/INR:
may be increased
More - arterial pH and lactate:
acidaemia may be present; lactate level may be elevated
More - serum urea and creatinine:
may be elevated creatinine and electrolyte abnormalities if renal impairment present
More
Non-paracetamol medications or dietary supplements
History
history of a drug taken either at normal doses or in overdose; possible examples include antiretroviral therapy (ART), amiodarone, non-steroidal anti-inflammatory drugs, chlorpromazine, halothane, oestrogenic or anabolic corticosteroids, including oral contraceptives, trimethoprim/sulfamethoxazole, isoniazid, ketoconazole, methotrexate, sodium valproate, statins, herbal supplements, dietary supplements, tyrosine kinase inhibitors (e.g., pazopanib), bile salt export pump inhibitors (e.g., bosentan, ciclosporin); alcoholism; fever; hepatitis (viral or toxic); vascular insult; chronic liver diseases; and reduced glutathione stores
Exam
early presentation: examination may be normal; later presentation: may have right upper quadrant tenderness, jaundice, evidence of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma), poor urine output
1st investigation
- serum liver tests:
predominant alanine aminotransferase and aspartate aminotransferase elevation
- prothrombin time/INR:
may be increased
More - arterial pH and lactate:
acidaemia may be present; lactate level may be elevated
More - serum urea and creatinine:
may be elevated creatinine and electrolyte abnormalities if renal impairment present
More - serum salicylate level:
may be positive or negative
More - urine drug screen:
may be positive or negative
More - serum paracetamol levels:
may be positive
More
Other investigations
Metabolic dysfunction-associated steatotic liver disease
History
often asymptomatic, may be obese, history of diabetes mellitus, hypertension, high triglyceride level, low HDL cholesterol, cardiac disease, sleep apnoea; dull right upper quadrant discomfort
Exam
hypertension, acanthosis nigricans, striae, central obesity, jaundice; end-stage diagnosis: may have muscle wasting, gynaecomastia, palmar erythema, spider angiomata, petechiae, scratch marks, ascites, distended abdominal veins, hepatosplenomegaly, signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver tests:
may be normal or elevated alanine aminotransferase (ALT) and aspartate aminotransferase (AST), bilirubin elevated in decompensated disease, alkaline phosphatase may be elevated up to twice the upper limit of normal
More - prothrombin time/INR:
may be normal; cirrhosis: may be elevated
- FBC:
initially normal; thrombocytopenia often occurs with cirrhosis
- metabolic panel:
abnormal
More - lipid panel:
elevated total cholesterol, LDL, triglyceride; low HDL
More - abdominal ultrasound:
hypoechoic areas (ovoid, round, or linear) within a hyperechoic (bright) liver; perihilar sparing frequently seen
More
Other investigations
- abdominal CT scan with contrast:
low liver attenuation; no mass effect or contour deformation, intrahepatic vessels follow normal course through fatty lesions, without deformity
More - abdominal MRI:
T1-weighted images: areas of fatty infiltration with increased signal intensity
More - liver biopsy:
demonstrates macrovesicular steatosis, occasional Mallory hyaline bodies, balloon cells, lobular inflammation, perisinusoidal fibrosis
More - simple liver test-based algorithms:
risk stratification of patients by severity of fibrosis
More - transient elastography:
decreased liver elasticity; may show fibrosis/cirrhosis/advanced fibrosis
More
Gilbert's syndrome
History
asymptomatic, incidental finding; or mild jaundice symptoms starting in adolescence or young adult age; fasting accentuates increase in jaundice, as may nicotinic acid (niacin) use
Exam
may be normal, or jaundice present
1st investigation
Other investigations
- fasting bilirubin test:
2- to 3-fold elevation (usually <6-fold rise) in unconjugated bilirubin
More - urine test for bilirubinuria:
negative
- genetic testing:
homozygous for TATA gene A(TA7)TAA alleles
Haemochromatosis
History
usually asymptomatic, may be positive family history of liver disease, skin pigmentation, joint pain or discomfort, cardiac disease, anorexia, diabetes mellitus, especially in advanced disease
Exam
frequently normal examination, joint swelling, signs of cardiac disease and/or diabetes mellitus, bronze skin; advanced disease: may have jaundice, muscle wasting, gynaecomastia, palmar erythema, spider angiomata, petechiae, ascites, distended abdominal veins, hepatosplenomegaly, signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver tests:
