Approach
Patients with craniopharyngiomas most often present in one of four ways: raised intracranial pressure with accompanying hydrocephalus, visual loss, endocrine disturbance, or any of these in combination.[4][8][14][21][22]
Such presentations may be acute (sudden visual loss or symptoms of intracranial hypertension) or more insidious in onset. Symptoms of raised intracranial pressure (headache, nausea, vomiting, diplopia, decreased level of consciousness) always suggest a potential intracranial mass and warrant urgent contrast-enhanced cranial imaging (preferably magnetic resonance imaging [MRI]). Visual loss also warrants intracranial imaging to exclude a mass affecting the optic nerves or chiasm.
Although a provisional diagnosis may be made following a full clinical, imaging, and endocrine work-up, definitive diagnosis is following surgical biopsy/resection with pathologic analysis of tumor tissue.[23][Figure caption and citation for the preceding image starts]: Craniopharyngioma: adamantinous histology (low power) with complex arrangements of epithelium, cysts, and gliotic brainFrom the collection of Dr Marc C. Chamberlain [Citation ends].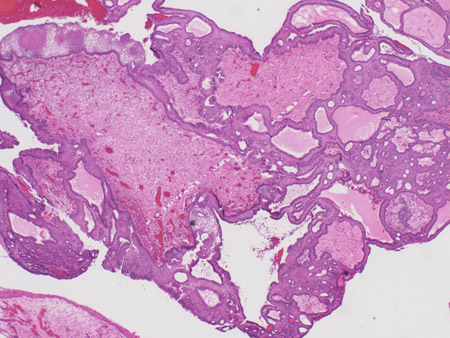 [Figure caption and citation for the preceding image starts]: Craniopharyngioma: adamantinous histology (medium power) with epithelial ribbons showing reticular areas and nodules of keratinFrom the collection of Dr Marc C. Chamberlain [Citation ends].
[Figure caption and citation for the preceding image starts]: Craniopharyngioma: adamantinous histology (medium power) with epithelial ribbons showing reticular areas and nodules of keratinFrom the collection of Dr Marc C. Chamberlain [Citation ends].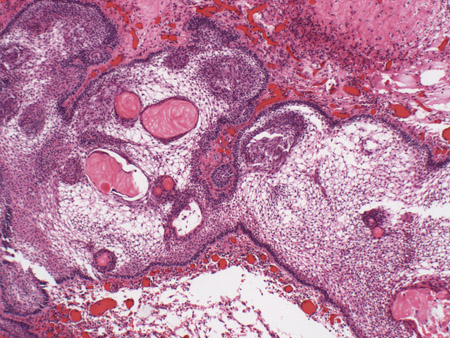 [Figure caption and citation for the preceding image starts]: Craniopharyngioma: adamantinous histology (high power) with basal-aligned columnar cells, stellate reticulum, and epithelial keratinizationFrom the collection of Dr Marc C. Chamberlain [Citation ends].
[Figure caption and citation for the preceding image starts]: Craniopharyngioma: adamantinous histology (high power) with basal-aligned columnar cells, stellate reticulum, and epithelial keratinizationFrom the collection of Dr Marc C. Chamberlain [Citation ends].
Clinical evaluation and recommended consultations
The majority of patients present with visual loss (either acuity or visual field); however, this may be challenging to ascertain in preverbal children. An ophthalmology consult is always indicated to perform formal visual field testing and assess the patient for optic atrophy and visual acuity. Furthermore, baseline assessment permits subsequent comparisons and response to treatment.[4][6][24]
Macrocephaly may be seen in infants with unfused intracranial sutures, as hydrocephalus secondary to ventricular outflow obstruction by an intracranial mass may occur.[3][4]
All patients require an endocrinologic assessment, as the majority manifest endocrine deficiencies; an endocrine consult is recommended.[4][8][9] In children with craniopharyngioma, growth hormone (GH) deficiency (causing growth failure) commonly precedes diagnosis.[25] A history of growth failure is confirmed by plotting height and weight on a standardized growth curve. Growth failure is, however, rarely a cause for referral prior to diagnosis of craniopharyngioma.[8][26]
Diabetes insipidus, suggested clinically by polyuria and polydipsia, may also be a presenting symptom in children and teenagers. In adults, amenorrhea or erectile dysfunction may indicate hypogonadotropic hypogonadism. Galactorrhea may also be a feature. Other common endocrinopathies include hypocortisolism, suggested by muscle weakness/fatigue, and hypothyroidism, which may manifest as fatigue, cold intolerance, or constipation.
