Dupuytren contracture
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
no MCP joint or PIP joint contracture
expectant management
Patients with early Dupuytren contracture who have evidence of the disease but have not yet developed contractures may be managed expectantly with regular follow-up every 6 months to evaluate for disease progression. Use of the Hueston table-top test and appropriate staging of Dupuytren contracture are essential during follow-up sessions.[49]Townley WA, Baker R, Sheppard N, et al. Dupuytren's contracture unfolded. BMJ. 2006;332:397-400. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1370973 http://www.ncbi.nlm.nih.gov/pubmed/16484265?tool=bestpractice.com [50]Au-Yong IT, Wildin CJ, Dias JJ, et al. A review of common practice in Dupuytren surgery. Tech Hand Up Extrem Surg. 2005 Dec;9(4):178-87. http://www.ncbi.nlm.nih.gov/pubmed/16340578?tool=bestpractice.com
corticosteroid injections
Treatment recommended for SOME patients in selected patient group
Patients with early Dupuytren contracture who have evidence of the disease but have not yet developed contractures can be treated with corticosteroid injections if they are experiencing bothersome symptoms.
The injection of Dupuytren nodules with triamcinolone acetonide monthly for up to 5 months or every 6 weeks for 3 injections has been shown to produce significant regression of the disease, with an average of 3.2 injections per nodule required for improvement of function.[28]Ketchum LD, Donahue TK. The injection of nodules of Dupuytren's disease with triamcinolone acetonide. J Hand Surg Am. 2000 Nov;25(6):1157-62. http://www.ncbi.nlm.nih.gov/pubmed/11119679?tool=bestpractice.com After corticosteroid injection, fewer patients progress to surgery than would be predicted with expectant management alone.[28]Ketchum LD, Donahue TK. The injection of nodules of Dupuytren's disease with triamcinolone acetonide. J Hand Surg Am. 2000 Nov;25(6):1157-62. http://www.ncbi.nlm.nih.gov/pubmed/11119679?tool=bestpractice.com
Primary options
triamcinolone acetonide: consult specialist for guidance on dose
≤30 degrees MCP joint contracture with no PIP joint contracture
collagenase injection
Collagenase clostridium histolyticum is used to treat adult patients with a palpable cord along with metacarpophalangeal (MCP) joint contracture or proximal interphalangeal (PIP) joint contracture, with a corresponding decrease in both fasciotomies and fasciectomies.[29]Lipman MD, Carstensen SE, Deal DN. Trends in the treatment of Dupuytren disease in the United States between 2007 and 2014. Hand (N Y). 2017 Jan;12(1):13-20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5207289 http://www.ncbi.nlm.nih.gov/pubmed/28082837?tool=bestpractice.com A mean of 1.4 injections is required to normalize affected joints, and clinical success is achieved within 29 days.[30]Badalamente MA, Hurst LC. Efficacy and safety of injectable mixed collagenase subtypes in the treatment of Dupuytren's contracture. J Hand Surg Am. 2007 Jul-Aug;32(6):767-74. http://www.ncbi.nlm.nih.gov/pubmed/17606053?tool=bestpractice.com In one study, reductions in contracture to 0 to 5 degrees of full extension, 30 days after the last injection, were achieved in cords injected with collagenase as compared with those injected with placebo.[31]Hurst LC, Badalamente MA, Hentz VR, et al. Injectable collagenase clostridium histolyticum for Dupuytren's contracture. N Engl J Med. 2009 Sep 3;361(10):968-79. https://www.nejm.org/doi/full/10.1056/NEJMoa0810866 http://www.ncbi.nlm.nih.gov/pubmed/19726771?tool=bestpractice.com Adverse events are localized to the injection site, generally of mild-to-moderate severity, and transient in nature.[30]Badalamente MA, Hurst LC. Efficacy and safety of injectable mixed collagenase subtypes in the treatment of Dupuytren's contracture. J Hand Surg Am. 2007 Jul-Aug;32(6):767-74. http://www.ncbi.nlm.nih.gov/pubmed/17606053?tool=bestpractice.com The most commonly reported adverse events were localized swelling in the hand, pain, bruising, pruritus, and transient regional lymph-node enlargement and tenderness. Serious adverse events were seen in 2% of collagenase recipients, including tendon ruptures and complex regional pain syndrome.[31]Hurst LC, Badalamente MA, Hentz VR, et al. Injectable collagenase clostridium histolyticum for Dupuytren's contracture. N Engl J Med. 2009 Sep 3;361(10):968-79. https://www.nejm.org/doi/full/10.1056/NEJMoa0810866 http://www.ncbi.nlm.nih.gov/pubmed/19726771?tool=bestpractice.com Although there is some literature with small numbers of patients to suggest that recurrence is more common in PIP joint contractures than in MCP joint contractures, additional long-term studies involving larger numbers of patients are warranted to verify the long-term effectiveness and recurrence rates of collagenase treatment, as well as its long-term safety.[32]Watt AJ, Curtin CM, Hentz VR. Collagenase injection as nonsurgical treatment of Dupuytren's disease: 8-year follow-up. J Hand Surg Am. 2010 Apr;35(4):534-9. http://www.ncbi.nlm.nih.gov/pubmed/20353858?tool=bestpractice.com
