Vitamin D deficiency is frequently underdiagnosed in children and adults, primarily because patients do not typically present with overt clinical signs and symptoms until the deficiency is severe and prolonged. In growing children, vitamin D deficiency will reduce bone mineral deposition (resulting in the skeletal manifestations of rickets), developmental delay, and faltering growth.[78]Uday S, Högler W. Nutritional rickets & osteomalacia: A practical approach to management. Indian J Med Res. 2020 Oct;152(4):356-67.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8061584
http://www.ncbi.nlm.nih.gov/pubmed/33380700?tool=bestpractice.com
In adults, vitamin D deficiency causes a defect in mineralization of the collagen matrix such that they present with signs and symptoms of osteomalacia (bone pain and tenderness, proximal muscle weakness reported as difficulty rising from a sitting position).[2]Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Jul;96(7):1911-30.
https://academic.oup.com/jcem/article/96/7/1911/2833671
http://www.ncbi.nlm.nih.gov/pubmed/21646368?tool=bestpractice.com
[78]Uday S, Högler W. Nutritional rickets & osteomalacia: A practical approach to management. Indian J Med Res. 2020 Oct;152(4):356-67.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8061584
http://www.ncbi.nlm.nih.gov/pubmed/33380700?tool=bestpractice.com
The hallmark for diagnosing vitamin D deficiency is the measurement of serum 25-hydroxyvitamin D.[1]Hossein-Nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc. 2013 Jul;88(7):720-55.
http://www.mayoclinicproceedings.org/article/S0025-6196(13)00404-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23790560?tool=bestpractice.com
[2]Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Jul;96(7):1911-30.
https://academic.oup.com/jcem/article/96/7/1911/2833671
http://www.ncbi.nlm.nih.gov/pubmed/21646368?tool=bestpractice.com
Although several inherited or acquired disorders of vitamin D metabolism do not result in a serum 25-hydroxyvitamin D level of <20 nanograms/mL, they are still considered causes of vitamin D deficiency and usually present in the same manner, often with more severe skeletal deformities and metabolic bone disease.[1]Hossein-Nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc. 2013 Jul;88(7):720-55.
http://www.mayoclinicproceedings.org/article/S0025-6196(13)00404-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23790560?tool=bestpractice.com
[5]Chanchlani R, Nemer P, Sinha R, et al. An overview of rickets in children. Kidney Int Rep. 2020 Jul;5(7):980-90.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7335963
http://www.ncbi.nlm.nih.gov/pubmed/32647755?tool=bestpractice.com
History
The presence of risk factors should be sought when taking a history. People most at risk of vitamin D deficiency include neonates who receive breast milk as their sole nutrition with no vitamin D supplementation; children and adults with black skin; and patients with malabsorption syndromes (celiac disease, cystic fibrosis, short bowel syndrome, inflammatory bowel disease, Whipple disease), including those who have undergone gastric bypass surgery.[2]Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Jul;96(7):1911-30.
https://academic.oup.com/jcem/article/96/7/1911/2833671
http://www.ncbi.nlm.nih.gov/pubmed/21646368?tool=bestpractice.com
In addition, children and adults who are institutionalized, exposed to minimal sunlight, always wear sun protection before going outdoors, or live in cold climates (vitamin D deficiency is most common in the winter months, when little if any cutaneous vitamin D production occurs from sun exposure) are at risk.[1]Hossein-Nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc. 2013 Jul;88(7):720-55.