may be normal, or non-specific pattern of abnormalities
- prothrombin time/INR:
normal, may be increased with portal hypertension and cirrhosis
- FBC:
may be normal; cirrhosis/portal hypertension: low platelet count
- serum iron and total iron binding capacity:
elevated serum iron, low total iron binding capacity
- serum transferrin saturation test:
>45%
More - serum ferritin:
high (>450 picomols/L [>200 nanograms/mL] in pre-menopausal women, >675 picomols/L [>300 nanograms/mL] in men and post-menopausal women)
More
Choledocholithiasis
History
pruritus, colicky right upper quadrant or epigastric pain after meals, nausea, fatigue, anorexia, pale stool, dark urine
Exam
right upper quadrant abdominal tenderness, may be jaundice, fever
1st investigation
- serum liver tests:
elevated alkaline phosphatase and conjugated bilirubin
- prothrombin time/INR:
may be increased
- FBC:
infection in obstructed biliary tree: elevated WBC count
- abdominal ultrasound scan:
biliary dilation with stone(s) in bile duct
More
Other investigations
- serum lipase and amylase:
elevated (>3 times upper limit of normal) in acute pancreatitis
More - abdominal CT scan:
biliary dilation with stone(s) in bile duct
More - endoscopic ultrasound scan:
stone(s) in bile duct
More - magnetic resonance cholangiopancreatography (MRCP):
stone(s) in bile duct
More - endoscopic retrograde cholangiopancreatography (ERCP):
stone(s) in bile duct
More
Uncommon
Hepatitis E
History
may be history of risk factors (e.g., consumption of undercooked pork products, travel to Southeast Asia, northern and central Africa, India, and Central America), anorexia, nausea and vomiting, diarrhoea, abdominal pain, weight loss, pregnancy
Exam
abdominal tenderness, tender hepatosplenomegaly, lymphadenopathy, jaundice, ascites, signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver tests:
elevation predominantly of aspartate aminotransferase, alanine aminotransferase and bilirubin (conjugated)
- prothrombin time/INR:
normal, may be increased
More - serum anti-hepatitis E virus IgM:
positive
Other investigations
- hepatitis E virus polymerase chain reaction:
positive
Hepatitis D
History
requires co-infection with hepatitis B virus; may be history of risk factors (e.g., high-risk sexual history, intravenous drug use), minimal or no symptoms; acute presentation (uncommon): jaundice, lethargy, confusion; chronic infection with late complications: itching, abdominal swelling, haematemesis, melaena, confusion, lethargy, weight loss, weakness, bruising, mild hepatitis, acute liver failure
Exam
usually normal, but if severe acute infection may be jaundice, tender hepatomegaly, signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma); chronic, late infection: may be jaundice, muscle wasting, gynaecomastia, palmar erythema, spider angiomata, petechiae, ascites, distended abdominal veins, hepatosplenomegaly, signs of encephalopathy
1st investigation
- serum liver tests:
aspartate aminotransferase and alanine aminotransferase may be elevated; bilirubin may be elevated
- prothrombin time/INR:
normal, may be increased
- hepatitis D virus (HDV) antigen:
may be positive
- HDV RNA:
positive
More - anti-HDV antibody:
positive
More - serum hepatitis B core antibody (IgM):
positive
- serum HBsAg:
positive
More - serum hepatitis B e antigen (HBeAg):
may be positive
More
Other investigations
- abdominal ultrasound:
non-specific changes
More
Epstein-Barr virus infection
History
generally adolescents and younger adults, sick contact, fever, malaise, sore throat, myalgia
Exam
cervical or generalised lymphadenopathy, fever, pharyngitis, rash (e.g., maculopapular, itchy rash following amoxicillin, ampicillin, or beta-lactam antibiotic therapy), hepatomegaly, splenomegaly, jaundice (rare)
1st investigation
- serum liver test:
predominant elevations of aspartate aminotransferase and alanine aminotransferase
- FBC:
lymphocytosis, atypical lymphocytes
- heterophile antibodies:
positive
- Epstein-Barr virus (EBV)-specific antibodies:
positive
Other investigations
- real-time PCR:
detection of EBV DNA
More - abdominal ultrasound scan:
enlarged spleen
Herpes simplex virus infection
History
generally adolescents and younger adults, sick contact, fever, malaise, oral or other mucosal ulcerations or lesions, sore throat, myalgia, immunosuppression, pregnancy
Exam
cervical or generalised lymphadenopathy, fever, pharyngitis, rash (oral or mucosal vesicular rash or ulcerations), right upper quadrant tenderness, hepatomegaly, splenomegaly, jaundice (rare)
1st investigation
- serum liver tests:
predominant elevations of aspartate aminotransferase and alanine aminotransferase
