Approach
Liver abscess is an uncommon disease. The historical features and signs are often nonspecific. Therefore, it is important to have a low threshold for consideration of liver abscess as a possible cause for the presenting complaint. Imaging of the liver and cultures of the abscess fluid are key to making the diagnosis and identifying the causative organism(s).
History
Underlying biliary tract abnormalities, ages >50 years, malignancy, diabetes mellitus, poor dentition, and interventional biliary or hepatic procedures are strongly associated risk factors for the development of pyogenic liver abscess. Patients who are from or have visited endemic areas for amebiasis are at increased risk of amebic liver abscess.[2]
The most common symptoms at presentation of pyogenic abscess are fever, chills, fatigue, nausea, vomiting, and abdominal pain. If the diaphragm is inflamed because of adjacent infection, then cough, shortness of breath, and pleuritic pain may also be present. Pain may be referred to the right shoulder tip in these cases. Patients with fungal liver abscess present with similar symptoms. Patients are typically immunocompromised or neutropenic.[19] Symptoms typically occur when the immune system recovers (when the neutrophil count begins to increase).
Generally, symptoms occur in an insidious manner, can be nonspecific, and are of variable duration. Symptoms of amebic abscess are similar to those of pyogenic abscess but are more likely to be associated with an acute onset.[19] Other symptoms of amebiasis, such as diarrhea, may coexist. Patients with particularly severe infection (of any type) may also develop symptoms more rapidly.
Physical exam
Fever, right upper quadrant tenderness, and hepatomegaly are usually found on physical exam. However, the absence of these findings does not exclude the diagnosis of liver abscess. Only a few patients with liver abscess have jaundice, which typically occurs late in the illness. Occasionally, pleural effusion may develop, resulting in the typical chest exam findings of dullness to percussion, absent breath sounds, decreased tactile fremitus, and decreased vocal transmission in the right lower zone. Rarely, ascites may be present. Patients with severe illness, often with bacteremia or cholangitis, may present with signs of shock.
Laboratory exam
Patients with suspected liver abscess should have basic laboratory studies, including:
Complete blood count
Serum albumin, aminotransferase, bilirubin, and alkaline phosphatase levels
Prothrombin time (PT) and activated partial thromboplastin time (aPTT)
Blood cultures.
Anemia and leukocytosis with an elevated neutrophil count are common. Liver biochemical tests, especially the alkaline phosphatase, are abnormal in most patients. The serum albumin is often low. Although these findings suggest liver disease, they are nonspecific. PT and aPTT are done to check that blood clotting is within normal limits before aspiration is performed. Blood cultures can identify the causative organism in approximately one half of patients and should be obtained if liver abscess is suspected. Blood cultures should be obtained prior to the administration of antibiotics.
If amebic abscess is suspected, serology may be diagnostic. Where there is coexistent diarrhea, the Entamoeba histolytica enzyme immunoassay can detect the antigen of Entamoeba histolytica in a stool specimen.
C-reactive protein is a nonspecific test that can be used to monitor the inflammatory response and therefore response to treatment.[27]
How to take a venous blood sample from the antecubital fossa using a vacuum needle.
Imaging tests
The preferred initial imaging tests are contrast-enhanced abdominal computed tomography (CT) scan and abdominal ultrasound.[29][30] Magnetic resonance imaging (MRI) is more sensitive than ultrasonography and CT for small abscesses but is expensive and more limited in availability. The sensitivity of CT for liver abscess is higher than that for ultrasound (97% vs 85%).[31][32] In the US, CT scan is usually performed, as it is usually readily available. Occasionally, both ultrasound scan and CT scan are performed: for example, if an initial ultrasound was inadequate or was negative despite a strong suspicion for a diagnosis of liver abscess. Either ultrasound or CT can be used to guide aspiration of the suspected collection. The advantages of ultrasound are wide availability, low cost, and lack of need for a contrast agent. CT allows detailed exam of organs adjacent to the liver and has a higher sensitivity. Avoid the use of noncontrast enhanced CT imaging alongside contrast enhanced imaging; the addition of unenhanced CT does not provide additional diagnostic information and exposes patients to unnecessary radiation.[33] An abscess typically is demonstrated on ultrasound or CT scan as a right-sided (most frequently) fluid collection with surrounding edema.[Figure caption and citation for the preceding image starts]: CT scan showing a liver abscess (7 cm x 5 cm) in a 46-year-old man who presented with fever, fatigue, and coughFrom the collection of Massachusetts General Hospital radiology images [Citation ends]. [Figure caption and citation for the preceding image starts]: CT scan (coronal view) showing liver abscess in a 46-year-old man who presented with fever, fatigue, and coughFrom the collection of Massachusetts General Hospital radiology images [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan (coronal view) showing liver abscess in a 46-year-old man who presented with fever, fatigue, and coughFrom the collection of Massachusetts General Hospital radiology images [Citation ends].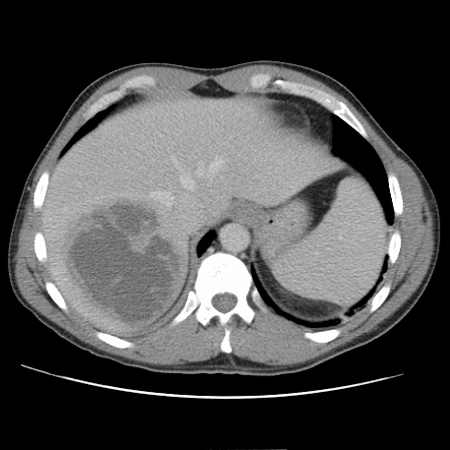
MRI with contrast may also be useful in the diagnosis of liver abscess, and can help differentiate from other causes of liver mass e.g., malignancy.[34] However, MRI is an expensive test, requires administration of gadolinium contrast, and may be limited in availability.
Before aspiration, it is important to check that all clotting parameters are within normal limits. Aspiration of the abscess fluid confirms the diagnosis of abscess and directs antibiotic therapy. However, culture of a sample from an existing drain is not helpful to guide antimicrobial therapy.[35] The fluid should be sent for Gram stain and for aerobic and anaerobic cultures.
Aspiration of the lesion confirms the diagnosis of amebic abscess, but it may not be necessary. The aspirate is typically a red-brown viscous fluid ("anchovy paste" or "chocolate sauce").[19] Antigen detection in the liver abscess fluid or polymerase chain reaction (typically performed at a reference laboratory) on liver abscess pus is definitive for diagnosis of amebic liver abscess.[Figure caption and citation for the preceding image starts]: Gross pathology of amebic abscess of liver; tube of "chocolate" pus from abscessCDC/Dr. Mae Melvin; Dr. E. West of Mobile, AL [Citation ends].
Aspiration/sampling should be avoided if there is evidence of abnormal coagulation. It is also contraindicated if a hydatid cyst is suspected, because of the low but real risk of anaphylaxis. However, aspiration may occasionally be performed in patients with possible hydatid disease when the diagnosis of amebic liver abscess remains a possibility, or when the aspiration is performed as part of the therapy. Aspiration should be undertaken only by physicians experienced in performing these procedures and in centers specialized in treating these patients.
A chest x-ray is also indicated if there are any chest symptoms or signs on exam (e.g., symptoms suggestive of diaphragmatic irritation or signs of pleural effusion).[19]
Use of this content is subject to our disclaimer
