Approach
Diagnosis is usually clinical. However, the findings often mimic those seen in other disease states; therefore, other conditions may need to be excluded.
Diagnostic phenotypes
A diagnosis of rosacea may be considered in the presence of 1 of the following diagnostic cutaneous signs:[1]
Fixed centrofacial erythema. People with Fitzpatrick skin types I to IV have a prominent history of flushing or blushing and usually present with persistent redness of the facial skin. In patients with type V or VI skin, erythema may be difficult to detect, and papules and pustules may be the first clearly visible signs of rosacea.
Phymatous changes. These can include patulous follicles, skin thickening or fibrosis, glandular hyperplasia, and a bulbous appearance. The most common form is rhinophyma, but other phymas may occur.
Major phenotypes
Without a diagnostic phenotype, the presence of 2 or more major features may be considered diagnostic.[1] Major phenotypes include the following:
Papules and pustules. The presence of dome-shaped red papules on the forehead, malar areas, nose, and chin, with or without accompanying pustules and often in crops, is characteristic of the disease. Nodules may also occur. Although patients with concomitant acne may exhibit comedones, comedones should be considered part of an acne process unrelated to rosacea, as has been supported by transcriptome analyses in acne and rosacea.
Flushing. A history of frequent blushing or flushing is common in people with Fitzpatrick skin types I to IV. In contrast to other erythematous changes, in rosacea flushing can occur within seconds to minutes in response to neurovascular stimulation by trigger factors.
Telangiectasia. Telangiectases are common signs of rosacea and are predominantly centrofacial in people with Fitzpatrick skin types I to IV. They are rarely seen in people with skin type V or VI; a dermatoscope may aid detection of telangiectases in these patients.
Ocular manifestations. Ocular rosacea can occur in the context of mild, moderate, or severe dermatological disease and may also appear in the absence of diagnostic skin manifestations. Ocular signs strongly suggestive of ocular rosacea include lid margin telangiectases, interpalpebral conjunctival injection, spade-shaped infiltrates in the cornea, and scleritis and sclerokeratitis. Ocular findings are the initial presentation in up to 20% of patients, some of whom may never progress to other phenotypes.[16]
A personal history, drug history, and complete physical examination are helpful to clinicians in excluding other entities in the possible differential diagnoses such as lupus erythematosus, corticosteroid-induced rosacea, or seborrhoeic eczema.
Secondary signs and symptoms
Secondary signs and symptoms may appear with 1 or more diagnostic or major phenotypes and may include the following:[1]
Burning or stinging. Burning or stinging sensations may occur typically on erythematous skin without scales, although scaling may also occur, especially on malar skin.
Oedema. Facial oedema may accompany or follow prolonged erythema or flushing. Sometimes soft oedema may last for days or be aggravated by inflammatory changes. Solid facial oedema (persisting hard, non-pitting oedema) can occur with rosacea, often, but not only, as a sequela of papules and pustules.
Dry appearance. Central facial skin may be rough and scaly so as to resemble dry skin and suggest an eczematous dermatitis, and rosacea may often include the co-existence of seborrhoeic dermatitis. This 'dry appearance' may be associated with burning or stinging sensations and may be caused by irritation rather than the disease process.[Figure caption and citation for the preceding image starts]: RhinophymaCourtesy of Dr Richard Allen Johnson (MD, CM. Harvard Medical School); used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Rosacea with erythema, papules, and pustulesCourtesy of Dr Richard Allen Johnson (MD, CM. Harvard Medical School); used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Rosacea with erythema, papules, and pustulesCourtesy of Dr Richard Allen Johnson (MD, CM. Harvard Medical School); used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Ocular rosacea and rhinophymaCourtesy of Dr Richard Allen Johnson (MD, CM. Harvard Medical School); used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Ocular rosacea and rhinophymaCourtesy of Dr Richard Allen Johnson (MD, CM. Harvard Medical School); used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Ocular rosacea presenting as chalazionCourtesy of Dr Richard Allen Johnson (MD, CM. Harvard Medical School); used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Ocular rosacea presenting as chalazionCourtesy of Dr Richard Allen Johnson (MD, CM. Harvard Medical School); used with permission [Citation ends].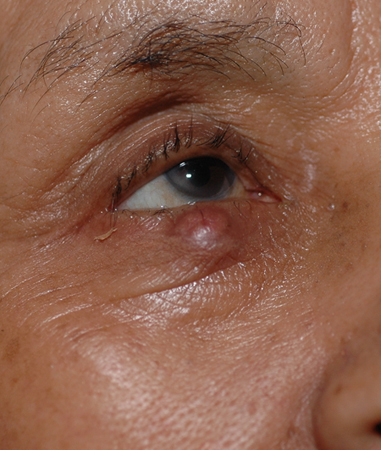 [Figure caption and citation for the preceding image starts]: Rosacea fulminansCourtesy of Dr Richard Allen Johnson (MD, CM. Harvard Medical School); used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Rosacea fulminansCourtesy of Dr Richard Allen Johnson (MD, CM. Harvard Medical School); used with permission [Citation ends]..jpg?status=ACTIVE)
Clinical stages
Rosacea is a progressive disorder that usually advances in stages if left untreated. There are 4 basic stages:
Stage 1: flushing (transient erythema, pre-rosacea)
A history of frequent blushing or flushing is common. Erythema may last for hours to days.[1]
Stage 2: persistent erythema
The most common sign is unremitting redness of the skin.[1]
Stage 3: papules and pustules
The presence of dome-shaped red papules on the forehead, malar areas, nose, and chin, with or without accompanying pustules and often in crops, is characteristic of the disease. The papules are usually not tender and they are not associated with scarring. Nodules may also occur.[1]
Although patients with rosacea may also exhibit features of acne, including comedones, these should be considered unrelated to rosacea.[1]
Stage 4: telangiectases
The presence of telangiectases is common but not necessary for the diagnosis.[1]
Investigations
Consider investigations to exclude other conditions. These may include an antinuclear antibody titre if systemic lupus erythematosus or other connective tissue disease is suspected, or a skin biopsy to exclude conditions such as sarcoidosis and mastocytosis.
Rosacea is characterised by several histopathological features on skin biopsy that are non-specific:
Telangiectases: often prominent with a peri-vascular and peri-follicular infiltrate of lymphocytes
Demodex mites: may be present in the hair follicle; sometimes increased in number in people with rosacea compared to people without rosacea (although there is no proven causal link)
Plasma cells: a small number of cells are usually present.
Use of this content is subject to our disclaimer