Investigations
1st investigations to order
chest x-ray
Test
A plain chest x-ray (CXR) should be obtained in every patient suspected to have CAO.[2][69][70]
Infrequently diagnostic, with a sensitivity to detect abnormalities of the trachea and main bronchi of approximately 66%.[71]
Air trapping, the hallmark of airway obstruction on CXR, is characterised by failure of the lung to decrease in volume and increase in opacity on exhalation compared with inhalation, as well as mediastinal shift to the side that is not trapping air.[71]
Τracheobronchial filling defects are indicative of mucus or neoplasms. Lobar or total lung collapse result from tumour-related obstruction of a main bronchus.
The 'Golden S sign' has been associated with the presence of a central obstructive mass. When a lobe collapses around a large central mass, the peripheral lung collapses and the central portion of the lung is prevented from collapsing by the presence of the mass. The related lung fissure is concave towards the lung peripherally but convex centrally, and the shape of the fissure resembles an 'S' or a 'reverse S'.[71]
Result
tracheal deviation, mediastinal shift, air trapping on exhalation phase film, tracheobronchial filling defect, post-obstructive pneumonia, atelectasis, lobar or total lung collapse, 'Golden S sign'
Investigations to consider
bronchoscopy (flexible and/or rigid)
Test
The most specific and sensitive test in the diagnosis of CAO.
Direct visualisation via bronchoscopy provides information on the location and morphology of the lesion, the amount of intraluminal disease, the presence of extraluminal compression, and the diameter and length of the lesion. Also allows evaluation of the surrounding tissue, in particular the airway distal to the obstruction. Tissue can be obtained for pathological diagnosis if necessary.[2]
Diagnostic flexible bronchoscopy is not able to provide complete evaluation of extraluminal disease or of the airways distal to the obstruction. Potentially dangerous in severe obstruction as the bronchoscope further obstructs the already narrow lumen, thus limiting ventilation and secretions. Swelling or bleeding may occur at the stricture site post-procedure.[18] The moderate sedation required may decrease ventilation and relax the respiratory muscles, creating a potentially unstable airway.
Rigid bronchoscopy is a safe and effective way of securing the airway that provides the ability to ventilate and oxygenate the patient while undertaking diagnostic and therapeutic airway intervention, and is thus the procedure of choice in patients with impending respiratory failure.[16][69][72][73][74][75]
Result
detailed characteristics of specific lesion
CT chest
Test
High-resolution computed tomography (HRCT) is the imaging test of choice in diagnosing CAO.[69] Computed tomography (CT) is a superior imaging modality to chest x-ray in detecting tracheal and main bronchi abnormalities, with a reported sensitivity of 97%.[71]
Allows determination of the type of obstructive lesion (intraluminal, extrinsic, or mixed) and the patency of the airway distal to the obstruction, the length and diameter of the lesion, and its relationship to nearby structures including vessels.[2]
Multidetector CT allows enhanced detection of airway lesions such as endobronchial tumours (including those in the central airways) that may be missed by conventional CT. [Figure caption and citation for the preceding image starts]: Malignant endobronchial obstruction on multidetector chest CT: lung window demonstrating right mainstem malignant obstructionFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends].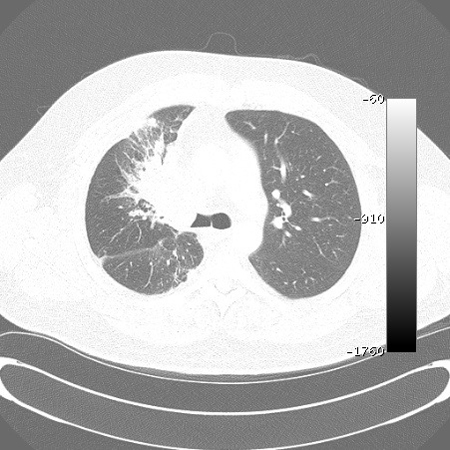 [Figure caption and citation for the preceding image starts]: Malignant endobronchial obstruction on multidetector chest CT: mediastinal window demonstrating right mainstem malignant obstructionFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Malignant endobronchial obstruction on multidetector chest CT: mediastinal window demonstrating right mainstem malignant obstructionFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends]. Also enables the reconstruction techniques of multiplanar reconstructions, external representation with 3D shaded surface displays, and volumetric representation with internal rendering (i.e., virtual bronchoscopy), which provide more accurate estimations of the length of tracheal and bronchial lesions.[41][77][Figure caption and citation for the preceding image starts]: Malignant endobronchial obstruction on multidetector chest CT: coronal reconstruction demonstrating right mainstem malignant obstructionFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends].
