Tests
1st tests to order
electromyogram (EMG)
Test
EMG should be performed for every patient presenting with clinical MNM.
The clinician should specify the clinically affected limb or limbs with attention to the specific nerves that appear to be affected. The clinical suspicion of MNM should also be noted.
Diagnostic sensitivity is high if the clinically involved nerves are compared with unaffected nerves.
The typical findings in a primary or secondary vasculitis leading to MNM are of an axonal, active, asymmetrical or multifocal, distally predominant sensorimotor neuropathy.
EMG can distinguish MNM caused by vasculitis, infection, or neoplastic infiltration from multiple entrapment neuropathies and multifocal demyelinating neuropathies (i.e., multifocal chronic inflammatory demyelinating polyradiculoneuropathy; also known as Lewis-Sumner syndrome).
EMG should also be used to guide the site of nerve or muscle/nerve biopsy. Preferably, a biopsy is done on an affected but not dead nerve.
Consultation with a neuromuscular neurologist should be considered when EMG is ordered.
Result
abnormal EMG typical of MNM
CBC with differential
Test
Anemia, leukocytosis, and thrombocytosis have been reported in a majority of patients with systemic vasculitic neuropathy, and a sizable minority of patients with nonsystemic vasculitic neuropathy.
Result
anemia, eosinophilia, leukocytosis, thrombocytosis
erythrocyte sedimentation rate (ESR)
C-reactive protein (CRP)
Test
CRP is an alternative marker to erythrocyte sedimentation rate for systemic inflammation.
The frequency of elevation in systemic and nonsystemic vasculitic neuropathy is not well defined.
Result
elevated
serum creatinine
Test
Elevated serum creatinine indicates renal involvement.
Renal manifestations are common in granulomatosis with polyangiitis (formerly known as Wegener granulomatosis), microscopic polyarteritis, and classic polyarteritis nodosa. Severe renal failure is common in these conditions.
Renal manifestations are uncommon and usually mild in patients with eosinophilic granulomatosis with polyangiitis (formerly known as Churg-Strauss syndrome).[34]
Result
elevated
serum glucose
Test
Diabetes mellitus may cause either MNM or a diabetic lumbosacral radiculoplexus neuropathy.[1]
Result
elevated
cryoglobulins
serum complement
Test
Complement was reported to be decreased in 50% to 90% of patients with systemic lupus erythematosus, rheumatoid vasculitis, essential mixed cryoglobulinemia, or Sjogren syndrome; around 25% of patients with classic polyarteritis nodosa; and around 10% of patients with nonsystemic vasculitic neuropathy.[1]
Result
decreased
hepatitis B surface antigen
Test
Typically found in patients with hepatitis B-associated polyarteritis nodosa.[1]
Result
positive
hepatitis C antibodies or RNA
Test
Hepatitis C antibodies and/or circulating RNA are present in hepatitis C-associated essential mixed cryoglobulinemia or hepatitis C-associated polyarteritis nodosa.[1]
Result
positive
anti-HIV antigens or HIV RNA
Test
Positive in patients with an HIV infection.[1]
Result
positive
Lyme disease antibodies
Test
Positive in patients with Lyme disease.[1]
Result
positive
cytoplasmic and perinuclear antineutrophil cytoplasmic antibodies (c-ANCA and p-ANCA)
Test
Anti-proteinase 3 tests are used to detect a cytoplasmic pattern (c-ANCA). Anti-myeloperoxidase tests are used to detect a perinuclear pattern (p-ANCA).
