Approach
Diagnosis is based on clinical findings, and confirmed with vaginal samples. Some evidence suggests that women frequently self-diagnose vaginitis and treat bacterial vaginosis and candidiasis with over-the-counter medications.[22]
Sexual partners of individuals with Trichomonas vaginalis should be offered screening for other STIs. Bacterial vaginosis and candidiasis are not typically sexually transmitted; however, they may occur concomitantly with STIs (e.g., gonorrhea and chlamydial infections) and therefore it is recommended to screen for STIs in all women with infective vaginitis. To aid the delivery of STI testing services, the World Health Organization recommends self-collection of samples as an option to test for N gonorrhoeae and C trachomatis and, where appropriate, T pallidum and T vaginalis.[23] The UK National Health and Care Excellence also recommends remote self-sampling be offered as an alternative to clinic attendance to improve uptake and frequency of STI testing.[24]
History
Precipitating factors for vaginitis could include shaving, douching, poor or excessive hygiene, and antibiotic, intrauterine device, or oral contraceptive pill use. In addition, a history of recent change in feminine hygiene products and/or soaps, or use of latex condoms or diaphragms, may be suggestive of irritant or allergic vaginitis. Infective vaginitis is more common during the reproductive years, whereas the menopause predisposes to atrophic vaginitis. Vulvovaginal candidiasis is more frequently seen in black women, and women with diabetes or HIV.[7][25] Weaker risk factors include smoking, more frequent intercourse, and pregnancy.[18][25]
The history should assess the entire spectrum of vaginal symptoms, including change in discharge, vaginal malodor, itching, dyspareunia, and dysuria. In addition to a description of symptoms, questions about the location of symptoms (vulva, vagina, and anus), duration, the response to prior treatment including self-treatment and douching, and a sexual history regarding number and gender identification of sexual partners, specific sexual practices and prior sexually transmitted infections, underlying medical conditions (e.g., diabetes, HIV status or inflammatory bowel disease), vulvovaginal hygiene practices, and relation of symptoms to the menstrual cycle can yield important insights into the likely etiology.[26]
Atrophic vaginitis is suggested by a history of dyspareunia, dryness, and dysuria in a postmenopausal woman and is diagnosed clinically. Women with vulvovaginal candidiasis often report a white, thick discharge like cottage cheese that is odorless, whereas women with bacterial vaginosis may report a malodorous, white discharge, which is often more noticeable following sexual intercourse.[27] In trichomoniasis, a sexually transmitted infection, the discharge is described as green, yellow, or white; frothy; and odorous.[4]
Vaginal bleeding may occur from cervicitis in trichomoniasis; rarely, it is also related to vaginal dryness in atrophic vaginitis.[4][28]
Fever and abdominal pain are very rare presenting symptoms and are usually associated with comorbid STIs.
Examination and vaginal samples
Examination involves external inspection of the genitalia and internal examination with a speculum.
Irritant or allergic vaginitis is typically diagnosed clinically, and examination may demonstrate erythema with or without edema.[29]
Atrophic vaginitis is typically diagnosed clinically based on history and evidence of atrophy on examination (decreased elasticity; dryness; friable, pale, shiny epithelium). Additional measures for diagnosis and assessment of treatment efficacy include vaginal pH, the vaginal maturation index (a calculation of the relative percentages of superficial cells compared to intermediate and parabasal cells), and evaluation of most bothersome symptom, in which women choose a symptom and rate severity (vaginal dryness, dyspareunia, vaginal irritation, dysuria, vaginal soreness, postcoital bleeding).[28]
Candidiasis is typically diagnosed clinically with evidence of erythema and a thick, white, cottage cheese-like discharge adherent to lateral vaginal walls, but may be confirmed by 10% potassium hydroxide (KOH) wet mount preparation or culture.
If bacterial vaginosis or trichomoniasis is suspected, vaginal samples for vaginal pH, amine ("whiff") test, saline, and KOH microscopy (wet mount) can aid diagnosis, together with clinical findings. [Figure caption and citation for the preceding image starts]: Trichomonas vaginitis with copious purulent discharge emanating from the cervical osCDC Image Library [Citation ends].
The pH and amine testing can be performed either through direct measurement or by colorimetric testing. It is important that the swab for pH evaluations be obtained from the mid-portion of the vaginal side wall to avoid false elevations in pH results caused by cervical mucus, blood, semen, or other products.[30]
An elevated pH is seen in bacterial infections and atrophic vaginitis.
Depending on institution preference, bacterial vaginosis may be diagnosed by vaginal Gram stain (Nugent criteria) or by the presence of at least 3 Amsel criteria:[26][31][32]
Vaginal pH >4.5
"Whiff" test
Clue cells (vaginal epithelial cells with distinctive stippled appearance in saline wet mount by being covered with bacteria)
Adherent white vaginal discharge.
[Figure caption and citation for the preceding image starts]: Photomicrograph revealing bacteria adhering to vaginal epithelial cells, known as clue cellsCDC Image Library; M. Rein [Citation ends].
In trichomoniasis, the wet mount reveals numerous white blood cells and motile protozoa.[Figure caption and citation for the preceding image starts]: Phase contrast wet mount micrograph of a vaginal discharge revealing the presence of Trichomonas vaginalis protozoaCDC Image Library [Citation ends].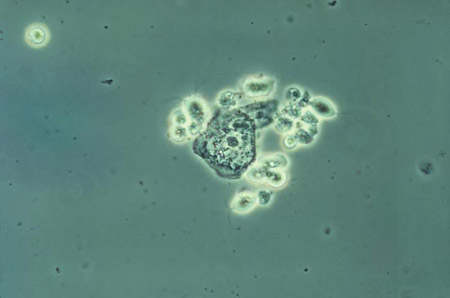 On inspection, the cervix may have a punctate and papilliform appearance (strawberry cervix).
On inspection, the cervix may have a punctate and papilliform appearance (strawberry cervix).
Laboratory tests
If the diagnosis is still uncertain, vaginal cultures or polymerase chain reaction tests for trichomoniasis or yeast may be warranted for infections that are resistant to treatment. These techniques are not carried out routinely.
A Gram stain of vaginal secretions for Nugent scoring of the bacterial flora identifies women with bacterial vaginosis.[26][32]
Other available tests for diagnosis include rapid tests for enzyme activity from bacterial vaginosis-associated organisms.[4][30][33][34]
STI testing is recommended in individuals with recurrent infections and/or those who are at risk of exposure to STIs (e.g., unprotected intercourse), and should include tests for gonorrhea, chlamydia, syphilis, and HIV.[4] Bacterial vaginosis and candidiasis are not typically sexually transmitted; however, they may occur concomitantly with STIs (e.g., gonorrhea and chlamydial infections) and therefore it is recommended to screen for STIs in all women with infective vaginitis.[35]
Use of this content is subject to our disclaimer