Also enables the reconstruction techniques of multiplanar reconstructions, external representation with 3D shaded surface displays, and volumetric representation with internal rendering (i.e., virtual bronchoscopy), which provide more accurate estimations of the length of tracheal and bronchial lesions.[41][77][Figure caption and citation for the preceding image starts]: Malignant endobronchial obstruction on multidetector chest CT: coronal reconstruction demonstrating right mainstem malignant obstructionFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends].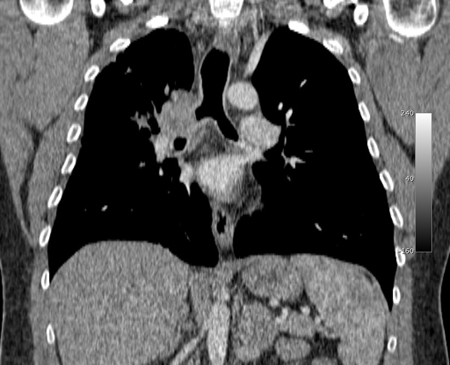 [Figure caption and citation for the preceding image starts]: Malignant endobronchial obstruction on multidetector chest CT: 3D volume rendering reconstruction demonstrating right mainstem malignant obstructionFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Malignant endobronchial obstruction on multidetector chest CT: 3D volume rendering reconstruction demonstrating right mainstem malignant obstructionFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends].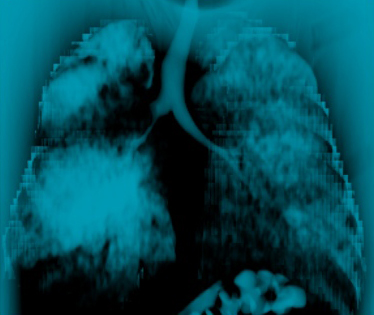 [Figure caption and citation for the preceding image starts]: Malignant endobronchial obstruction on multidetector chest CT: 2D multiplanar reconstruction (minimal intensity projection) demonstrating right mainstem malignant obstructionFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Malignant endobronchial obstruction on multidetector chest CT: 2D multiplanar reconstruction (minimal intensity projection) demonstrating right mainstem malignant obstructionFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends].
Virtual bronchoscopy is comparable to flexible bronchoscopy for the visualisation of the central airways and detection of obstructive bronchial lesions (both endoluminal and external) and focal airway stenoses.[41][78][79]
Paired inspiratory dynamic and expiratory multislice helical CT of the chest is useful in the diagnosis of tracheobronchomalacia.[13] Malacia of the central airways is defined as a reduction in the cross-sectional area of >50% on expiratory images compared with inspiratory images.[77][1][Figure caption and citation for the preceding image starts]: Dynamic airway collapse: A. bronchoscopic view on inhalation; B. bronchoscopic view on exhalation showing dynamic airway collapse; C. CT chest showing normal airway on inhalation; D. CT chest showing significant airway collapse on exhalationFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends].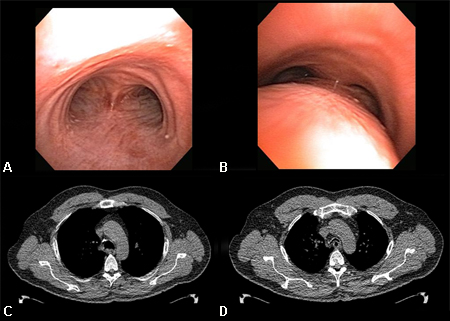
Result
diffuse or focal tracheal narrowing, intratracheal masses, tracheal deviation, tracheal compression, space-occupying bronchial lesions (e.g., tumour, mucus), tracheobronchial filling defect, post-obstructive pneumonia, lobar atelectasis, partial or total lung collapse, extraluminal compression, diffuse or focal bronchial narrowing, 'Golden S sign', >50% reduction in cross-sectional area on expiration in malacia of central airways
MRI of chest
Test
Useful in assessing the larynx, proximal trachea, and mediastinal and hilar masses, and to readily differentiate between vascular and soft-tissue masses.[69]
Able to provide multiplane images of the chest without the need of contrast material and particularly good at visualising vascular structures surrounding the airways, such as vascular rings or aneurysms that may compress the trachea.[35]
Result
vascular rings, aneurysms, soft tissue masses