One systematic review has found that having previous surgery did not affect the efficacy and safety of collagenase injections, making this an option in patients with recurrent Dupuytren contracture.[34]Bainbridge C, Gerber RA, Szczypa PP, et al. Efficacy of collagenase in patients who did and did not have previous hand surgery for Dupuytren's contracture. J Plast Surg Hand Surg. 2012 Sep;46(3-4):177-83. http://informahealthcare.com/doi/pdf/10.3109/2000656X.2012.683795 http://www.ncbi.nlm.nih.gov/pubmed/22670890?tool=bestpractice.com
After the injection is given, a dressing is placed on the hand. The patient is then instructed to return to the office the next day for the finger extension maneuver, in which the finger is extended to break the cord. This may be done with or without a local anesthetic. After the manipulation is successfully completed, there are no restrictions and early movement is encouraged. Although wearing a nighttime splint afterward has not been proven to decrease recurrence, it should be offered to the patient. The patient is followed to assess the need for up to 2 further injections every 4 to 6 weeks.[30]Badalamente MA, Hurst LC. Efficacy and safety of injectable mixed collagenase subtypes in the treatment of Dupuytren's contracture. J Hand Surg Am. 2007 Jul-Aug;32(6):767-74. http://www.ncbi.nlm.nih.gov/pubmed/17606053?tool=bestpractice.com
Primary options
collagenase clostridium histolyticum: 0.58 mg intralesionally as a single dose, maximum 3 doses/cord
More collagenase clostridium histolyticumMay repeat 2 doses at intervals of 4 weeks if the contracture remains.
needle aponeurotomy
Under sterile conditions, the area is anesthetized with lidocaine and an 18-gauge needle is used to puncture the aponeurotic band causing the digital contracture. This weakens the contracture until it can be broken by mechanical force, typically with a characteristic snap. The needle is introduced volar (palmar side) to the tendon at various sites progressing from proximal to distal. Care must be taken not to insert the needle into the tendon, to avoid iatrogenic injury. Use of ultrasound to guide the procedure may reduce the risk of accidental lesions.[62]Sakellariou VI, Brault J, Rizzo M. Ultrasound-assisted percutaneous needle fasciotomy for Dupuytren's contracture. Orthopedics. 2015 May;38(5):299-303. http://www.ncbi.nlm.nih.gov/pubmed/25970356?tool=bestpractice.com
This procedure is usually successful in correcting the contracture, takes very little time to perform (20-30 minutes), requires only local anesthesia, and is not very painful. In comparison with open surgical procedures, it results in similar resolution, minimal scarring, faster recovery, and can be repeated easily if the contracture recurs.[35]Toppi JT, Trompf L, Smoll NR, et al. Dupuytren's contracture: an analysis of outcomes of percutaneous needle fasciotomy versus open fasciectomy. ANZ J Surg. 2015 Sep;85(9):639-43. http://www.ncbi.nlm.nih.gov/pubmed/24438029?tool=bestpractice.com [36]Zhou C, Selles RW, Slijper HP, et al. Comparative effectiveness of percutaneous needle aponeurotomy and limited fasciectomy for Dupuytren's contracture: a multicenter observational study. Plast Reconstr Surg. 2016 Oct;138(4):837-46. http://www.ncbi.nlm.nih.gov/pubmed/27307334?tool=bestpractice.com [37]van Rijssen AL, Gerbrandy FS, Ter Linden H, et al. A comparison of the direct outcomes of percutaneous needle fasciotomy and limited fasciectomy for Dupuytren's disease: a 6-week follow-up study. J Hand Surg Am. 2006 May-Jun;31(5):717-25. http://www.ncbi.nlm.nih.gov/pubmed/16713831?tool=bestpractice.com Needle aponeurotomy is thus an attractive option for patients with less aggressive and early disease.[38]Foucher G, Medina J, Navarro R. Percutaneous needle aponeurotomy: complications and results. J Hand Surg Br. 2003 Oct;28(5):427-31. http://www.ncbi.nlm.nih.gov/pubmed/12954251?tool=bestpractice.com Recurrence rates of up to 58% have been reported during 3 to 5 years of follow-up, but long-term outcomes are not well reported.[40]Chen NC, Srinivasan RC, Shauver MJ, et al. A systematic review of outcomes of fasciotomy, aponeurotomy, and collagenase treatments for Dupuytren's contracture. Hand (N Y). 2011 Sep;6(3):250-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3153627 http://www.ncbi.nlm.nih.gov/pubmed/22942847?tool=bestpractice.com
All patients with contractures should receive hand therapy postprocedure.