c-ANCA is present in most patients with active granulomatosis with polyangiitis (formerly known as Wegener granulomatosis). The specificity of a positive c-ANCA result for granulomatosis with polyangiitis is 80% to 100%, with a sensitivity of 28% to 92%.[8]
c-ANCA may be present in about 30% of patients with microscopic polyarteritis or eosinophilic granulomatosis with polyangiitis (formerly known as Churg-Strauss syndrome).[50]
Specificity of a positive c-ANCA for microscopic polyarteritis or eosinophilic granulomatosis with polyangiitis is about 99%.[1][50]
p-ANCA is present in about half of patients with microscopic polyarteritis, one third of patients with eosinophilic granulomatosis with polyangiitis, and 10% of patients with granulomatosis with polyangiitis. Specificity for ANCA-associated vasculitis is 99%.[1][50][51]
c-ANCA is strongly associated with granulomatosis with polyangiitis in the correct clinical setting, but should not be used to justify initiation of immunosuppression, for which a tissue diagnosis is required.[8]
Result
elevated
rheumatoid factor
Test
Rheumatoid factor was reported to be present in 60% to 90% of patients with rheumatoid vasculitis, essential mixed cryoglobulinemia, or Sjogren syndrome; around 25% of patients with classic polyarteritis nodosa; and around 10% of patients with nonsystemic vasculitic neuropathy.[1][34]
Result
positive
antinuclear antibodies (ANA)
anti-double-stranded (ds) DNA
Test
Positive in patients with systemic lupus erythematosus.[1]
Result
positive
anti-Sjogren syndrome-related antigen A (SSA) or -SSB antibodies
Test
Positive in cases of systemic lupus erythematosus and in Sjogren syndrome.[1]
Result
positive
serum angiotensin-converting enzyme
Test
May be elevated in about 50% of patients with sarcoidosis, but sensitivity may be lower for isolated sarcoid neuropathy.[47]
Result
elevated
protein electrophoresis and immunofixation
Test
A monoclonal band may be present in patients with monoclonal gammopathy of unknown significance, lymphoma, lymphocytic leukemia, myeloproliferative disorder, or amyloidosis.
A monoclonal band is not usually found in cases of vasculitic neuropathy.
The presence of a monoclonal gammopathy in a patient with MNM should prompt further investigation.
Determination of the significance of a positive band must be made in combination with electrodiagnostic and biopsy results. A skeletal survey must be performed to assess for osteosclerotic myeloma, and consultation with a hematologist may be necessary.
Result
monoclonal band
chest x-ray
Test
Abnormal findings are consistent with a systemic vasculitis involving the lungs or sarcoidosis.
In patients with eosinophilic granulomatosis with polyangiitis (formerly known as Churg-Strauss syndrome), infiltrates are present in most patients but are often nonspecific. Bilateral multifocal consolidation in a patchy nonsegmental distribution is common.[51]
In patients with sarcoidosis, symmetric bilateral hilar adenopathy is present in about 85% of patients, and unilateral hilar adenopathy in 5%. Chest computed tomography is more sensitive than an x-ray.[52]
Result
abnormal findings
urinalysis
Test
Findings implicate a systemic vasculitis or malignancy involving the kidneys.
Renal manifestations are common in granulomatosis with polyangiitis (formerly known as Wegener granulomatosis), microscopic polyarteritis, and systemic lupus erythematosus. Urinalysis may frequently reveal red blood cell (RBC) casts in these disorders.
Polyarteritis nodosa causes renal infarcts but not glomerulonephritis, so RBC casts are unusual. Proteinuria and hematuria may occur in patients with polyarteritis nodosa.[11]
Result
red cell casts, proteinuria, hematuria
muscle and nerve biopsy
Test
Nerve or muscle/nerve biopsy should be considered for every patient with clinical MNM. Nonsystemic vasculitic neuropathy can only be definitively diagnosed with a nerve biopsy.[23]
Biopsy is typically performed on a pure sensory nerve without motor supply (e.g., sural, distal superficial peroneal, posterior cutaneous nerve of the thigh, or superficial radial).
Histologic features of necrotizing vasculitis are generally found in the clinical syndrome of vasculitic MNM. [Figure caption and citation for the preceding image starts]: Medium-size artery and arterioles in epi- perineurium of sural nerve showing transmural dense mixed cell infiltrates, fibrinoid necrosis and luminal occlusion (arrow) in a case of polyarteritis nodosa. Note that the muscularis layer is interrupted and destroyed by the inflammatory infiltrate (arrowhead). Paraffin section; Hematoxylin and EosinFrom the personal collection of Professor Sakir Humayun Gultekin, MD, FCAP; used with permission [Citation ends].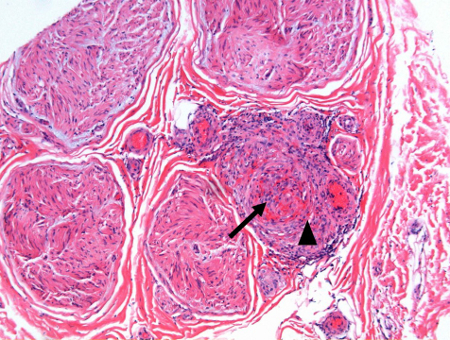 However, segmental nerve involvement and skip areas may fail to show vasculitis in the limited biopsy tissue.
However, segmental nerve involvement and skip areas may fail to show vasculitis in the limited biopsy tissue.