http://www.mayoclinicproceedings.org/article/S0025-6196(13)00404-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23790560?tool=bestpractice.com
[21]Charoenngam N, Holick MF. Immunologic effects of vitamin D on human health and disease. Nutrients. 2020 Jul 15;12(7):2097.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7400911
http://www.ncbi.nlm.nih.gov/pubmed/32679784?tool=bestpractice.com
[58]Wacker M, Holick MF. Sunlight and vitamin D: a global perspective for health. Dermatoendocrinol. 2013 Jan 1;5(1):51-108.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3897598
http://www.ncbi.nlm.nih.gov/pubmed/24494042?tool=bestpractice.com
Furthermore, adults >50 years of age have reduced synthetic capacity to make vitamin D in their skin and, therefore, are also at higher risk.[58]Wacker M, Holick MF. Sunlight and vitamin D: a global perspective for health. Dermatoendocrinol. 2013 Jan 1;5(1):51-108.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3897598
http://www.ncbi.nlm.nih.gov/pubmed/24494042?tool=bestpractice.com
Children who do not receive at least 600 IU of vitamin D a day from diet and supplements, and adults who do not receive at least 1000 to 2000 IU of vitamin D a day from diet and supplements, are likely to be vitamin D-deficient or -insufficient.[2]Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Jul;96(7):1911-30.
https://academic.oup.com/jcem/article/96/7/1911/2833671
http://www.ncbi.nlm.nih.gov/pubmed/21646368?tool=bestpractice.com
Obese children and adults (BMI >30), and those with cystic fibrosis, require 2 to 3 times more vitamin D than the general population to satisfy their vitamin D requirement, and so also fall into the high-risk category.[1]Hossein-Nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc. 2013 Jul;88(7):720-55.
http://www.mayoclinicproceedings.org/article/S0025-6196(13)00404-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23790560?tool=bestpractice.com
[66]Wortsman J, Matsuoka LY, Chen TC, et al. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000 Sep;72(3):690-3. [Erratum in: Am J Clin Nutr. 2003 May;77(5):1342.]
http://ajcn.nutrition.org/content/72/3/690.full
http://www.ncbi.nlm.nih.gov/pubmed/10966885?tool=bestpractice.com
Medication history is important because patients taking glucocorticoids, antiepileptic medication, highly active antiretroviral therapy, rifampin, or St John's wort are also prone to developing vitamin D deficiency.[68]Gröber U, Kisters K. Influence of drugs on vitamin D and calcium metabolism. Dermatoendocrinol. 2012 Apr 1;4(2):158-66.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3427195
http://www.ncbi.nlm.nih.gov/pubmed/22928072?tool=bestpractice.com
History of liver and chronic kidney disease should be excluded.
In mild or early disease, patients may be completely asymptomatic. Faltering growth and delayed achievement of motor milestones are common childhood presentations of rickets. In adults with severe or prolonged vitamin D deficiency, symptoms of osteomalacia typically include throbbing, aching bone discomfort that can be localized or generalized.[78]Uday S, Högler W. Nutritional rickets & osteomalacia: A practical approach to management. Indian J Med Res. 2020 Oct;152(4):356-67.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8061584
http://www.ncbi.nlm.nih.gov/pubmed/33380700?tool=bestpractice.com
In addition, easy fatigability and malaise are common symptoms. Patients may also report difficulty rising from a sitting position (due to proximal muscle weakness), and a waddling gait.[2]Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Jul;96(7):1911-30.