- FBC:
lymphocytosis
- herpes simplex virus (HSV) IgM:
positive
- HSV DNA:
positive
Other investigations
- liver biopsy:
haemorrhagic necrosis, viral cytopathic effects and inclusions, positive HSV immunostain
Cytomegalovirus infection
History
immunocompetent people: may be asymptomatic, fever, sore throat; immunocompromised people (e.g., with AIDS or solid organ or bone marrow transplant): more severe symptoms, including fever, headache, cough, chest pain, shortness of breath, lethargy, malaise, vomiting, diarrhoea, abdominal pain, floaters in vision, blindness
Exam
may have normal examination, or lymphadenopathy, splenomegaly; immunocompromised people may also have areas of infarction and haemorrhage on funduscopy
1st investigation
- serum liver test:
predominant elevations of aspartate aminotransferase and alanine aminotransferase
- FBC:
immunocompetent people: lymphocytosis, atypical lymphocytes; immunocompromised people: may be anaemia, leukopenia, thrombocytopenia
- cytomegalovirus (CMV) serology:
IgM elevated in acute infection; IgG elevated if past infection
More - nucleic acid detection (blood or tissue sample):
positive
More - viral culture (blood or tissue sample):
virus may or may not be detected
More
Other investigations
- pp65 antigenaemia:
quantitative result showing number of pp65-positive cells/150,000-200,000 cells
More - liver biopsy:
demonstration of CMV-specific cytoplasmic and intranuclear inclusions
HIV infection
History
variable depending on stage of disease, may have risk factors for HIV infection (e.g., intravenous drug use, HIV-infected blood transfusion, homosexual or heterosexual unprotected sexual intercourse with HIV-infected partner), night sweats, fevers, skin rashes, oral ulceration, diarrhoea, abdominal pain, genitourinary symptoms, headaches
Exam
variable depending on stage of the disease; may be lymphadenopathy, skin rashes (e.g., Kaposi's sarcoma, herpes zoster lesions), oral thrush, hairy leukoplakia, hepatomegaly, splenomegaly, retinal lesions, jaundice, muscle wasting, gynaecomastia, palmar erythema, spider angiomata, petechiae, ascites, distended abdominal veins, signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver tests:
may be normal; predominant aspartate aminotransferase and alanine aminotransferase elevation or predominant alkaline phosphatase elevation
More - FBC:
may be normal, or may be anaemia or thrombocytopenia
- serum HIV enzyme-linked immunosorbent assay (ELISA):
positive
More - serum HIV rapid test:
positive
- HIV non-invasive tests (e.g., saliva sample):
positive
- serum hepatitis B serology:
positive in presence of hepatitis B co-infection
- serum hepatitis C serology:
positive in presence of hepatitis C co-infection
Other investigations
- serum Western blot:
positive
More - serum p24 antigen:
positive
More - CD4 cell count:
count >0.5 x 10⁹/L (>500 cells/microlitre): patients usually asymptomatic; count <0.35 x 10⁹/L (<350 cells/microlitre): implies substantial immune suppression; count <0.2 x 10⁹/L (<200 cells/microlitre): increased risk of opportunistic infections
More
Sepsis
History
fever, chills, confusion, collapse, shortness of breath; may have risk factor for sepsis (e.g., underlying malignancy, age >65 years, haemodialysis, alcoholism, diabetes mellitus)
Exam
high or low temperature, tachycardia, tachypnoea, hypotension, may have evidence of source of infection (e.g., cellulitis, peritonitis), abdominal tenderness, jaundice; with liver failure may develop signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, rigidity, coma), high APACHE (intensive care unit disease severity rating) score
1st investigation
- serum liver test:
marked elevation of liver enzymes, predominantly aspartate aminotransferase and alanine aminotransferase; bilirubin may be elevated
- FBC:
WBC count >12 x 10⁹/L (>12,000/microlitre) or <4 x 10⁹/L (<4000/microlitre); low platelets
- clotting screen:
elevated prothrombin time, elevated partial thromboplastin time, elevated D-dimer, and elevated fibrinogen
- blood culture:
may be positive for infecting organism
- ABG:
low PaO2, elevated PaCO2
- lactate levels:
hyperlactataemia: 2 to 5 mmol/L (18 to 45 mg/dL); shock: ≥4 mmol/L( ≥36 mg/dL)
- serum urea and creatinine:
elevated
- blood glucose:
may be abnormal
Other investigations
- urine microscopy and culture:
may be positive for infecting organism
- sputum culture:
may be positive for infecting organism
- CXR:
may show consolidation, pleural effusion, cardiac abnormalities, or a pneumothorax
Extrapulmonary tuberculosis
History