Imaging
Contrast-enhanced cranial imaging is required in all patients with possible intracranial mass lesions.[27] MRI is preferred for anatomic localization, as the tumor is best appreciated in three planes (axial, coronal, and sagittal) and MRI better defines the tumor's anatomic relationship to adjacent structures. However, computed tomography (CT) imaging is helpful for ascertaining the presence of calcifications and cysts. Tumor location (e.g., sellar or chiasmatic) and appearance (dystrophic calcification, cystic component, contrast-enhancing solid component) are suggestive of craniopharyngioma.[Figure caption and citation for the preceding image starts]: Craniopharyngioma: coronal postcontrast MRIFrom the collection of Dr Marc C. Chamberlain [Citation ends].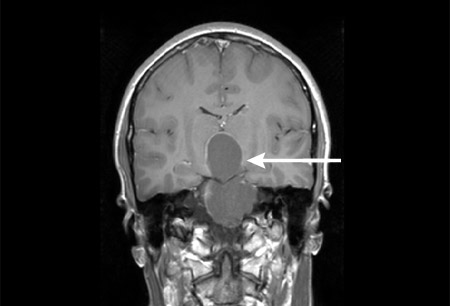 [Figure caption and citation for the preceding image starts]: Craniopharyngioma: axial postcontrast MRIFrom the collection of Dr Marc C. Chamberlain [Citation ends].
[Figure caption and citation for the preceding image starts]: Craniopharyngioma: axial postcontrast MRIFrom the collection of Dr Marc C. Chamberlain [Citation ends].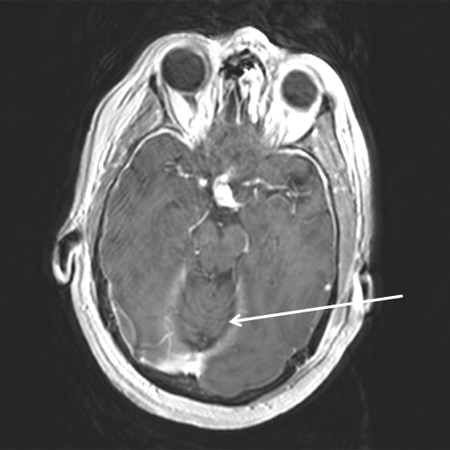 [Figure caption and citation for the preceding image starts]: Craniopharyngioma: sagittal postcontrast MRIFrom the collection of Dr Marc C. Chamberlain [Citation ends].
[Figure caption and citation for the preceding image starts]: Craniopharyngioma: sagittal postcontrast MRIFrom the collection of Dr Marc C. Chamberlain [Citation ends].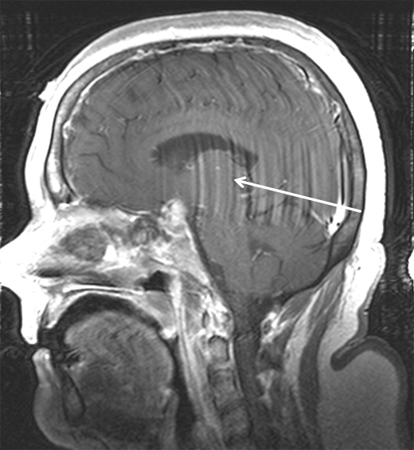 [Figure caption and citation for the preceding image starts]: Craniopharyngioma: sagittal postcontrast MRIFrom the collection of Dr Marc C. Chamberlain [Citation ends].
