Approach
Small interatrial communications can close spontaneously. If corrective closure is required, device closure in the catheterisation laboratory or surgical closure can be used depending on the type of interatrial communication.[25] Minimally invasive surgical repair can be performed through limited sternal and parasternal incisions, antero-lateral thoracotomies, or lateral mini-thoracotomies.[26]
Interatrial communications should be treated by physicians experienced in the management of congenital heart disease.[23][27]
Indications for corrective closure
Young patients with interatrial communications can be observed initially, as small defects may close or shrink and may not need corrective closure. If the ratio of pulmonary vascular to systemic blood flow, Qp:Qs, is <1.5, the defect is of little prognostic importance and does not require closure. If the Qp:Qs ratio is or remains ≥1.5, or there is evidence of right atrial enlargement, the defect requires closure to prevent heart failure, atrial arrhythmias, and pulmonary vascular obstructive disease.[28] This is usually performed at age 2 to 4 years. Patients who develop unremitting heart failure require earlier repair.
A key consideration in patients with interatrial communications is the extent of pulmonary vascular resistance (PVR). Corrective closure is not recommended if PVR is ≥5 Wood units (WU). Instead, pulmonary vasodilator therapy should be initiated in an attempt to lower PVR.[23][27] If pulmonary vasodilator treatment lowers PVR to <5 WU, corrective closure may be considered. If the patient is not responding and PVR remains ≥5 WU, corrective closure should generally not be performed.[23] Note that in some patients with a left-to-right shunt and a PVR ≥5WU, corrective closure or partial closure may still be considered by some clinicians on a case-by-case basis, weighing risks and benefits.
Fixed pulmonary hypertension with shunt reversal as a result of pulmonary overcirculation is also referred to as Eisenmenger's syndrome and is associated with various degrees of desaturation. Patients with Eisenmenger's syndrome should avoid pregnancy, dehydration, and high altitudes. They are at increased risk of systemic thromboembolism. Endocardial pacing is therefore contra-indicated and particular care must be taken with intravenous injections to avoid air embolism.
Patients with Eisenmenger's syndrome frequently develop erythrocytosis to compensate for the hypoxaemia, which can lead to hyperviscosity. Hyperviscosity can produce symptoms of headache, fatigue, and sometimes mental status changes. Treatment of symptomatic hyperviscosity involves phlebotomy and intravenous infusion of saline. Routine phlebotomy should be avoided.
Pulmonary vasodilator therapy may be used to improve quality of life. Those demonstrated to be of benefit include endothelin receptor antagonists (e.g., bosentan), the phosphodiesterase-5 inhibitors sildenafil or tadalafil, and, in limited studies, infusions of the prostanoid epoprostenol.[29] Oral therapy is usually favoured to avoid complications associated with intravenous administration in patients with Eisenmenger's syndrome. A pulmonary-to-systemic shunt (reversed Potts shunt) procedure may be considered as a last resort option for patients with pulmonary hypertension who have undergone surgical correction of congenital heart disease and are unresponsive to maximal medical therapy. It may improve exercise capacity and facilitate easier medical management. Heart and lung transplantation, or double lung transplantation with repair of the cardiac defect, may also be considered in selected patients with severe disease.[10]
Options for corrective closure
Treatment involves percutaneous closure or an operation (using either direct sutures or a patch of autologous pericardium) to close the defect. Device closure is used to treat secundum defects but cannot usually be used in other types of interatrial communications due to the closeness of the defects to other cardiac structures. Surgical closure is indicated for large defects, defects with missing rims that prevent secure placement of a catheter device, or if associated lesions need corrective surgery simultaneously.
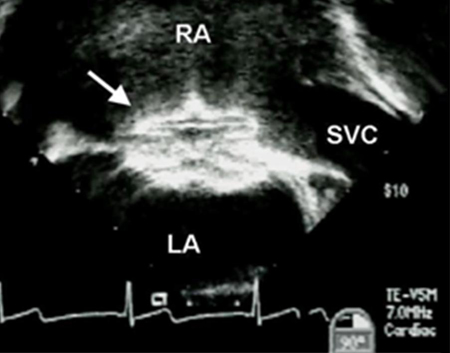
Ostium secundum atrial septal defect (ASD) or vestibular ASD: device closure is the preferred method if rims are adequate to secure a device. [Figure caption and citation for the preceding image starts]: Trans-oesophageal echocardiographic image of an interatrial communication occluder device (arrow). LA: left atrium; RA: right atrium; SVC: superior vena cavaImage courtesy of Patrick W. O'Leary, MD [Citation ends].
 If the rims are inadequate or there are large septal aneurysms or multiple fenestrations of the atrial septum, surgical closure is required.
If the rims are inadequate or there are large septal aneurysms or multiple fenestrations of the atrial septum, surgical closure is required.Ostium primum defect: surgical closure with repair of the left atrioventricular valve is the most commonly used procedure.
Coronary sinus defect: surgical correction can be performed by simply closing the orifice of the coronary sinus. However, in the presence of a left superior vena cava, re-routing to the right atrium is needed to avoid significant systemic arterial desaturation.
Sinus venosus defect: anomalous right pulmonary veins are baffled via the defect to the left atrium. A Warden operation may also be performed, whereby the superior vena cava is transected and then reconnected to the right atrial appendage while a patch is placed to the orifice of the superior vena cava to route anomalous right pulmonary vein flow across the defect to the left atrium.
Sinus venosus defect with partial anomalous pulmonary drainage and unroofed coronary sinus (especially if associated with a persistent left superior vena cava) should be corrected irrespective of shunt volume.
Surgical correction can be performed with minimally invasive strategies through thoracotomies or mini-sternotomies, with equivalent results when compared with conventional median sternotomy procedures.[26]
Prophylactic antibiotics to prevent endocarditis are required for the first 6 months after device or surgical closure.[23][27] Patients with unrepaired cyanotic heart disease will also require endocarditis prophylaxis when undergoing certain interventions.
Use of this content is subject to our disclaimer