may have risk factors (e.g., exposure to tuberculosis [TB] infection; from Asia, Africa, or Latin America; HIV infection, immunosuppressive medication, malignancy, renal failure, apical fibrosis on CXR, extremely young age), may have fever, anorexia, night sweats, bone pain, pleuritic chest pain, cough, abdominal swelling
Exam
signs may be variable, including hepatomegaly, splenomegaly, jaundice, ascites
1st investigation
- serum liver test:
normal, may be elevated alkaline phosphatase
- FBC:
may be leukocytosis (without left shift) and anaemia; may be elevated monocyte and eosinophil counts, lymphopenia, or pancytopenia
- sputum acid-fast bacilli smear and culture:
presence of acid-fast bacilli (Ziehl-Neelsen stain) in specimen. Testing of 3 specimens (minimum 8 hours apart, including an early morning specimen) is recommended in many countries; consult local guidance[100]
More - chest x-ray:
consolidation, pulmonary infiltrates, mediastinal or hilar lymphadenopathy, upper zone fibrosis
More - liver biopsy, acid-fast bacilli smear, and culture of biopsy specimen:
granulomas on histology; AFB smear and culture positive
More - nucleic acid amplification tests (NAAT):
positive for M tuberculosis
More
Toxins
History
exposure to poisons such as mushrooms (e.g., Amanita phalloides), herbal preparations (e.g., cascara, chaparral, comfrey, kava, ma huang), or industrial chemicals (e.g., carbon tetrachloride, trichloroethylene, paraquat)
Exam
early presentation: examination may be normal; later presentation: may have right upper quadrant tenderness, jaundice, evidence of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma), poor urine output
1st investigation
- serum liver tests:
predominant aspartate aminotransferase and alanine aminotransferase elevation
- prothrombin time/INR:
may be increased
- serum urea and creatinine:
may be elevated creatinine and electrolyte abnormalities if renal impairment present
- toxicology screen:
may be positive
More
Other investigations
Alpha-1 antitrypsin deficiency
History
family history of liver or pulmonary disease, abdominal pain, pruritus, generalised malaise, weight loss, fatigue, anorexia, pale stool, dark urine; symptoms of emphysema, especially at young age without other risk factors
Exam
signs of necrotising panniculitis; may have jaundice, muscle wasting, gynaecomastia, palmar erythema, spider angiomata, petechiae, ascites, distended abdominal veins, hepatosplenomegaly, signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver tests:
elevated or normal aspartate aminotransferase and alanine aminotransferase; alkaline phosphatase normal
- prothrombin time/INR:
may be increased
- FBC:
may be normal; cirrhosis: low platelet count
- abdominal ultrasound:
non-specific changes
- alpha-1 antitrypsin (AAT) phenotyping:
presence of Z or M alleles
More - plasma alpha-1 antitrypsin level:
reduced plasma level <20 micromol/L
More
Other investigations
- CXR:
emphysematous changes may be present
- chest CT scan:
emphysematous changes may be present
Wilson's disease
History
family history may be positive; symptoms emerging in childhood, adolescence, or early adulthood; tremor, slurred speech, abdominal pain, pruritus, generalised malaise, weakness, weight loss, anorexia, pale stools, dark urine, irritability, depression, easy bruising
Exam
Kayser-Fleischer rings, parkinsonian-like tremor, rigidity, clumsy gait, poor balance, impaired coordination, abnormal postures, repetitive movements, bradykinesia (tongue, lips, and jaw), dysarthria, dysphonia (hoarse voice), inappropriate and uncontrollable grinning (risus sardonicus), drooling, hypermelanotic pigmentation, bruises, signs of dementia and/or psychosis, jaundice, hepatosplenomegaly[78]
1st investigation
- serum liver tests:
may be normal, elevated aspartate aminotransferase, alanine aminotransferase, direct bilirubin; alkaline phosphatase normal or below normal; alkaline phosphatase (ALP):bilirubin ratio of <4 has a high sensitivity and specificity for diagnosing acute liver failure secondary to Wilson's disease[65]
- prothrombin time/INR:
may be increased
- FBC:
may be normal; cirrhosis: low platelet count
- abdominal ultrasound:
non-specific
- serum ceruloplasmin:
decreased
More - 24-hour urinary copper excretion:
elevated
More - slit-lamp ophthalmological examination:
Kayser-Fleischer rings present in Wilson's disease
Autoimmune hepatitis
History
most likely female (female-to-male ratio is 3.6:1), may have history of other autoimmune disease; may be asymptomatic, or have abdominal pain, fatigue, arthralgias, nausea, and vomiting; with acute liver failure: lethargy, confusion, worsening jaundice
Exam
