Investigations
1st investigations to order
visual field testing (perimetry)
Test
Diagnosis must include serial perimetry.[1] The visual field defects are the same types that occur in papilloedema due to other causes and are similar to those found in glaucoma. The most common defects are enlargement of the physiological blind spot and loss of inferonasal portions of the visual field, along with constriction of isopters.[35] Central defects are uncommon and warrant a search for another diagnosis unless there is a large serous retinal detachment from high-grade optic disc oedema (which can be seen with optical coherence tomography). The loss of visual field may be progressive and severe, and lead to blindness. The temporal profile of visual loss is usually gradual. However, acute severe loss of vision of the type found in ischaemic optic neuropathy can occur.
Result
visual field defects; enlarged blind spot, inferonasal loss, other nerve fibre bundle defects, or constriction of the field
dilated fundoscopy
Test
Frisén grading stages papilloedema from stage 0 (normal optical disc) to stage 5 (severe).[37][44] Grades 3 and greater are risk factors for poor visual outcome.[42][Figure caption and citation for the preceding image starts]: Frisén stage 1From the personal collection of Dr M. Wall; used with permission [Citation ends].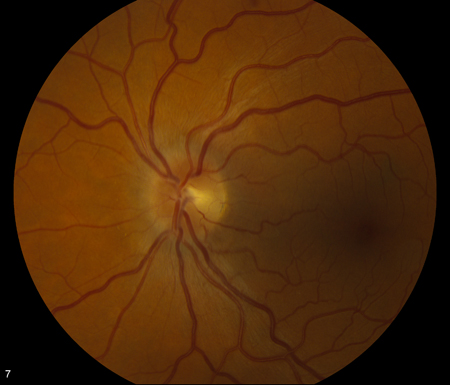 [Figure caption and citation for the preceding image starts]: Frisén stage 2From the personal collection of Dr M. Wall; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Frisén stage 2From the personal collection of Dr M. Wall; used with permission [Citation ends].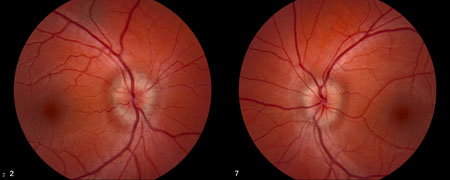 [Figure caption and citation for the preceding image starts]: Frisén stage 3From the personal collection of Dr M. Wall; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Frisén stage 3From the personal collection of Dr M. Wall; used with permission [Citation ends].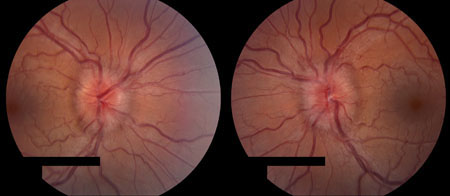 [Figure caption and citation for the preceding image starts]: Frisén stage 4From the personal collection of Dr M. Wall; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Frisén stage 4From the personal collection of Dr M. Wall; used with permission [Citation ends].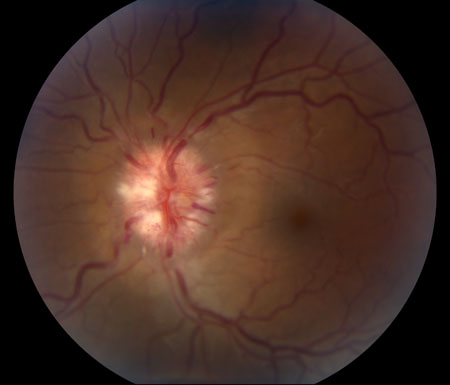 [Figure caption and citation for the preceding image starts]: Frisén stage 5From the personal collection of Dr M. Wall; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Frisén stage 5From the personal collection of Dr M. Wall; used with permission [Citation ends].
Result
Frisén grading of papilloedema
visual acuity
Test
Mild visual loss is common in patients with idiopathic intracranial hypertension.[54] However, only around one fifth of patients have any abnormality in Snellen visual acuity, and Snellen testing is insensitive to the amount of visual loss found with perimetry and to worsening of the grade of papilloedema.[38]
Result
usually normal, or near normal, in patients with papilloedema, except when the condition is long-standing and severe, or if there is a neurosensory detachment
MRI of brain with or without contrast
Test
Axial and sagittal views are used to assess for empty sella and flattening of the globe.[Figure caption and citation for the preceding image starts]: Magnetic resonance image (MRI) of empty sella on sagittal viewFrom the personal collection of Dr M. Wall; used with permission [Citation ends].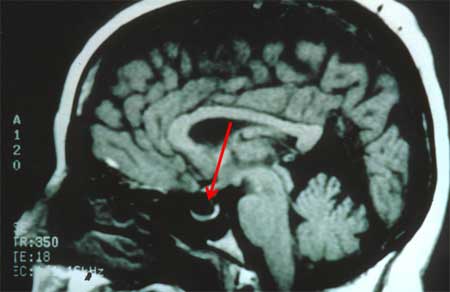
Result
transverse sinus stenosis has a high specificity (95%) and reasonable sensitivity (84%); other signs have overall high specificity but low sensitivity, and include empty sella, posterior pituitary stalk displacement, meningoceles, posterior globe flattening, abnormalities of the optic nerve, slit-like ventricles, tight subarachnoid spaces, and inferior position of cerebellar tonsils
lumbar puncture at spinal L3/L4
Test
Can be done once intracranial mass lesions have been excluded. Aseptic technique and local anaesthetic are required. Patient should be in the left lateral decubitus position with legs extended before measuring opening pressure, with normal respiratory rate and depth (no observable hypo- or hyperventilation). It is often easier to enter the subarachnoid space with the patient in the sitting position and then place the patient in the lateral decubitus position for pressure measurement and cerebrospinal fluid collection. Fluoroscopic-guided lumber puncture may be preferred for patients who are very obese. Sedation causes hypoventilation and should not be used when recording intracranial pressure.
Result
elevated: opening pressure >250 mm H2O; opening pressures between 200 and 250 mm H2O are intermediate and require other signs of raised intracranial pressure, such as bilateral venous stenoses on magnetic resonance venography
Investigations to consider
magnetic resonance venogram of head
Test
Bilateral venous stenoses of the transverse sinus are commonly found with increased intracranial pressure.
Result
negative for venous thrombosis; usually shows bilateral venous stenosis of transverse sinus
optical coherence tomography
Test
Measures the thickness of the retinal nerve fibre layer and quantifies the progress of papilloedema.[44]
Result
evaluation of retinal nerve fibre layer thickness
Use of this content is subject to our disclaimer