Tests
1st tests to order
cranial CT scan
Test
Cranial imaging should be performed as soon as possible in cases of suspected abusive head trauma in order to make the diagnosis and identify injuries that require surgical intervention.[1][40]
A CT scan of the brain is usually the first study performed because of speed and availability. In a small number of patients, subdural hemorrhage may not be present, either because it is not large enough to be apparent on CT or because the presence of significant brain edema may tamponade the blood before it can accumulate.[49][50]
In all cases of suspected abusive head trauma, 3-dimensional reconstruction should be performed to rule out skull fracture.
Further imaging with MRI is indicated if inflicted traumatic brain injury is diagnosed by CT or if there is a high suspicion of abusive head injury with a negative CT.[40][41][Figure caption and citation for the preceding image starts]: CT scan revealing subdural hemorrhage extending over the right convexity and in the intrahemispheric region, as well as enlargement of the extra-axial fluid spacesFrom the personal collection of Alice Newton, MD; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: CT findings in fatal abusive head trauma often reveal significant brain edema with loss of gray-white differentiation and effacement of the ventricles. Subdural blood is often difficult to appreciate in such casesFrom the personal collection of Alice Newton, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CT findings in fatal abusive head trauma often reveal significant brain edema with loss of gray-white differentiation and effacement of the ventricles. Subdural blood is often difficult to appreciate in such casesFrom the personal collection of Alice Newton, MD; used with permission [Citation ends].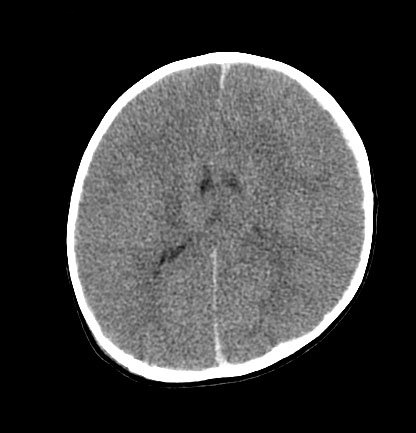
Result
subdural fluid collection, midline shift, skull fracture
CBC
Test
Subdural bleeding from inflicted traumatic brain injury may result in a drop in hematocrit (Hct) and, rarely, infants may require blood transfusion.
The greatest number of inflicted brain injury cases occurs when children are at a physiologic nadir of their Hct, so determining the etiology of a low Hct is complicated and may not be directly attributable to intracranial blood loss.
The WBC count may be elevated due to demargination of WBCs after trauma, and may not be indicative of infection.
Result
variable; Hct may be low, WBC count may be elevated
liver function tests
Test
There are commonly no external signs of abusive abdominal trauma, and elevated liver function tests may be the only clue to the presence of abdominal injury.[51]
Abusive abdominal injury may include hollow viscus perforation, blunt liver or splenic trauma, bowel wall hematoma, and renal, adrenal, or pancreatic contusion.
Result
elevated if abdominal injury present
toxicology screen
Test
The presence of a positive toxicology screen (for illicit drugs such as cocaine and marijuana) may reflect passive exposure in the home.
Care should be used in interpreting testing, as a positive test for benzodiazepines and opiates may be related to drugs used during resuscitation.
Result
variable
prothrombin time (PT)/activated PTT/fibrinogen/von Willebrand testing
Test
Coagulation studies should be performed along with thorough history taking to rule out any preexisting bleeding disorders.[31]
However, it must be noted that prothrombin prolongation and activated coagulation may result from parenchymal brain damage, especially in more severely injured children.[52]
Result
normal; may be abnormal in severe cases
urinalysis
Test
Urine should be tested for infection if fever is present and for glutaric aciduria type I if clinically indicated: for example, positive family history (autosomal recessive); macrocephaly; motor delay; and learning difficulties.[32][44][45]
Result
usually normal; dipstick positive for leukocytes, nitrates, and blood suggest infection; increased levels of glutaric, glutaconic, and 3-hydroxyglutaric acids suggests glutaric aciduria type I
cerebrospinal fluid analysis
Test
If clinical signs suggest meningitis or encephalitis, lumbar puncture should be ordered unless contraindicated.
In the case of trauma, the cerebrospinal fluid shows an abundance of red blood cells and normal glucose, and may reveal xanthochromia if injury occurred at least 8 to 12 hours before presentation.
