Etiology
The most common bacterial pathogens in infective conjunctivitis include Pneumococcus, Staphylococcus aureus, Moraxella catarrhalis, and Haemophilus influenzae.[16][17][18][19]
Rarely, Neisseria gonorrhoeae causes a hyperacute purulent conjunctivitis; the organism is transmitted from the genitalia to the hands and then to the eyes.[20]Chlamydia is a common cause of persistent conjunctivitis.[1][16][21]
Viral conjunctivitis can be caused by adenovirus, herpes simplex, Epstein-Barr, varicella zoster, molluscum contagiosum, coxsackie, measles, mumps, rubella, zika, COVID-19, mpox, and enteroviruses.[1] Adenovirus is the most common cause, reported in 65% to 90% of viral conjunctivitis cases.[22][23] Adenoviral conjunctivitis usually causes epidemic keratoconjunctivitis, follicular conjunctivitis, and nonspecific conjunctivitis.[24][25] Viral conjunctivitis is highly contagious and spreads by direct contact with people or contaminated surfaces exposed to secretions.[19][26][27]
Contact lens wear may lead to a keratoconjunctivitis or giant cell papillary conjunctivitis secondary to infrequent lens replacement, prolonged wearing time, poor lens hygiene, allergenic contact lens solutions, ionic nature or high water content, or poor fit of contact lenses.[1]
Mechanical conjunctivitis can be caused by chronic conjunctival irritation, especially while sleeping. It is often caused by floppy eyelid syndrome, which is associated with obesity, sleep apnea, upper eyelid laxity, and lid imbrication (upper eyelid excursion over lower eyelid).
Toxic/chemical conjunctivitis results from irritation of the conjunctiva by environmental exposure to chemicals (including acids and bases). Some eye preparations (such as glaucoma medications, antibiotics, and antivirals) contain the preservative, benzalkonium chloride, that can accumulate in the conjunctiva after frequent administration, potentially resulting in toxic keratoconjunctivitis.[28]
Ocular cicatricial pemphigoid (a subtype of mucous membrane pemphigoid) may develop from a genetic predisposition or in response to certain topical medications such as idoxuridine, pilocarpine, epinephrine, timolol, and echothiophate.
Neoplastic conjunctivitis is caused by a sebaceous gland carcinoma; secondary radiation therapy may also induce a chronic conjunctivitis. Neoplastic conjunctivitis may also be caused by ocular surface squamous neoplasia, conjunctival lymphoma, and melanoma.[1][Figure caption and citation for the preceding image starts]: Bacterial conjunctivitisFrom the collection of Mr Hugh Harris; used with permission [Citation ends].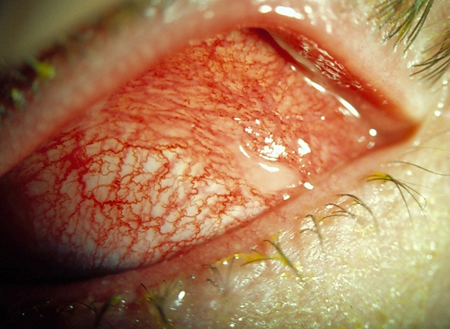
There are a number of rare causes of conjunctivitis, some of which have specific predisposing factors or associated features:[1][29][30][31][32][33][34][35]
Superior limbic keratoconjunctivitis (SLK): patient is typically a woman with chronic red and irritable eyes and abnormal thyroid function tests; condition may have been present for several years; dry eye and meibomian gland dysfunction, ocular graft-versus-host disease (GVHD), contact lens use
Blepharoconjunctivitis: there is chronic blepharitis with acute exacerbations of conjunctival injection; there may be an infective component, e.g., Staphylococcus, or Demodex (mites)
Keratoconjunctivitis sicca: dry eye syndrome
Rosacea conjunctivitis: rosacea may have ocular manifestations, including red eye and irritation
Giant fornix syndrome: a rare cause of conjunctivitis in older women (eighth to tenth decade) where there is an enlarged superior fornix and recurrent chronic purulent conjunctivitis
Pediculosis palpebrarum: infestation of lid margins by the crab louse (Phthirus pubis)
Conjunctival chalasis: there is loose or redundant conjunctival tissue, possibly after eye surgery; may lead to dry eye and meibomian gland dysfunction
Immune mediated: ocular cicatricial pemphigoid (a subtype of mucous membrane pemphigoid), graft versus host disease, Stevens-Johnson syndrome/toxic epidermal necrolysis (TEN), thyroid eye disease, and vasculitis are immune mediated causes of conjunctivitis
Ligneous conjunctivitis: a rare pseudomembranous disease of mucous membranes
Dupilumab-associated ocular surface disease: reported ocular adverse effects include conjunctivitis, dry eyes, and blepharitis
Parinaud oculoglandular syndrome: fever, regional lymphadenopathy, and follicular conjunctivitis; may occur in patients with Bartonella infection (cat scratch disease)
Mucus fishing syndrome: can be caused by mechanical trauma and associated disease causing irritation (e.g. dry eye, allergic conjunctivitis, or blepharitis).
Pathophysiology
The conjunctiva contains nonkeratinizing, squamous epithelium and a thin, richly vascularized substantia propria. The conjunctiva also has accessory lacrimal glands and goblet cells.
Allergic conjunctivitis is caused by a type I hypersensitivity reaction to an allergen. The allergen binds to a mast cell and crosslinking to IgE occurs, leading to mast cell degranulation and initiation of an inflammatory cascade.[7] Mediators released include histamine, tryptase, leukotrienes, and prostaglandins. The early phase of the allergic cascade lasts around 20 to 30 minutes, with mediators causing itching, increased vascular permeability, vasodilation, redness, and conjunctival injection. The late phase starts several hours later, with infiltration of inflammatory cells such as neutrophils, lymphocytes, basophils, and eosinophils.[36]
Infective conjunctivitis occurs as a result of reduced host defenses and external contamination.[37] Infectious pathogens can invade from adjacent sites or by a blood-borne pathway and replicate within the conjunctival mucosal cells. Both bacterial and viral infections initiate a leukocyte or lymphocytic inflammatory cascade leading to the attraction of red and white blood cells to the area. These white blood cells reach the conjunctival surface and accumulate there by easily moving through the dilated and highly permeable capillaries.
Classification
American Academy of Ophthalmology Preferred Practice Pattern[1]
Allergic conjunctivitis
Atopic keratoconjunctivitis
Seasonal/perennial allergic conjunctivitis
Vernal conjunctivitis
Bacterial conjunctivitis
Gonococcal (hyperacute) bacterial conjunctivitis
Nongonococcal bacterial conjunctivitis
Chlamydial conjunctivitis
Parinaud oculoglandular syndrome
Viral conjunctivitis
Adenoviral conjunctivitis
Herpetic conjunctivitis (herpes simplex virus and varicella zoster virus)
Molluscum contagiosum
Measles, mumps, and rubella (MMR)
Epstein-Barr virus
Zika
COVID-19
Mpox
Mechanical/irritative/toxic conjunctivitis
Superior limbic keratoconjunctivitis (SLK)
Blepharoconjunctivitis
Keratoconjunctivitis sicca (dry eye)
Rosacea conjunctivitis
Contact lens-related keratoconjunctivitis
Giant papillary conjunctivitis
Floppy eyelid syndrome
Giant fornix syndrome
Medication or preservative-induced ketaconjunctivitis
Conjunctival chalasis
Dupilumab-associated ocular surface disease
Immune-mediated conjunctivitis
Ocular mucous membrane pemphigoid (OMMP)
Graft-versus-host disease
Stevens-Johnson syndrome/toxic epidermal necrolysis (TEN)
Graves disease ophthalmopathy
Vasculitis
Neoplastic
Sebaceous carcinoma
Ocular surface squamous neoplasia
Melanoma
Conjunctival lymphoma
Other
Ligneous conjunctivitis
Pediculosis palpebrarum (Phthirus pubis)
Factitious conjunctivitis
Mucus fishing syndrome
Use of this content is subject to our disclaimer