History and exam
Key diagnostic factors
common
presence of risk factors
hearing loss
Commonly presents with a conductive hearing loss.[1] There may be a mixed conductive and sensorineural hearing loss in patients with cochlear damage or in those with a pre-existing hearing loss (e.g., congenital or presbycusis). Hearing may be normal in some patients.
ear discharge resistant to antibiotic therapy
Recurrent or chronic purulent aural discharge that may be unresponsive to antibiotic therapy is common in acquired cholesteatoma.
Discharge is malodorous and may be scant.
attic crust in retraction pocket
Otoscopy typically shows crust or keratin in the attic (upper part of the middle ear), the pars flaccida, or the pars tensa (usually posterior superior aspect), with or without a perforation of the tympanic membrane.[Figure caption and citation for the preceding image starts]: Retraction pocket in attic (upper part of the middle ear)From Dr Susan Douglas' personal teaching collection [Citation ends]. [Figure caption and citation for the preceding image starts]: Cholesteatoma in attic (upper part of the middle ear)From Dr Susan Douglas' personal teaching collection [Citation ends].
[Figure caption and citation for the preceding image starts]: Cholesteatoma in attic (upper part of the middle ear)From Dr Susan Douglas' personal teaching collection [Citation ends].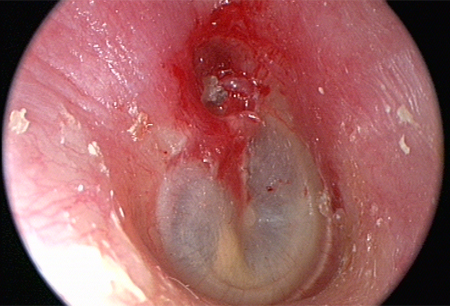
uncommon
white mass behind intact tympanic membrane
Occurs in congenital cholesteatoma.
Other diagnostic factors
common
tinnitus
May be associated with hearing loss; occurs in the affected ear.
uncommon
otalgia
Uncommonly found. Pain may be a feature of advanced disease.
altered taste
Occurs due to involvement of the facial nerve (cranial nerve VII).
dizziness
Occurs if there is erosion of the semicircular canal with the disease.
Risk factors
strong
middle ear disease
Acquired cholesteatoma is usually associated with eustachian tube dysfunction, often with a previous history of middle ear disease such as otitis media.[4]
eustachian tube dysfunction
Typically due to otitis media. Eustachian tube dysfunction promotes invagination of the tympanic membrane, which becomes pulled into the middle ear space because of the negative pressure (vacuum-like) effect.[16] This forms a retraction pocket.
These pockets are initially self-cleansing. However, the neck of the pocket then narrows and traps squamous cells, expands in size, and leads to cholesteatoma formation.[3]
otological surgery
May lead to implantation of viable keratinocytes into the middle ear cleft, which can result in cholesteatoma formation.[4]
traumatic blast injury to ear
May lead to implantation of viable keratinocytes into the middle ear cleft, which can result in cholesteatoma formation.[4]
weak
family history
Children with a family history of middle ear disease and/or cholesteatoma have an increased risk of developing cholesteatoma.[16][21] One Swedish case-control study using nationwide register data found that the risk of cholesteatoma was strongly associated with a family history of the condition, suggesting a possible genetic pre-disposition; family history was nevertheless quite rare and could therefore only explain a limited number of all cases.[13]
Use of this content is subject to our disclaimer