flow-volume loops (FVL)
Test
Assessment of the shape of the FVL allows identification and categorisation of upper airway obstruction (UAO) as dynamic (non-fixed or variable) extrathoracic, dynamic (non-fixed or variable) intrathoracic, or fixed UAO. [Figure caption and citation for the preceding image starts]: Dynamic (non-fixed or variable) extrathoracic upper airway obstruction: flow-volume loop shows 'flattened' inspiratory limb during forced inspirationFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends].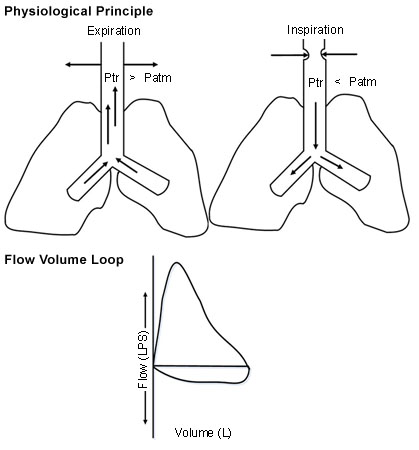 [Figure caption and citation for the preceding image starts]: Dynamic (non-fixed or variable) intrathoracic upper airway obstruction: flow-volume loop shows 'flattened' expiratory limb during forced exhalationFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Dynamic (non-fixed or variable) intrathoracic upper airway obstruction: flow-volume loop shows 'flattened' expiratory limb during forced exhalationFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends].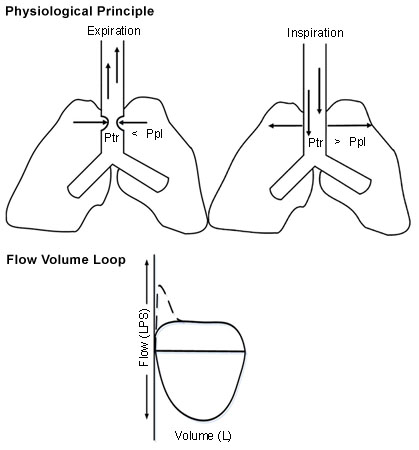 [Figure caption and citation for the preceding image starts]: Fixed upper airway obstruction: flow-volume loop shows 'flattened' inspiratory and expiratory loopsFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Fixed upper airway obstruction: flow-volume loop shows 'flattened' inspiratory and expiratory loopsFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends].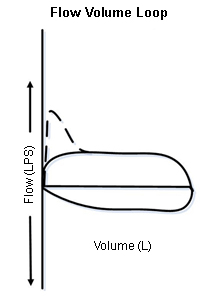
Takes into account the dynamic characteristics of the airways, such as alterations in upper airway calibre due to changes in the transmural pressure induced by forced inspiratory and expiratory manoeuvres during spirometry.
As the classical tracings of tracheal obstruction are not seen until the lumen is severely narrowed (diameter 8-10 mm), FVL is not very sensitive in detecting UAO.[2][15][35]
In patients with pre-existing lung diseases (e.g., COPD), the FVL may not show the described configuration due to the inability to generate high enough flow rates and the presence of airflow obstruction in multiple anatomical sites.[2] Thus, central lesions are under-recognised with FVL in these patients.[15]
Result
flattened inspiratory limb in variable extrathoracic UAO, flattened expiratory limb in variable intrathoracic UAO, flattened inspiratory and expiratory limbs in fixed UAO
spirometry
Test
Due to the possibility of inducing respiratory failure, spirometry should not be undertaken in patients with respiratory distress or advanced CAO.[2]
Significant reductions in the forced expiratory volume in 1 second (FEV1) are not observed until the diameter at the obstruction site decreases to 6 mm. Thus, FVL changes may be seen prior to the development of an abnormal FEV1.[2]
Result
disproportionate peak expiratory flow rate reduction in comparison to FEV1, maximal voluntary ventilation (MVV) to FEV1 ratio <25%, MVV reduction with normal FEV1
Emerging tests
endobronchial ultrasound (EBUS)
Test
EBUS has been used successfully in the assessment and treatment planning of CAO.[2][82] Although not used routinely in clinical practice, it can be used to determine the presence of extracartilaginous disease, the degree of airway involvement, and identify the distal end of an obstructive lesion once the obstruction has been acutely stabilised.[1]
Result
extracartilaginous disease
Use of this content is subject to our disclaimer