Combined muscle/nerve biopsy has been reported to improve the sensitivity of the biopsy compared with nerve biopsy alone.[3][53]
Biopsy and tissue diagnosis is important before starting a patient on long-term immunosuppressive agents, which carry significant side effects. In this context, an empirical therapy without tissue diagnosis is undesirable for this serious disorder.
Pathologic findings of significant demyelination rule out vasculitic or neoplastic neuropathy and may suggest an alternative diagnosis such as multifocal chronic inflammatory demyelinating polyradiculoneuropathy (Lewis-Sumner syndrome).[1]
Result
tissue evidence for neuropathy
Tests to consider
anti-Smith (anti-Sm) antibodies
Test
Positive in cases of systemic lupus erythematosus.[1]
Result
positive
anti-topoisomerase I (anti-Scl 70) and anti-centromere (ACA) antibodies
Test
Positive in patients with scleroderma.[1]
Result
positive
skin biopsy
Test
Biopsy of skin lesions such as palpable purpura, erythema, petechiae, nodules, maculopapules, and livedo reticularis may demonstrate characteristic findings of vasculitis.[54][55]
Skin scrapings of a lepromatous lesion demonstrate mycobacterium leprae.[56]
Result
abnormal findings consistent with vasculitis or infection
lip biopsy
Test
A lip biopsy (minor salivary gland biopsy) is more sensitive and specific than antibody tests for the diagnosis of Sjogren syndrome.
Result
abnormal findings consistent with Sjogren syndrome
anti-Hu antibodies
Test
Anti-Hu antibodies are associated with paraneoplastic MNM.
Anti-Hu should be requested if there is a suspicion of small-cell lung cancer or a paraneoplastic etiology.
Result
positive
cerebrospinal fluid (CSF) analyses
Test
Protein is elevated in 30% of patients with a vasculitic neuropathy, but is a nonspecific finding.
Protein may be elevated in sarcoidosis, infections of the central nervous system, and meningeal carcinomatosis.
Cytology may show evidence of neoplastic cells if meningeal carcinomatosis is suspected, but sensitivity is low. Repeat lumbar punctures and large-volume CSF samples (20-30 mL) raise sensitivity.
Lyme disease antibodies indicate MNM due to Lyme disease.
Human T-cell lymphotropic virus type 1 antibodies may be positive. Polymerase chain reaction may be positive for cytomegalovirus in patients with HIV infection.
Result
elevated protein, presence of infection or neoplasm
CT of chest, abdomen/pelvis
Test
Abnormal findings are consistent with a systemic vasculitis, sarcoidosis, or neoplasm.
In patients with eosinophilic granulomatosis with polyangiitis (formerly known as Churg-Strauss syndrome), lung infiltrates are present in most patients but are often nonspecific. Bilateral multifocal consolidation in a patchy nonsegmental distribution is common.[51]
Ground glass lung infiltrates are common in patients with granulomatosis with polyangiitis (formerly known as Wegener granulomatosis), microscopic polyarteritis, or severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) pneumonitis.[43][57]
Symmetric bilateral hilar adenopathy is present in about 85% of patients with sarcoidosis, and unilateral hilar adenopathy is present in another 5% of patients.
Abdomen/pelvis computed tomography is indicated if there is a clinical suspicion of lymphoma or other neoplasm as the underlying etiology for the neuropathy.
Result
abnormal findings
positron emission tomography (PET) scan of chest, abdomen, or pelvis
Test
Abnormal findings are consistent with malignancy. PET is more sensitive than computed tomography for a small tumor.
PET scanning may be useful if no definite cause is identified for MNM.
Result
abnormal findings
conventional angiography
Test
Abnormal findings are suggestive of a systemic vasculitis.
An angiogram of the visceral arteries is indicated if there is a clinical suspicion for polyarteritis nodosa. Characteristic findings include microaneurysms, beading from sequential areas of arterial narrowing and dilation, and stenosis.[8][58]
Result
abnormal findings
magnetic resonance angiography
Test
Abnormal findings are suggestive of a systemic vasculitis such as polyarteritis nodosa. Similar to conventional angiogram, findings could include microaneurysms, beading from sequential areas of arterial narrowing and dilation, and stenosis. Magnetic resonance angiography is generally not sensitive enough for evaluating a patient with suspected MNM and medium-, small-, or variable-size vessel vasculitis (primary nonsystemic vasculitic neuropathy).
Result
abnormal findings
Use of this content is subject to our disclaimer