percutaneous fasciotomy
A similar procedure to needle aponeurotomy, but uses a scalpel to cut and release the band causing the digital contracture and is thus performed by a hand surgeon in the operating room.[43]Rowley DI, Couch M, Chesney RB, et al. Assessment of percutaneous fasciotomy in the management of Dupuytren's contracture. J Hand Surg Br. 1984 Jun;9(2):163-4. http://www.ncbi.nlm.nih.gov/pubmed/6747419?tool=bestpractice.com [44]Colville J. Dupuytren's contracture - the role of fasciotomy. Hand. 1983 Jun;15(2):162-6. http://www.ncbi.nlm.nih.gov/pubmed/6884846?tool=bestpractice.com The finger is brought into full extension with a characteristic snap.
This procedure causes less pain and allows a faster recovery than traditional open fasciectomy interventions. However, it is associated with a risk of recurrence of up to 43%, as diseased fascia is unavoidably left behind, and there is risk of flexor tendon or nerve injury.[43]Rowley DI, Couch M, Chesney RB, et al. Assessment of percutaneous fasciotomy in the management of Dupuytren's contracture. J Hand Surg Br. 1984 Jun;9(2):163-4. http://www.ncbi.nlm.nih.gov/pubmed/6747419?tool=bestpractice.com [44]Colville J. Dupuytren's contracture - the role of fasciotomy. Hand. 1983 Jun;15(2):162-6. http://www.ncbi.nlm.nih.gov/pubmed/6884846?tool=bestpractice.com [45]Bryan AS, Ghorbal MS. The long-term results of closed palmar fasciotomy in the management of Dupuytren's contracture. J Hand Surg Br. 1988 Aug;13(3):254-6. http://www.ncbi.nlm.nih.gov/pubmed/3171286?tool=bestpractice.com
All patients with contractures should receive hand therapy postprocedure.
corticosteroid injections
Patients who wish to avoid a more invasive procedure may benefit from corticosteroid injections.
The injection of Dupuytren nodules with triamcinolone acetonide monthly for up to 5 months or every 6 weeks for 3 injections has been shown to produce significant regression of the disease, with an average of 3.2 injections per nodule required for improvement of function.[28]Ketchum LD, Donahue TK. The injection of nodules of Dupuytren's disease with triamcinolone acetonide. J Hand Surg Am. 2000 Nov;25(6):1157-62. http://www.ncbi.nlm.nih.gov/pubmed/11119679?tool=bestpractice.com After corticosteroid injection, fewer patients progress to surgery than would be predicted with expectant management alone.[28]Ketchum LD, Donahue TK. The injection of nodules of Dupuytren's disease with triamcinolone acetonide. J Hand Surg Am. 2000 Nov;25(6):1157-62. http://www.ncbi.nlm.nih.gov/pubmed/11119679?tool=bestpractice.com
All patients with contractures should receive hand therapy postprocedure.