[Figure caption and citation for the preceding image starts]: Craniopharyngioma: sagittal postcontrast MRIFrom the collection of Dr Marc C. Chamberlain [Citation ends].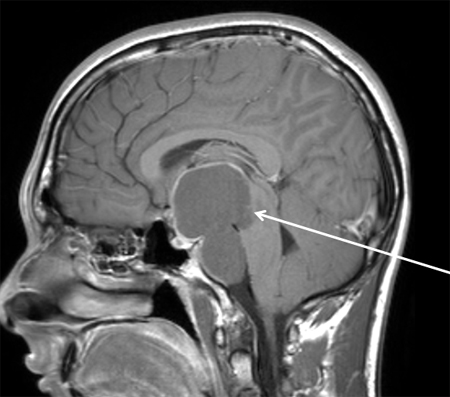
Laboratory evaluation
Because endocrine dysfunction is so common in patients with craniopharyngioma (30% to 80% of patients), both at presentation and following treatment, a careful endocrinologic baseline evaluation is required in all patients.[4][8][9] This aspect of care is best coordinated by a consulting endocrinologist and should include serum prolactin (often elevated), GH and related assays (serum GH levels as well as provocative stimulation, and serum insulin-like growth factor and growth factor protein levels), thyroid function (T3, T4, and thyroid-stimulating hormone), cortisol and serum adrenocorticotropic hormone levels, and an assessment for diabetes insipidus (serum sodium, serum/urine osmolality).
For assessment of hypogonadotropic hypogonadism, follicle-stimulating hormone and luteinizing hormone should be measured in both sexes and, in males, also testosterone.
Surgical biopsy or resection
Definitive diagnosis is following surgical biopsy/resection with pathologic analysis of tumor tissue.[23][Figure caption and citation for the preceding image starts]: Craniopharyngioma: adamantinous histology (low power) with complex arrangements of epithelium, cysts, and gliotic brainFrom the collection of Dr Marc C. Chamberlain [Citation ends].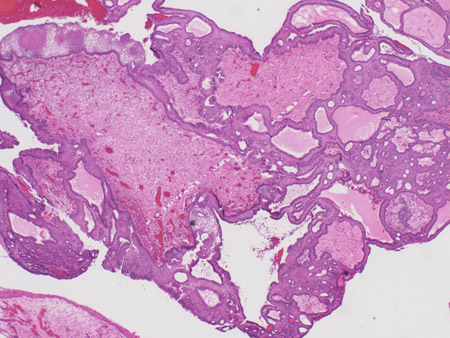 [Figure caption and citation for the preceding image starts]: Craniopharyngioma: adamantinous histology (medium power) with epithelial ribbons showing reticular areas and nodules of keratinFrom the collection of Dr Marc C. Chamberlain [Citation ends].
[Figure caption and citation for the preceding image starts]: Craniopharyngioma: adamantinous histology (medium power) with epithelial ribbons showing reticular areas and nodules of keratinFrom the collection of Dr Marc C. Chamberlain [Citation ends].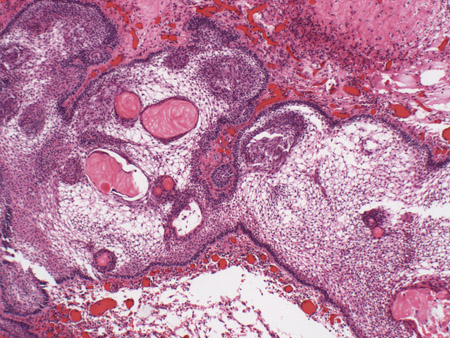 [Figure caption and citation for the preceding image starts]: Craniopharyngioma: adamantinous histology (high power) with basal-aligned columnar cells, stellate reticulum, and epithelial keratinizationFrom the collection of Dr Marc C. Chamberlain [Citation ends].
[Figure caption and citation for the preceding image starts]: Craniopharyngioma: adamantinous histology (high power) with basal-aligned columnar cells, stellate reticulum, and epithelial keratinizationFrom the collection of Dr Marc C. Chamberlain [Citation ends].
Use of this content is subject to our disclaimer