normal, or manifestation of other autoimmune disease; some have features of advanced liver disease: jaundice, muscle wasting, gynaecomastia, palmar erythema, spider angiomata, petechiae, ascites, distended abdominal veins, signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver tests:
severe disease: alanine aminotransferase >7 times upper limit of normal (or 5 times if gamma-globulin markedly elevated), other enzymes and bilirubin may be elevated
More - prothrombin time/INR:
increased in acute liver failure and in patients with cirrhosis
- FBC:
low WBC count and platelets suggest cirrhosis
- antinuclear antibody:
positive
More - anti-smooth muscle antibodies:
positive in type 1 disease
- anti-liver-kidney microsome 1 antibody:
positive in type 2 disease
- liver biopsy:
demonstrates interface hepatitis, predominance of plasmacytic inflammatory infiltrate, bridging necrosis, fibrosis, lobular collapse
More
Other investigations
- serum immunoglobulins:
IgG 3-6 g/dL
More - abdominal ultrasound scan:
variable
More - abdominal CT scan:
abnormal contrast enhancement, irregular nodular liver (cirrhosis)
More - endoscopic retrograde cholangiopancreatography (ERCP):
stenosis or obstruction may be demonstrated
More - magnetic resonance cholangiopancreatography (MRCP):
stenosis or obstruction may be demonstrated
More
Primary biliary cholangitis
History
most commonly women (female-to-male ratio 9:1), may be family history of primary biliary cholangitis or other autoimmune disease, may be personal history of other autoimmune disease (e.g., Sjogren's syndrome, scleroderma, coeliac disease, thyroid disease), pruritus, excoriations, malaise, pigmentation; abdominal pain may be present but most commonly absent; hyperlipidaemia, weight loss, dark urine, keratoconjunctivitis; advanced disease: weight loss, abdominal swelling, confusion
Exam
may be normal apart from skin excoriations and periorbital xanthelasma; may have tendon xanthomas, skin hyperpigmentation, hepatosplenomegaly, right upper quadrant pain; late disease: proximal limb muscle wasting, oedema, varices, jaundice, muscle wasting, gynaecomastia, palmar erythema, spider angiomata, petechiae, ascites, distended abdominal veins, hepatosplenomegaly, signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver tests:
elevated alkaline phosphatase; direct bilirubin elevated in late disease
- prothrombin time/INR:
may be increased in patients with cirrhosis
- FBC:
may be normal; cirrhosis: low platelet count
- serum anti-mitochondrial antibody (AMA) (by immunofluorescence or enzyme-linked immunosorbent assay [ELISA]):
positive
More - liver biopsy:
florid bile duct lesion (especially in early disease) with granuloma formation; ductopenia also occurs
More
Primary sclerosing cholangitis
History
more commonly men (male-to-female ratio 2:1), often asymptomatic, may be history of ulcerative colitis or Crohn's disease, itching, abdominal pain, fatigue, weight loss, chills, night sweats, pale stools, abdominal swelling
Exam
may be normal, excoriations, cachexia, fever, ascites, hepatosplenomegaly, jaundice, muscle wasting, gynaecomastia, palmar erythema, spider angiomata, petechiae, ascites, distended abdominal veins, signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver tests:
elevated alkaline phosphatase, may be mild elevations of aspartate aminotransferase and alanine aminotransferase, elevated direct bilirubin in advanced disease or with a dominant stricture
- prothrombin time/INR:
may be increased in patients with cirrhosis or advanced disease
- FBC:
may be normal; cirrhosis: low platelet count
- perinuclear anti-neutrophilic cytoplasmic antibody:
may be positive
More - abdominal ultrasound:
non-specific changes, demonstration of bile-duct dilation uncommon unless dominant stricture or cholangiocarcinoma is present
- magnetic resonance cholangiopancreatography (MRCP):
normal or multi-focal intrahepatic and/or extrahepatic strictures and dilations ± dominant biliary stricture
More
Other investigations
- anti-mitochondrial antibody:
negative
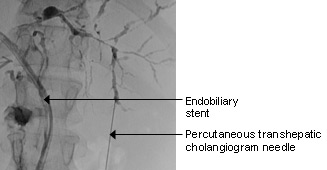
More - endoscopic retrograde cholangiopancreatography (ERCP):
normal or multi-focal intrahepatic and/or extrahepatic strictures and dilations ± dominant biliary stricture
More - histology of brushings from ERCP:
abnormal cells if malignancy co-exists
- liver biopsy:
fibrosis and strictures demonstrated, ‘onion skin’ fibrosis is pathognomic
More
Hepatocellular carcinoma (HCC)
History
may be prior history of liver disease (cirrhosis), may be asymptomatic, increasing abdominal swelling, weight loss, fatigue, presence of hepatitis B or hepatitis C viral infection, alcohol or tobacco use, history of non-alcoholic fatty liver disease