Primary options
triamcinolone acetonide: consult specialist for guidance on dose
>30 degrees MCP joint contracture and/or PIP joint contracture
open partial fasciectomy + perioperative antibiotics
The most common procedure used in the surgical management of Dupuytren contracture, as it is associated with a postoperative recurrence rate of 15%.[49]Townley WA, Baker R, Sheppard N, et al. Dupuytren's contracture unfolded. BMJ. 2006;332:397-400. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1370973 http://www.ncbi.nlm.nih.gov/pubmed/16484265?tool=bestpractice.com
Through a transverse palmar incision overlying the distal palmar crease, the fascia forming pathologic cords is excised in a proximal-to-distal direction. [Figure caption and citation for the preceding image starts]: Preoperative view of the ring finger of a patient with a flexion contracture with surgical indications, showing the incision marking, demonstrating a transverse incision overlying the distal palmar crease, and oblique Brunner incisions coursing from it proximally and distallyFrom the collection of Dr C.M. Rodner; used with permission [Citation ends].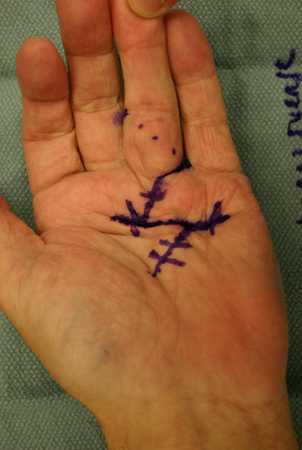 The choice of digital incision is surgeon-dependent and is most often between a Brunner and a longitudinal incision (often combined with multiple Z-plasties).
The choice of digital incision is surgeon-dependent and is most often between a Brunner and a longitudinal incision (often combined with multiple Z-plasties).
In the palm, the neurovascular structures deep to the involved fascia are identified and retracted. [Figure caption and citation for the preceding image starts]: Intraoperative view of the ring finger of a patient with a flexion contracture, with the radial digital neurovascular bundle identified and isolated coursing volar over the Dupuytren cord, which is being held up by forceps as it is excised in a proximal-to-distal directionFrom the collection of Dr C.M. Rodner; used with permission [Citation ends]. The diseased fascia is excised and elevated in a proximal-to-distal direction. As the Dupuytren cord moves into the finger, care is taken to identify the radial and ulnar digital arteries and nerves, particularly in PIP joint contractures. The joints are inspected for persistent contractures, and residual contracture of the PIP joint is addressed with a release of the volar plate followed by release of the collateral ligaments if necessary.
The diseased fascia is excised and elevated in a proximal-to-distal direction. As the Dupuytren cord moves into the finger, care is taken to identify the radial and ulnar digital arteries and nerves, particularly in PIP joint contractures. The joints are inspected for persistent contractures, and residual contracture of the PIP joint is addressed with a release of the volar plate followed by release of the collateral ligaments if necessary.
When possible, direct primary closure of the palmar skin is performed over a Penrose drain to prevent hematoma, as this method of closure allows for early motion and good skin sensibility, avoiding the meticulous wound care required with an open wound. [Figure caption and citation for the preceding image starts]: Postoperative view of the ring finger of a patient with a flexion contracture, showing the closed wound over a Penrose drain, which is used to minimize subsequent hematoma formationFrom the collection of Dr C.M. Rodner; used with permission [Citation ends]. If the palmar defect is too large for primary closure, skin grafting or the McCash "open-palm" technique are used. The patient is followed up within a few days to pull out the drain and assess the wound.
If the palmar defect is too large for primary closure, skin grafting or the McCash "open-palm" technique are used. The patient is followed up within a few days to pull out the drain and assess the wound.
All patients with contractures should receive hand therapy postprocedure. After an open partial fasciectomy, flexion exercises begin once the wound has stabilized.
Postoperative infection is countered with the use of perioperative antibiotics and careful soft tissue handling. Cefazolin is the agent of choice. Clindamycin can be used as an alternative in patients with penicillin allergy, to provide gram-positive cover.
Primary options
cefazolin: 1g intravenously administered 30 minutes to 1 hour prior to the start of surgery
Secondary options
clindamycin: 600 mg intravenously administered 30 minutes to 1 hour prior to the start of surgery
postoperative splinting
Treatment recommended for SOME patients in selected patient group
After an open partial fasciectomy, the fingers can be splinted in full extension.
By the fifth postoperative day, patients are sent to the hand therapist for a forearm-based digital extension splint that is worn full time between therapy visits. Flexion exercises begin once the wound has stabilized. Regaining digital flexion often proves more difficult than maintaining extension after fasciectomy, due to the postoperative extension splinting required. [Figure caption and citation for the preceding image starts]: One-month postoperative view of the ring finger of a patient with a flexion contracture, demonstrating full active digital extensionFrom the collection of Dr C.M. Rodner; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: One-month postoperative view of the ring finger of a patient with a flexion contracture, demonstrating active digital flexionFrom the collection of Dr C.M. Rodner; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: One-month postoperative view of the ring finger of a patient with a flexion contracture, demonstrating active digital flexionFrom the collection of Dr C.M. Rodner; used with permission [Citation ends]. By the third postoperative week the splint is weaned, to be worn at night only, and nighttime extension splinting can continue for as long as 6 months.