https://academic.oup.com/jcem/article/96/7/1911/2833671
http://www.ncbi.nlm.nih.gov/pubmed/21646368?tool=bestpractice.com
Patients with oncogenic osteomalacia usually present with nonspecific symptoms of muscle weakness and aching bone pain.[4]Jan de Beur SM, Minisola S, Xia WB, et al. Global guidance for the recognition, diagnosis, and management of tumor-induced osteomalacia. J Intern Med. 2023 Mar;293(3):309-28.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10108006
http://www.ncbi.nlm.nih.gov/pubmed/36511653?tool=bestpractice.com
Physical exam
Children
Rickets occurs as a consequence of poor global mineralization of the skeleton, and is characterized by delayed growth, bone pain, and bone deformity.[5]Chanchlani R, Nemer P, Sinha R, et al. An overview of rickets in children. Kidney Int Rep. 2020 Jul;5(7):980-90.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7335963
http://www.ncbi.nlm.nih.gov/pubmed/32647755?tool=bestpractice.com
These abnormalities usually manifest between 6 months and 2 years of age. Type of deformity depends on the biomechanical situation of the extremities at the time when the structural weakness develops. Bone deformities of the forearms and posterior bowing of the distal tibia can occur in infants (due to muscle tension), whereas exaggerated physiologic bowing of the legs (genu varum) is a finding in toddlers who have started walking (due to gravity pushing on the lower limbs). Older children may have valgus or windswept (valgus deformity of one leg and varus deformity of the other) deformities of the legs. Other bony deformities that may occur include knob-like projections along the ribcage (rachitic rosary), frontal bossing, and widening of the ends of the long bones, especially the wrists. Muscle traction on the softened ribcage is responsible for chest deformation leading to pectus carinatum, thoracic asymmetry, and a widening of the thoracic base. Tooth development is impaired, with delayed eruption and early dental caries. Head sweating may be evident due to increased neuromuscular activity. Infants or young children may seem irritable as a result of associated bone pain. Features of hypocalcemia may be present as a result of inherited disorders of vitamin D metabolism or chronic untreated vitamin D deficiency. These include muscle cramps, muscle weakness, carpal pedal spasm, numbness, paresthesias, tetany, and seizures.[78]Uday S, Högler W. Nutritional rickets & osteomalacia: A practical approach to management. Indian J Med Res. 2020 Oct;152(4):356-67.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8061584
http://www.ncbi.nlm.nih.gov/pubmed/33380700?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Inward or outward bowing of the legs is a typical sign of classic ricketsCDC [Citation ends].
Adults
In adults with vitamin D deficiency, the growth plates are closed and there is enough mineral in the skeleton to prevent the gross skeletal deformities that are seen in children. Physical exam may reveal localized or generalized bony tenderness. Pressing with thumb or forefinger on the sternum, radius, and anterior tibia and eliciting wincing bone pain is a classic sign of periosteal bone discomfort associated with osteomalacia.[1]Hossein-Nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc. 2013 Jul;88(7):720-55.
http://www.mayoclinicproceedings.org/article/S0025-6196(13)00404-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23790560?tool=bestpractice.com
Pain in the hips may result in a waddling gait, and proximal muscle weakness is often seen; this is diagnosed by watching the patient get up from a sitting position with difficulty.
Laboratory investigations
The diagnosis of vitamin D deficiency or insufficiency in both adults and children is made by determining the patient's level of serum 25-hydroxyvitamin D.[1]Hossein-Nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc. 2013 Jul;88(7):720-55.
http://www.mayoclinicproceedings.org/article/S0025-6196(13)00404-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23790560?tool=bestpractice.com
[2]Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Jul;96(7):1911-30.
https://academic.oup.com/jcem/article/96/7/1911/2833671
http://www.ncbi.nlm.nih.gov/pubmed/21646368?tool=bestpractice.com
[74]Institute of Medicine. Dietary reference intakes for calcium and vitamin D. 2011 [internet publication].
https://www.nap.edu/catalog/13050/dietary-reference-intakes-for-calcium-and-vitamin-d
In addition, measuring plasma concentrations of calcium, phosphorus (fasting), and intact parathyroid hormone (PTH) and alkaline phosphatase may aid diagnosis and help determine the underlying cause. Serum 25-hydroxyvitamin D should not be used as a screening test in otherwise healthy populations.[2]Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Jul;96(7):1911-30.
https://academic.oup.com/jcem/article/96/7/1911/2833671
http://www.ncbi.nlm.nih.gov/pubmed/21646368?tool=bestpractice.com
[79]Munns CF, Shaw N, Kiely M, et al. Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endocrinol Metab. 2016 Feb;101(2):394-415.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4880117
http://www.ncbi.nlm.nih.gov/pubmed/26745253?tool=bestpractice.com
[80]American Society for Clinical Pathology. Thirty five things physicians and patients should question. Choosing Wisely, an initiative of the ABIM Foundation. 2021 [internet publication].