Exam
hepatomegaly, signs of haemochromatosis or other liver diseases, may have jaundice, muscle wasting, gynaecomastia, palmar erythema, spider angiomata, petechiae, ascites, distended abdominal veins, hepatosplenomegaly, signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver tests:
elevated alkaline phosphatase and bilirubin; aspartate aminotransferase and alanine aminotransferase may be normal or elevated
More - prothrombin time/INR:
may be increased in patients with cirrhosis
- alpha-fetoprotein (AFP):
may be elevated
More - abdominal ultrasound scan:
demonstrates a liver mass
More
Other investigations
- alpha-fetoprotein L3:
elevated
More - abdominal multiphasic contrast CT scan:
typical hypervascular pattern, arterial phase enhancement of liver lesions
More - abdominal dynamic contrast MRI:
high-intensity pattern on T2-weighted images, and a low-intensity pattern on T1-weighted images on MRI
More - image-guided liver biopsy:
well-differentiated to poorly differentiated hepatocytes, large multi-nucleated giant cells with central necrosis
More
Liver metastases
History
may be a history of colon, breast, lung, or other cancer, or symptoms referable to primary tumour; variable presentation with increasing abdominal swelling, weight loss, fatigue
Exam
hepatomegaly, signs of other malignancies, may have jaundice, muscle wasting, gynaecomastia, palmar erythema, spider angiomata, petechiae, ascites, distended abdominal veins, hepatosplenomegaly, signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion; asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver tests:
elevated alkaline phosphatase and bilirubin, aspartate aminotransferase and alanine aminotransferase may be normal or elevated
- prothrombin time/INR:
may be increased
- abdominal ultrasound scan:
liver mass(es)
- CT scan (chest and abdomen):
abnormal liver mass(es) demonstrated, may also demonstrate primary tumour and other sites of metastases
Other investigations
- liver biopsy:
confirms metastatic tissue
More
Pancreatic cancer
History
may be family history of pancreatic cancer, may be other risk factors (e.g., smoking, hereditary cancer syndromes, prior history of alcohol excess), sudden onset of jaundice with pruritus, epigastric pain radiating into back may occur, generalised malaise, weight loss, fatigue, low mood
Exam
jaundice, abdominal mass in the epigastrium, hepatomegaly, positive Courvoisier's sign (painless palpable gallbladder with jaundice), or signs of disseminated intravascular coagulation (petechiae, purpura, bruising), cachexia
1st investigation
- serum liver tests:
high direct bilirubin, elevated alkaline phosphatase, aspartate aminotransferase and alanine aminotransferase may be normal or elevated
- prothrombin time/INR:
may be increased
- abdominal ultrasound scan:
may show biliary dilation (intra- and extrahepatic), pancreatic mass, or liver metastases
More - abdominal CT scan:
biliary dilation (intra- and extrahepatic) with possible mass
More
Other investigations
- magnetic resonance cholangiopancreatography (MRCP):
biliary dilation (intra- and extrahepatic) with extrahepatic mass causing obstruction/stricture
More - endoscopic ultrasound scan:
biliary dilation (intra- and extrahepatic) with extrahepatic mass causing obstruction/stricture
More - endoscopic retrograde cholangiopancreatography (ERCP):
biliary dilation (intra- and extrahepatic) with extrahepatic mass causing obstruction/stricture
More - fluorodeoxyglucose-positron emission tomography/CT (FDG-PET/CT):
may demonstrate a mass in the pancreas and the extent of local or distant spread
More
Cholangiocarcinoma
History
may be prior history of inflammatory bowel disease, primary sclerosing cholangitis, cholangitis, choledocholithiasis, cholecystolithiasis, other structural disorders of the biliary tract, chronic hepatitis B or C virus, alcoholic liver disease, HIV, caroli disease, liver fluke; sudden onset of jaundice with pruritus, generalised malaise, weight loss, fatigue, pain often not present, alcohol consumption, cigarette smoking, obesity, hypertension, environmental toxins (e.g., 1,2-dichloropropane, asbestos)
Exam
jaundice, hepatomegaly
1st investigation
- serum liver tests:
elevated alkaline phosphatase; aspartate aminotransferase and alanine aminotransferase may be normal or elevated; direct bilirubin may be elevated
- prothrombin time/INR:
may be increased
More - CA19-9:
elevated
- abdominal ultrasound scan:
biliary dilation (intra- and extrahepatic)
More - abdominal CT or MRI:
intrahepatic mass lesion, dilated intrahepatic ducts, and localised lymphadenopathy may be seen
More
Other investigations
- magnetic resonance cholangiopancreatography (MRCP):
biliary dilation (intra- and extrahepatic) with extrahepatic mass causing obstruction/stricture
More - endoscopic ultrasound scan:
biliary dilation (intra- and extrahepatic) with extrahepatic mass causing obstruction/stricture
More - endoscopic retrograde cholangiopancreatography (ERCP):
biliary dilation (intra- and extrahepatic) with extrahepatic mass causing obstruction/stricture
More
Hodgkin's lymphoma
History
usually young adult, may have fever, night sweats, weight loss, generalised pruritus, alcohol-induced pain, abdominal pain
Exam
cervical or supraclavicular lymphadenopathy, hepatomegaly, splenomegaly, tonsillar enlargement, unlikely to have signs of liver disease alone
1st investigation
- serum liver tests:
elevation of alkaline phosphatase and bilirubin, with near-normal aspartate aminotransferase and alanine aminotransferase
- FBC:
may have thrombocytopenia, pancytopenia if bone marrow is involved
- prothrombin time/INR:
normal or elevated
- CT scan:
may demonstrate either solitary or multiple mass lesions in the liver; diffuse lesions without nodule formation are a relatively rare finding
More
Other investigations
- liver biopsy:
non-specific findings, or features of Hodgkin's lymphoma
- lymph node biopsy ± bone marrow biopsy:
abnormal
Non-Hodgkin's lymphoma
History
may be associated risk factors (e.g., age >50 years, history of Epstein-Barr virus infection, human T-lymphocytic virus 1, human herpes virus 8, hepatitis C virus, HIV infection, Helicobacter pylori infection, Sjogren's syndrome, coeliac disease), may be asymptomatic; weight loss, night sweats, fatigue, fevers, abdominal discomfort
Exam
may be normal; lymphadenopathy, pallor, jaundice, purpura, hepatomegaly, splenomegaly, skin nodules, change in mental status, unlikely to have signs of liver disease alone
1st investigation
- serum liver tests:
elevation of alkaline phosphatase and bilirubin, with near-normal aspartate aminotransferase and alanine aminotransferase
- prothrombin time/INR:
normal or elevated
- FBC:
may have thrombocytopenia, pancytopenia if bone marrow is involved
- CT scan:
may demonstrate either solitary or multiple mass lesions in the liver; diffuse lesions without nodule formation are a relatively rare finding
More
Other investigations
- liver biopsy:
non-specific findings, or features of non-Hodgkin's lymphoma
- lymph node biopsy ± bone marrow biopsy:
abnormal
Shock
History
may have underlying disorder (e.g., cardiac disease, evidence of gastrointestinal bleed, history of trauma, pancreatitis, diarrhoea and vomiting, burns, anaphylaxis/poisoning, pulmonary embolism), agitation, altered cognition; risk of acute liver failure with onset of encephalopathy, may progress to confusion and coma
Exam
hypotension, tachycardia, tachypnoea, cyanosis, oliguria, cool extremities; risk of acute liver failure with signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver test:
predominant aspartate aminotransferase and alanine aminotransferase elevation typically coinciding with episode of shock followed by decline; alkaline phosphatase and bilirubin may be elevated
- FBC:
haemorrhage: haemoglobin may be low; sepsis: WBC count >12 x 10⁹/L (>12,000/microlitre) or <4 x 10⁹/L (<4000/microlitre)
- prothrombin time/INR:
elevated
- Doppler liver ultrasound scan:
normal or decreased hepatic or portal flow, non-specific changes
Other investigations
- echocardiogram:
demonstrates decreased cardiac function, ejection fraction may be low
- serum urea and creatinine:
may be elevated
Portal vein thrombosis
History
may be a history of myeloproliferative disorders (polycythaemia vera, especially in young women), paroxysmal nocturnal haemoglobinuria, antiphospholipid antibody syndrome, prior or current oral contraceptives use, prior history of cirrhosis; generalised abdominal pain
Exam
splenomegaly, epigastric tenderness, mild hepatomegaly; if there is underlying liver disease may have jaundice, muscle wasting, gynaecomastia, palmar erythema, spider angiomata, petechiae, scratch marks, ascites, distended abdominal veins
1st investigation
- serum liver tests:
elevated aspartate aminotransferase, alanine aminotransferase alkaline phosphatase, and bilirubin
- prothrombin time/INR:
may be increased
- FBC with reticulocyte count:
leukopenia and/or thrombocytopenia
- abdominal ultrasound scan:
thrombus may be visualised as an echogenic area, or may not be demonstrated
Other investigations
- Doppler venous study of portal vein:
portal vein occlusion demonstrated
- abdominal MRI scan:
portal vein occlusion demonstrated
Budd-Chiari syndrome
History
may have personal history or family history of thrombophilia, myeloproliferative disorder; abdominal pain
Exam
ascites, hepatomegaly, splenomegaly, gastrointestinal bleed, leg oedema; uncommonly acute liver failure with jaundice, bleeding tendency, and signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver test:
elevated aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, and bilirubin
- prothrombin time/INR:
may be increased
- FBC:
may be abnormal in presence of underlying myeloproliferative disorder
- serum urea and creatinine:
may be elevated in acute liver failure
- colour and pulsed Doppler ultrasound:
large hepatic vein appearing void of flow signal, or with a reversed or turbulent flow; large intrahepatic or subcapsular collaterals with continuous flow connecting the hepatic veins or the diaphragmatic or intercostal veins; caudate lobe hypertrophy (>70%)
- MRI abdomen with contrast:
obstructed hepatic veins and inferior vena cava intrahepatic or subcapsular collaterals
More - screen for hypercoagulable state:
factor V Leiden, protein C or protein S deficiency, antithrombin III deficiency, antiphospholipid antibodies, or JAK2 mutation may be positive
Other investigations
- contrasted CT scan:
failure to visualise hepatic veins is considered suggestive for hepatic vein obstruction
More - hepatic venography:
thrombi are observed in hepatic veins, with spider web-like collaterals
- liver biopsy:
high-grade venous congestion, centrilobular liver cell atrophy, and, possibly, thrombi within terminal hepatic venules
Intrahepatic cholestasis of pregnancy
History
second- and third-trimester pregnancy, twin pregnancy, nausea, vomiting, abdominal pain, pruritus (sparing the face), fatigue
Exam
pregnancy, excoriations, jaundice, tender hepatomegaly, splenomegaly, lymphadenopathy
1st investigation
- serum liver tests:
elevated alkaline phosphatase 5-10 times normal; aspartate aminotransferase, alanine aminotransferase, and bilirubin also elevated; aminotransferase levels may be increased
- bile acids:
laboratory-specific upper end of the normal range, typically ≥10 micromol/L and <40 micromol/L (mild), ≥40 micromol/L and <100 micromol/L (moderate), and ≥100 micromol/L (severe); in non-fasting samples, 19 micromol/L is used as the lower diagnostic threshold
More
Haemolysis, elevated liver enzymes, low platelets (HELLP) syndrome
History
late-trimester pregnancy and in postnatal patients, history of pre-eclampsia, nausea, vomiting, abdominal pain, pruritus, fatigue, headache, visual disturbances; risk of acute liver failure with onset of encephalopathy, may progress to confusion and coma
Exam
pregnancy, may be hypertensive, oedematous, tender hepatomegaly, splenomegaly, lymphadenopathy, brisk reflexes, bleeding tendencies; risk of acute liver failure with signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver tests:
elevated aspartate aminotransferase, alanine aminotransferase, and elevated total and indirect bilirubin
- serum LDH:
elevated
- peripheral blood smear:
schistocytes, burr cells, polychromasia may be seen secondary to haemolysis
- serum uric acid:
elevated
- prothrombin time/INR:
increased
- FBC:
low platelet count
- serum electrolytes and creatinine:
may be evidence of renal impairment with elevated creatinine
- urinalysis and protein-to-creatinine ratio:
proteinuria
- fetal ultrasound:
may reveal growth restriction
- abdominal ultrasound:
non-specific changes
More
Other investigations
- serum haptoglobin:
low
More
Acute fatty liver of pregnancy
History
late pregnancy (28-40 weeks' gestation), history of pre-eclampsia, nausea, vomiting, abdominal pain, pruritus, fatigue, ascites, altered mental state; risk of acute liver failure with onset of encephalopathy, may progress to confusion and coma
Exam
pregnancy, hypertension (pre-eclampsia and eclampsia), jaundice, tender hepatomegaly, splenomegaly, lymphadenopathy; risk of acute liver failure with signs of encephalopathy (e.g., memory, attention, and concentration deficits; confusion, asterixis, nystagmus, clonus, rigidity, coma)
1st investigation
- serum liver tests:
moderate elevation of aspartate aminotransferase and alanine aminotransferase, direct bilirubin also elevated
- prothrombin time/INR:
normal or increased in severe disease
- serum glucose:
may be reduced
- serum urea and creatinine:
may be elevated
- FBC:
may show leukocytosis
- abdominal ultrasound:
normal or diffuse pattern; ascites
More
Use of this content is subject to our disclaimer
 ]
]