By the third postoperative week the splint is weaned, to be worn at night only, and nighttime extension splinting can continue for as long as 6 months.
Some surgeons have abandoned postoperative splinting, favoring earlier mobilization in order to minimize difficulties with flexion. There is also evidence to suggest that splinting (including nighttime extension splinting) after surgery provides no additional benefit to standard hand therapy in maintaining finger extension, except perhaps for cases in which extension loss occurs postoperatively, whereby nighttime extension splinting may provide some benefit.[53]Kemler MA, Houpt P, van der Horst CM. A pilot study assessing the effectiveness of postoperative splinting after limited fasciectomy for Dupuytren's disease. J Hand Surg Eur Vol. 2012 Oct;37(8):733-7. http://www.ncbi.nlm.nih.gov/pubmed/22311918?tool=bestpractice.com [54]Collis J, Collocott S, Hing W, et al. The effect of night extension orthoses following surgical release of Dupuytren contracture: a single-center, randomized, controlled trial. J Hand Surg Am. 2013 Jul;38(7):1285-94. http://www.ncbi.nlm.nih.gov/pubmed/23790420?tool=bestpractice.com Postoperative splinting may not be justified in all patients.
segmental aponeurotomy
A compromise between percutaneous techniques and open fasciectomy, in which multiple small incisions are made in the palm and the digits to remove segments of the Dupuytren cord and achieve discontinuity between the segments of diseased tissue, with no effort made to remove all of the pathologic tissue.
The clinical results of this technique compare quite well with traditional open fasciectomy techniques, with a recurrence rate ranging from 20% to 35%.[46]Rayan GM. Dupuytren disease: Anatomy, pathology, presentation, and treatment. J Bone Joint Surg Am. 2007 Jan;89(1):189-98. http://www.ncbi.nlm.nih.gov/pubmed/17256226?tool=bestpractice.com [47]Moermans JP. Long-term results after segmental aponeurectomy for Dupuytren's disease. J Hand Surg Br. 1996;21:797-800. http://www.ncbi.nlm.nih.gov/pubmed/8982932?tool=bestpractice.com [48]Moermans JP. Segmental aponeurectomy in Dupuytren's disease. J Hand Surg Br. 1991 Aug;16(3):243-54. http://www.ncbi.nlm.nih.gov/pubmed/1960487?tool=bestpractice.com
All patients with contractures should receive hand therapy postprocedure.
percutaneous fasciotomy
A similar procedure to needle aponeurotomy, but uses a scalpel to cut and release the band causing the digital contracture and is thus performed by a hand surgeon in the operating room.[43]Rowley DI, Couch M, Chesney RB, et al. Assessment of percutaneous fasciotomy in the management of Dupuytren's contracture. J Hand Surg Br. 1984 Jun;9(2):163-4. http://www.ncbi.nlm.nih.gov/pubmed/6747419?tool=bestpractice.com [44]Colville J. Dupuytren's contracture - the role of fasciotomy. Hand. 1983 Jun;15(2):162-6. http://www.ncbi.nlm.nih.gov/pubmed/6884846?tool=bestpractice.com The finger is brought into full extension with a characteristic snap.
This procedure causes less pain and allows a faster recovery than traditional open fasciectomy interventions. However, it is associated with a risk of recurrence of up to 43%, as diseased fascia is unavoidably left behind, and there is a risk of flexor tendon or nerve injury.[43]Rowley DI, Couch M, Chesney RB, et al. Assessment of percutaneous fasciotomy in the management of Dupuytren's contracture. J Hand Surg Br. 1984 Jun;9(2):163-4. http://www.ncbi.nlm.nih.gov/pubmed/6747419?tool=bestpractice.com [44]Colville J. Dupuytren's contracture - the role of fasciotomy. Hand. 1983 Jun;15(2):162-6. http://www.ncbi.nlm.nih.gov/pubmed/6884846?tool=bestpractice.com [45]Bryan AS, Ghorbal MS. The long-term results of closed palmar fasciotomy in the management of Dupuytren's contracture. J Hand Surg Br. 1988 Aug;13(3):254-6. http://www.ncbi.nlm.nih.gov/pubmed/3171286?tool=bestpractice.com
All patients with contractures should receive hand therapy postprocedure.