Result
elevated WBC count if infection present; elevated red blood cell count or xanthochromia in cases of trauma
cranial MRI
Test
MRI may include T1- and T2-weighted sequences, gadolinium-enhanced imaging, proton density or fluid-attenuated inversion-recovery (FLAIR) imaging, diffusion-weighted imaging, and gradient echo T2-W sequences. In select cases, MR angiogram or venogram may also be included to rule out the possibility of aneurysm or intracranial venous thrombosis.[53]
MRI study is complementary to CT, and should be performed in all diagnosed cases of inflicted traumatic brain injury, as it can help discern between subarachnoid and subdural bleeding, and help further determine degree of brain injury, allowing prognostication. MRI is also indicated if high suspicion of abusive head injury persists subsequent to negative CT.[40][41]
MRI may identify subdural collections, cortical contusions, ischemia, intraparenchymal hemorrhage, and shearing injuries.[41]
The presence of mixed-density subdural hemorrhage does not necessarily indicate old and new injury, as this finding may occur with "hyperacute" bleeding or mixing of blood with cerebrospinal fluid when a tear in the arachnoid membrane occurs.[Figure caption and citation for the preceding image starts]: MRI depicting subdural hygromas surrounding severe brain atrophy from abusive head trauma. This child was initially erroneously diagnosed with meningitisFrom the personal collection of Alice Newton, MD; used with permission [Citation ends].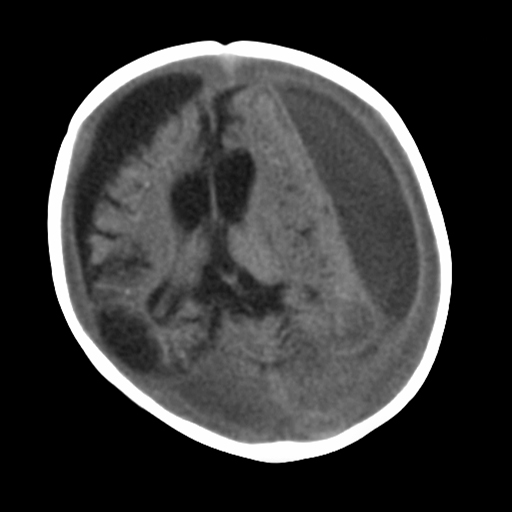
Result
subdural collections, cortical contusions, ischemia, intraparenchymal hemorrhage, and shearing injuries
Tests to consider
spinal MRI
Test
May be considered to assess for concurrent spinal injuries.[1]
Result
ligamentous injuries or spinal subdural hemorrhage
cranial ultrasound
Test
Cranial ultrasound is not sensitive enough for routine diagnostic use.[41]
In cases of unexplained increasing head circumference or in very unstable patients, cranial ultrasound can be helpful to detect subdural hemorrhage and to identify subarachnoid or subdural fluid collection. Cranial ultrasound, however, may not identify small subdural collections. High resolution ultrasound may be used to monitor lesions identified on CT or MRI.
Result
subdural fluid collection
skeletal survey
Test
Skeletal survey of hands, feet, long bones, skull, spine, and ribs (including oblique ribs) should be performed in children <2 years to detect occult fractures.[1] Multiple views of the axial and appendicular skeleton are required.
In cases of diagnosed abuse, a follow-up skeletal survey in 2 weeks is often performed to diagnose any fractures that may not have been identified on initial study. A complete repeat survey is usually appropriate, although a limited view follow-up could also be considered.[43]
Result
variable; unexplained fractures including skull fractures, long-bone fractures, rib fractures, and classic metaphyseal lesions
complementary imaging
Test
Complementary imaging may be indicated depending on the findings of the skeletal survey. These include CT/MRI for brain analysis and nuclear scintigraphy and/or extremity CT for a focal area of concern.[43]
Bone scintigraphy can be helpful in identifying rib and long-bone fractures, but it does not help identify the classic metaphyseal lesions.
Result
variable; unexplained fractures
blood culture
Test
Should be obtained as part of the routine workup of a febrile illness.
Result
bacteremia may be present
serum calcium
Test
Normal values are 9.0 to 10.8 mg/dL (2.25 to 2.70 mmol/L); as low as 7.6 mg/dL (1.90 mmol/L) in neonatal period.
It is important to exclude other underlying medical conditions that could cause the symptoms: for example, calcium may be decreased in hypocalcemic rickets.
Result
normal values for age
serum 1,25-dihydroxy vitamin D levels (calcidiol)
Test
Normal values are 16 to 65 picograms/mL (41.6 to 169.0 picomols/L); may be higher in preterm babies.
It is important to exclude other underlying medical conditions that could cause the symptoms: for example, vitamin D can be normal or increased in hypocalcemic rickets; they are usually normal or slightly increased in hypophosphatemic forms of rickets.
Result
normal values for age
serum inorganic phosphorus
Test
Normal values vary with age; neonatal period: 4.5 to 9.0 mg/dL (1.45 to 2.91 mmol/L); adolescence: 2.7 to 4.5 mg/dL (0.87 to 1.45 mmol/L).
It is important to exclude other underlying medical conditions that could cause the symptoms: for example, phosphate may be decreased in hypocalcemic and hypophosphatemic rickets.
Result
normal values for age
serum parathyroid hormone (PTH)
Test
Normal values vary with age and method.
It is important to exclude other underlying medical conditions that could cause the symptoms: for example, high serum PTH levels with hypocalcemic rickets and normal PTH levels with hypophosphatemic rickets.
Result
normal values for age
serum alkaline phosphatase
Test
High alkaline phosphatase may represent a high bone turnover state; may be elevated if skeletal fractures are present.
Alkaline phosphatase is also elevated in rickets and in osteogenesis imperfecta.
Result
elevated
skin biopsy/fibroblast culture
Test
If osteogenesis imperfecta is considered a possible differential diagnosis, skin biopsy or blood sample should be obtained, allowing testing for mutation of COL1A1 and COL1A2 genes. Additionally, a collagen synthesis assay may show quantitative or qualitative differences in collagen in patients with osteogenesis imperfecta.
Result
normal; abnormal collagen synthesis if osteogenesis imperfecta
postmortem exam
Test
Any unexplained infant death must have a postmortem exam to determine possible traumatic, infectious, or other medical causes before the diagnosis of sudden infant death syndrome is made.
A review of the medical records and investigation of the scene of death is also required.[54]
Result
subdural hemorrhage, brain edema, retinal or optic nerve sheath hemorrhage, unexplained fractures
Use of this content is subject to our disclaimer