https://web.archive.org/web/20230316185857/https://www.choosingwisely.org/societies/american-society-for-clinical-pathology
[81]American Academy of Pediatrics – Section on Endocrinology. Five things physicians and patients should question. Choosing Wisely, an initiative of the ABIM Foundation. 2022 [internet publication].
https://web.archive.org/web/20230326144421/https://www.choosingwisely.org/societies/american-academy-of-pediatrics-section-on-endocrinology
A 25-hydroxyvitamin D level of ≤20 nanograms/mL is considered vitamin D-deficient and is associated with a normal serum calcium, low-normal serum phosphorus, and a high-normal or elevated intact PTH level.[2]Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Jul;96(7):1911-30.
https://academic.oup.com/jcem/article/96/7/1911/2833671
http://www.ncbi.nlm.nih.gov/pubmed/21646368?tool=bestpractice.com
[74]Institute of Medicine. Dietary reference intakes for calcium and vitamin D. 2011 [internet publication].
https://www.nap.edu/catalog/13050/dietary-reference-intakes-for-calcium-and-vitamin-d
A 25-hydroxyvitamin D level between 21 and 29 nanograms/mL is considered vitamin D-insufficient.[2]Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Jul;96(7):1911-30.
https://academic.oup.com/jcem/article/96/7/1911/2833671
http://www.ncbi.nlm.nih.gov/pubmed/21646368?tool=bestpractice.com
These patients have a normal level of serum calcium and phosphorus and usually a normal or slightly elevated intact PTH.
Measuring the serum level of 1,25-dihydroxyvitamin D is of no value in determining vitamin D status because it circulates at a concentration 1000 times lower than 25-hydroxyvitamin D, has a half-life of only 4 hours (compared with the 2 to 3 weeks for 25-hydroxyvitamin D), and secondary hyperparathyroidism enhances its production. Many physicians who obtain a serum 1,25-dihydroxyvitamin D level find it normal and conclude that the patient cannot be vitamin D-deficient. However, this measurement is of great value in distinguishing the inherited or acquired disorders of vitamin D metabolism.[2]Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Jul;96(7):1911-30.
https://academic.oup.com/jcem/article/96/7/1911/2833671
http://www.ncbi.nlm.nih.gov/pubmed/21646368?tool=bestpractice.com
[82]Endocrine Society. Five things physicians and patients should question. Choosing Wisely, an initiative of the ABIM Foundation. 2022 [internet publication].
https://web.archive.org/web/20221207180203/https://www.choosingwisely.org/societies/endocrine-society
Children
A serum 25-hydroxyvitamin D level of <15 nanograms/mL is usually associated with skeletal manifestations of vitamin D-deficiency rickets. The serum calcium can be normal or low, and the serum phosphorus is usually low-normal or low. The serum alkaline phosphatase and intact PTH levels are usually elevated. A child with pseudovitamin D-deficiency rickets usually has a normal 25-hydroxyvitamin D level with hypocalcemia, hypophosphatemia, elevated alkaline phosphatase, and intact PTH levels with a low or undetectable level of 1,25-dihydroxyvitamin D. A child with vitamin D-resistant rickets has all the biochemical manifestations of pseudovitamin D-resistant rickets with the exception that the serum 1,25-dihydroxyvitamin D is markedly elevated. Children with X-linked hypophosphatemic rickets and autosomal-dominant hypophosphatemic rickets have a normal serum 25-hydroxyvitamin D and calcium, a low level of serum phosphorus, and an inappropriately low or low-normal level of 1,25-dihydroxyvitamin D.[1]Hossein-Nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc. 2013 Jul;88(7):720-55.