collagenase injection
Collagenase clostridium histolyticum is used to treat adult patients with a palpable cord along with metacarpophalangeal (MCP) joint contracture or proximal interphalangeal (PIP) joint contracture, with a corresponding decrease in both fasciotomies and fasciectomies.[29]Lipman MD, Carstensen SE, Deal DN. Trends in the treatment of Dupuytren disease in the United States between 2007 and 2014. Hand (N Y). 2017 Jan;12(1):13-20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5207289 http://www.ncbi.nlm.nih.gov/pubmed/28082837?tool=bestpractice.com A mean of 1.4 injections is required to normalize affected joints, and clinical success is achieved within 29 days.[30]Badalamente MA, Hurst LC. Efficacy and safety of injectable mixed collagenase subtypes in the treatment of Dupuytren's contracture. J Hand Surg Am. 2007 Jul-Aug;32(6):767-74. http://www.ncbi.nlm.nih.gov/pubmed/17606053?tool=bestpractice.com In one study, reductions in contracture to 0 to 5 degrees of full extension, 30 days after the last injection, were achieved in cords injected with collagenase as compared with those injected with placebo.[31]Hurst LC, Badalamente MA, Hentz VR, et al. Injectable collagenase clostridium histolyticum for Dupuytren's contracture. N Engl J Med. 2009 Sep 3;361(10):968-79. https://www.nejm.org/doi/full/10.1056/NEJMoa0810866 http://www.ncbi.nlm.nih.gov/pubmed/19726771?tool=bestpractice.com Adverse events are localized to the injection site, generally of mild-to-moderate severity, and transient in nature.[30]Badalamente MA, Hurst LC. Efficacy and safety of injectable mixed collagenase subtypes in the treatment of Dupuytren's contracture. J Hand Surg Am. 2007 Jul-Aug;32(6):767-74. http://www.ncbi.nlm.nih.gov/pubmed/17606053?tool=bestpractice.com The most commonly reported adverse events were localized swelling in the hand, pain, bruising, pruritus, and transient regional lymph-node enlargement and tenderness. Serious adverse events were seen in 2% of collagenase recipients, including tendon ruptures and complex regional pain syndrome.[31]Hurst LC, Badalamente MA, Hentz VR, et al. Injectable collagenase clostridium histolyticum for Dupuytren's contracture. N Engl J Med. 2009 Sep 3;361(10):968-79. https://www.nejm.org/doi/full/10.1056/NEJMoa0810866 http://www.ncbi.nlm.nih.gov/pubmed/19726771?tool=bestpractice.com Although there is some literature with small numbers of patients to suggest that recurrence is more common in PIP joint contractures than in MCP joint contractures, additional long-term studies involving larger numbers of patients are warranted to verify the long-term effectiveness and recurrence rates of collagenase treatment, as well as its long-term safety.[32]Watt AJ, Curtin CM, Hentz VR. Collagenase injection as nonsurgical treatment of Dupuytren's disease: 8-year follow-up. J Hand Surg Am. 2010 Apr;35(4):534-9. http://www.ncbi.nlm.nih.gov/pubmed/20353858?tool=bestpractice.com
One systematic review has found that having previous surgery did not affect the efficacy and safety of collagenase injections, making this an option in patients with recurrent Dupuytren contracture.[34]Bainbridge C, Gerber RA, Szczypa PP, et al. Efficacy of collagenase in patients who did and did not have previous hand surgery for Dupuytren's contracture. J Plast Surg Hand Surg. 2012 Sep;46(3-4):177-83. http://informahealthcare.com/doi/pdf/10.3109/2000656X.2012.683795 http://www.ncbi.nlm.nih.gov/pubmed/22670890?tool=bestpractice.com
After the injection is given, a dressing is placed on the hand. The patient is then instructed to return to the office the next day for the finger extension maneuver, in which the finger is extended to break the cord. This may be done with or without a local anesthetic. After the manipulation is successfully completed, there are no restrictions and early movement is encouraged. Although wearing a nighttime splint afterward has not been proven to decrease recurrence, it should be offered to the patient. The patient is followed to assess the need for up to 2 further injections every 4 to 6 weeks.[30]Badalamente MA, Hurst LC. Efficacy and safety of injectable mixed collagenase subtypes in the treatment of Dupuytren's contracture. J Hand Surg Am. 2007 Jul-Aug;32(6):767-74. http://www.ncbi.nlm.nih.gov/pubmed/17606053?tool=bestpractice.com
Primary options
collagenase clostridium histolyticum: 0.58 mg intralesionally as a single dose, maximum 3 doses/cord
More collagenase clostridium histolyticumMay repeat 2 doses at intervals of 4 weeks if the contracture remains.

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer