Urgent considerations
See Differentials for more details
Acute coronary syndrome (ACS)
ACS refers to acute myocardial ischemia caused by atherosclerotic coronary disease and includes ST elevation MI (STEMI), non-ST elevation MI (NSTEMI), and unstable angina. Evaluation includes ECG and cardiac enzymes.
ACS presents with substernal chest pain that radiates to the left arm, neck, or jaw. There can be associated nausea and vomiting. Patients with STEMI need to be urgently triaged as they may suffer from life-threatening arrhythmias, cardiogenic shock, or pulmonary edema. Anticoagulation and acute reperfusion therapy with angioplasty or thrombolytics (if no contraindications and angioplasty not available) should be considered based on guideline recommendations.[25][26][27]
Aortic dissection
Suggested by sudden onset severe, sharp, or tearing posterior chest or back pain or anterior chest pain. Asymmetric pulses and discordant blood pressure (BP) on exam of both upper extremities should be sought as an examination clue. A widened mediastinum on chest x-ray is suggestive and the definitive diagnosis is made by transesophageal echocardiography, magnetic resonance imaging (MRI), or dynamic contrast computed tomography (CT) scan. Patients should be admitted to the intensive care unit for monitoring and aggressive reduction in BP. Surgical management is indicated for dissections involving the ascending aorta.[28]
Pneumothorax
Stable patients with spontaneous primary pneumothorax may be managed conservatively if asymptomatic or minimally symptomatic.[18] For patients needing intervention an ambulatory device may be an option, otherwise consider either needle aspiration or chest tube drainage, taking into account individual patient factors (including patient preference) and clinician experience.[18][29]
Hypoxemia and hypotension with deviation of trachea to the opposite side are indicative of tension pneumothorax and require urgent decompression with needle thoracostomy, followed by chest drain insertion.[Figure caption and citation for the preceding image starts]: Large left pneumothorax with visible pleural line and absence of lung markings beyond the lineFrom the collection of Dr Ami Rubinowitz; used with permission [Citation ends].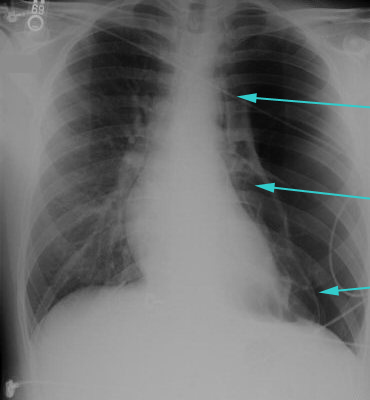
How to decompress a tension pneumothorax. Demonstrates insertion of a large-bore intravenous catheter into the fourth intercostal space in an adult.
How to insert an intercostal (chest) drain using the open technique. Video demonstrates: tube selection, how to identify the site for drain insertion, how to make the correct incision, how to insert the intercostal drain, how to secure the drain, and postprocedure care.
How to insert an intercostal (chest) drain using the Seldinger technique. Video demonstrates: how to identify a safe site for insertion; use of an introducer needle, guidewire, dilators, and intercostal drain; how to confirm drain position; and postprocedure care.
Pulmonary embolism
A potentially life-threatening condition that can cause sudden death from hypoxemia, shock, and hemodynamic compromise.
The clinical probability of pulmonary embolism (PE) in hemodynamically stable patients is assessed using a combination of the Pulmonary Embolism Rule-Out Criteria (the PERC rule), the Wells (or Geneva) score, plus D-dimer testing if indicated.[40][41][42][43][44] [ PERC Rule for the Assessment of Possible Pulmonary Embolism Opens in new window ] [ Pulmonary Embolism Wells Score Opens in new window ] [ Revised Geneva Score for Estimation of the Clinical Probability of Pulmonary Embolism in Adults Opens in new window ]
If there is a low clinical suspicion of PE, it can effectively be ruled out in any patient who meets the PERC rule.[43] If clinical suspicion of PE is high or the patient does not meet the PERC rule, the Wells or Geneva score can be used to categorize the patient as ''PE likely'' or ''PE unlikely''.[40][44]
In hemodynamically stable patients with low or intermediate clinical probability of PE, D-dimer measurement is recommended to assess the need for imaging. In patients with very low clinical probability of PE, D-dimer testing is reserved for those who do not meet the PERC rule.[43]
Those with a high clinical probability of PE, or with a positive D-dimer, should proceed immediately to computed tomographic pulmonary angiography (CTPA; or ventilation-perfusion [V/Q] lung scan if CTPA is contraindicated). In patients with high pretest probability of PE, anticoagulation should be initiated while awaiting imaging results.[44][45]
Hemodynamically unstable patients require urgent primary reperfusion, anticoagulation, and supportive care.[45] CTPA is indicated in patients with suspected PE who are hemodynamically unstable at presentation provided it is immediately available and the patient is well enough to have it. In practice this is often not the case and echocardiography is used instead.
Pneumonia/empyema
Pneumonia with associated complicated effusion or empyema needs to be drained urgently as it can be a source of persistent infection and can eventually undergo fibrinous organization forming loculated effusion or trapped lung syndrome. Methods to drain the empyema include chest tube insertion, or surgical options such as video-assisted thoracoscopic surgery or open decortication.
Other causes of pleuritic chest pain
Though not causes of pleuritis per se, conditions such as pericarditis or perforated viscus should be considered in the differential diagnosis when patients present with chest pain that is pleuritic in nature.
Use of this content is subject to our disclaimer


