Complications
Laser therapy: Complications include perforation (of airways, oesophagus, or pulmonary artery), cardiac arrhythmias, pneumothorax (tension and non-tension), haemorrhage, hypoxaemia, myocardial infarction, stroke, air embolism (secondary to gas exiting the probe tip under pressure and crossing the mucosal membranes into the blood vessels through bronchovascular fistulae formed by coagulation of the tissue), and endobronchial ignition (it is thus recommended that the FiO2 should not exceed 40% during the procedure).[63]
Electrocautery: Risk of haemorrhage is between 2% and 5%. Other complications include endobronchial ignition, electric shock to the operator if appropriate grounding not in place, and airway perforation. Loss of effectiveness can occur with bleeding due to the diffusion of the current across a larger surface area.
Argon plasma coagulation: Overall complication rate of <1%. Complications include haemorrhage, airway perforation and stenosis, endobronchial ignition, and air embolism with argon gas.
Photodynamic therapy (PDT): The most common complication is skin photosensitivity that lasts for 4 to 6 weeks; patients must be advised to avoid sun exposure during this time. Other complications include local airway oedema, strictures, haemorrhage, and fistulae formation, although PDT has a lower risk of airway perforation.
Balloon bronchoplasty: Complications include stenosis recurrence, pain, mediastinitis, and bleeding, as well as airway tearing or rupture with subsequent pneumothorax or pneumomediastinum.
Airway stenting: Associated with a high complication rate, particularly with long-term use.[19] Silicone stents (e.g., Dumon stent, Montgomery T-tube, Hood stent, Reynders-Noppen Tygon stent) are complicated by a high migration rate and obstruction by granulation tissue formation at the stent-ends or by mucous secretions due to impaired mucociliary clearance.[2][69][74][114]Stents may also be associated with halitosis, stent fracture, metal fatigue, airway and vascular perforations, mucosal tears, and obstruction of lobar orifices.[18][69][74][122]
The American College of Chest Physicians multi-centre registry study reported an overall complication rate of 3.9% (range 0.9% to 11.7%) following therapeutic bronchoscopic procedures for malignant CAO. The risk factors identified for complications included emergency/urgent procedures, an American Society of Anesthesiologists (ASA) score >3, redo therapeutic bronchoscopy, and moderate sedation. They also report a 14.8% 30-day mortality.[139][Figure caption and citation for the preceding image starts]: Chest x-ray showing right mainstem endobronchial stent occlusion with mucusFrom the collections of Jose Fernando Santacruz MD, FCCP, DAABIP and Erik Folch MD, MSc; used with permission [Citation ends].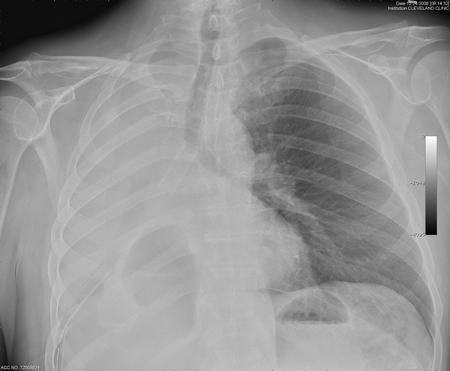
The major limiting factor of external beam radiation (EBR) is the unwanted radiation exposure of normal tissue, including the lung parenchyma, heart, spine, and oesophagus. Approximately 50% of patients treated with EBR for local control develop disease progression in the irradiated field.
Approximately 20% to 30% of patients with lung cancer will develop clinical features and complications associated with airway obstruction, including post-obstructive pneumonia.[2]
Presents with dyspnoea, cough, purulent sputum, fevers, and chills.[66] Recurrent pneumonias are also frequent.
Post-obstructive pneumonia may be evident on chest x-ray or computed tomography.
Non-resolving or post-obstructive pneumonia related to central airway obstruction (CAO) will not adequately respond clinically and radiographically to antibiotic therapy, and patients may experience persistent symptoms and chest x-ray may show signs of infiltrates for >4 to 6 weeks.
In patients with post-obstructive infections, a course of antibiotics should be given after the airway has been re-established. However, the usefulness of empirical antibiotic coverage following CAO relief is unproven.
Complications of this technique include haemorrhage (particularly in the right and left upper lobes and often presenting with massive haemoptysis), fistula formation to the mediastinum, arrhythmias, hypotension, bronchospasm, bronchial stenosis or necrosis, and radiation bronchitis. Fatal haemorrhage has been described in up to 32% of cases; however, it is difficult to distinguish between bleeding caused by radiation and that caused by the tumour itself.
Use of this content is subject to our disclaimer