History and exam
Key diagnostic factors
common
known underlying medical cause
Includes blepharitis, connective tissue disorders, vitamin A deficiency, hepatitis C, HIV, hematopoietic stem cell transplantation, laser in situ keratomileusis, contact lens use, diabetes mellitus, sarcoidosis, and Parkinson disease.
use of known causative medications
Includes preserved topical ophthalmic medications, postmenopausal hormone replacement therapy, oral contraceptives, antihistamines, beta-blockers, anticholinergics, diuretics, some psychotropic drugs, and retinoids.
corneal filaments
Small comma shaped strands, attached at one end to the cornea (corresponding to the lid aperture) may be evident on slit-lamp examination after staining with fluorescein or rose bengal.
Other diagnostic factors
common
ocular irritation/foreign body sensation
These nonspecific symptoms can be indicative of dry eye. Symptom severity does not always correlate with signs.[35]
ocular burning
This nonspecific symptom can be indicative of dry eye. Symptom severity does not always correlate with signs.[35]
transient blurred vision
Intermittent visual blurring may occur.
tearing
Reflex watering may be experienced with ocular surface irritation and also in patients with diabetes.
blepharitis/meibomianitis
Eyelid margin inflammation may be present on examination. [Figure caption and citation for the preceding image starts]: BlepharitisPrivate collection of Dr Jonathan Smith and Dr Philip Severn; used with permission [Citation ends].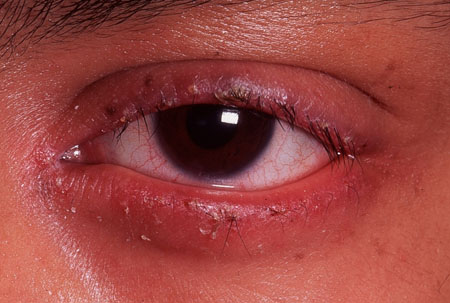
punctate epithelial erosions
Fine punctate staining of the inferior cornea (corresponding to the lid aperture) may be evident on slit-lamp examination after staining with fluorescein or rose bengal.
conjunctival punctate erosions
Fine punctate staining of the conjunctiva may be evident on slit-lamp examination after staining with fluorescein, rose bengal, or lissamine green stain. [Figure caption and citation for the preceding image starts]: Dry eye (stained with rose bengal)Private collection of Dr Jonathan Smith and Dr Philip Severn; used with permission [Citation ends].
conjunctival injection
Injected conjunctiva may be a presenting sign.
uncommon
lagophthalmos
Inability to fully close lid apertures leads to increased tear film evaporation.
proptosis
Eyeball protrusion or displacement can lead to difficulty with lid closing. This leads to increased tear film evaporation.
presence of mites
Careful examination of the base of the eyelashes may reveal Demodex mites, which can cause ocular irritation and refractory dry eye.
Risk factors
strong
female sex
older age
blepharitis/meibomianitis
Eyelid margin inflammation may pre-empt dry eye.[3][Figure caption and citation for the preceding image starts]: BlepharitisPrivate collection of Dr Jonathan Smith and Dr Philip Severn; used with permission [Citation ends].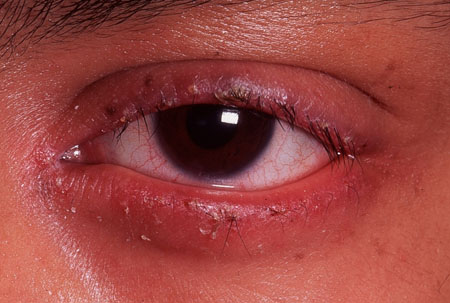
connective tissue disorders
Many connective tissue disorders, including Sjögren syndrome, rheumatoid arthritis, systemic lupus erythematosus, systemic sclerosis (scleroderma), and mixed connective tissue disorder), are associated with lacrimal acinar damage and dry eye.[3]
vitamin A deficiency
Dry eye, with or without aqueous deficiency, can occur with vitamin A deficiency, which affects tear film instability.[3]
hematopoietic stem cell transplantation
Dry eye has been reported in allograft recipients and is a common complication of graft versus host disease.[21]
lens and eyelid surgery
Dry eye is a common complication of ocular surgery (e.g., prior keratoplasty, cataract surgery, and keratorefractive surgery) and eyelid surgery (e.g., punctal cautery, prior ptosis repair, blepharoplasty, entropion/ectropion repair).[2]
contact lens use
Contact lens use causes tear film hyperosmolarity; however, scleral lenses may be beneficial to selected patients as they can help the healing of persistent corneal epithelial defects secondary to dry eye.[13]
diabetes mellitus
Increased prevalence of dry eye has been reported in diabetic patients.[3]
systemic medications
Many systemic medications (including antiandrogenic treatments, oral contraceptives, antihistamines, beta-blockers, anticholinergics, diuretics, some psychotropic drugs, and retinoids) are known to cause dry eye.[3]
Postmenopausal hormone replacement therapy has been linked with an increased risk of dry eye.[16]
The mechanisms of action vary depending on specific pharmacologic properties.
preserved topical ophthalmic medications
Parkinson disease
Patients may develop dry eye due to autonomic dysfunction and reduced blink rates.[11]
weak
environmental factors
Environmental factors such as wind, low humidity, and increased air temperature can worsen dry eye by increasing tear film evaporation.[3]
occupational factors
Occupations requiring sustained visual attention, such as microscope work and computer screen usage, can reduce blink rates and increase tear evaporation.[3]
headache
One meta-analysis of 11 studies demonstrated headache, particularly migraine, as an independent risk factor for dry eye disease.[23]
Use of this content is subject to our disclaimer