http://www.mayoclinicproceedings.org/article/S0025-6196(13)00404-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23790560?tool=bestpractice.com
[5]Chanchlani R, Nemer P, Sinha R, et al. An overview of rickets in children. Kidney Int Rep. 2020 Jul;5(7):980-90.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7335963
http://www.ncbi.nlm.nih.gov/pubmed/32647755?tool=bestpractice.com
Adults
For adults, there are no overt skeletal deformities because the growth plates are closed. Instead, vitamin D deficiency causes secondary hyperparathyroidism, with a normal or mildly elevated alkaline phosphatase, normal calcium, and low or low-normal fasting phosphorus. The hallmark of oncogenic osteomalacia is a low serum phosphorus level (usually 1.2 to 1.6 micrograms/dL) and an inappropriately low-normal or low level of serum 1,25-dihydroxyvitamin D.[4]Jan de Beur SM, Minisola S, Xia WB, et al. Global guidance for the recognition, diagnosis, and management of tumor-induced osteomalacia. J Intern Med. 2023 Mar;293(3):309-28.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10108006
http://www.ncbi.nlm.nih.gov/pubmed/36511653?tool=bestpractice.com
Serum calcium and intact PTH levels are usually normal, whereas 25-hydroxyvitamin D level is low or normal.
Imaging
In asymptomatic patients, plain film radiographs are usually unnecessary, but x-rays of the knees and wrists should be performed when rickets or osteomalacia is suspected.[78]Uday S, Högler W. Nutritional rickets & osteomalacia: A practical approach to management. Indian J Med Res. 2020 Oct;152(4):356-67.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8061584
http://www.ncbi.nlm.nih.gov/pubmed/33380700?tool=bestpractice.com
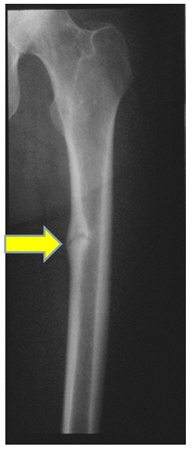
Widening of the epiphyseal plate, and loss of definition of the zone of provisional calcification at the epiphyseal/metaphyseal interface, are early signs of rickets. Looser pseudofractures, which lie perpendicular to the cortical margins with the characteristic sclerotic borders, are a pathognomonic finding in osteomalacia.[83]Modest JM, Sheth H, Gohh R, et al. Osteomalacia and renal osteodystrophy. R I Med J (2013). 2022 Oct 3;105(8):22-7.
http://rimed.org/rimedicaljournal/2022/10/2022-10-22-fractures-modest.pdf
http://www.ncbi.nlm.nih.gov/pubmed/36173905?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: X-rays of a wrist from a child with vitamin D-deficiency rickets before (left panel) and after (right panel) treatment with vitamin DFrom the collection of M.F. Holick, PhD, MD; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Radiograph of the femoral shaft in a patient with osteomalacia demonstrating a "pseudofracture" (also known as Looser's zone) on the medial aspect of the mid-femoral shaftFrom the collection of Bridget Sinnott, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Radiograph of the femoral shaft in a patient with osteomalacia demonstrating a "pseudofracture" (also known as Looser's zone) on the medial aspect of the mid-femoral shaftFrom the collection of Bridget Sinnott, MD [Citation ends].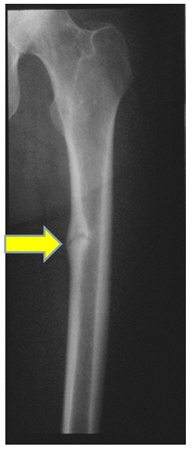
Adults with chronic vitamin D deficiency may have low bone density leading to osteopenia and osteoporosis. A dual-energy x-ray absorptiometry (DEXA) scan should therefore be performed to assess bone density; it also aids in tracking disease progression.

 [Figure caption and citation for the preceding image starts]: Radiograph of the femoral shaft in a patient with osteomalacia demonstrating a "pseudofracture" (also known as Looser's zone) on the medial aspect of the mid-femoral shaftFrom the collection of Bridget Sinnott, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Radiograph of the femoral shaft in a patient with osteomalacia demonstrating a "pseudofracture" (also known as Looser's zone) on the medial aspect of the mid-femoral shaftFrom the collection of Bridget Sinnott, MD [Citation ends].