Tests
1st tests to order
immunoglobulin A-tissue transglutaminase (IgA-tTG)
Test
Order an IgA-tTG test as the initial test in any patient with suspected celiac disease.[34][68][70][71][72]
Higher titers have increased positive predictive value. Serologic testing should be done on a gluten-containing diet.[110][111]
Result
titer above normal range for laboratory; however, a normal titer does not exclude celiac disease, as seronegative celiac disease occurs in a minority of patients
quantitative IgA
IgG DGP (deamidated gliadin peptide)
CBC
Test
Iron deficiency anemia is a common clinical presentation in adults.
Folate (and rarely vitamin B12) deficiency may lead to macrocytic anemia.[88]
Result
low Hb and microcytic hypochromic red cells
endomysial antibody (EMA)
Test
EMA is an alternative to IgA-tTG with greater specificity but lower sensitivity.
Perform initially if IgA-tTG is unavailable.[74]
Result
elevated titer
skin biopsy
Test
Order this test initially in any patient with skin lesions suggestive of dermatitis herpetiformis.
Both sensitivity and specificity are high, if normal-appearing skin adjacent to a lesion is biopsied.
Result
granular deposits of IgA at the dermal papillae of lesional and perilesional skin by direct immunofluorescence
small bowel endoscopy
Test
The endoscopic appearance is not sensitive for diagnosis and may be normal in up to one third of cases at diagnosis.[113][Figure caption and citation for the preceding image starts]: Scalloping of the duodenal mucosa in a patient with celiac diseaseFrom the personal collection of DA Leffler; used with permission [Citation ends].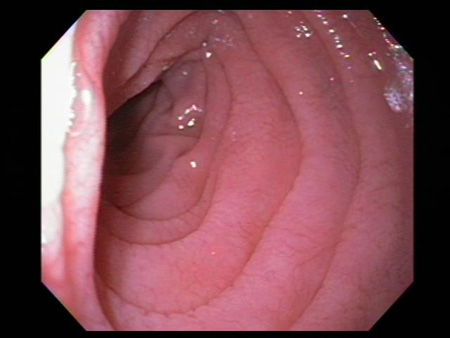 [Figure caption and citation for the preceding image starts]: Scalloping of the duodenal mucosa in a patient with celiac diseaseFrom the personal collection of DA Leffler; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Scalloping of the duodenal mucosa in a patient with celiac diseaseFrom the personal collection of DA Leffler; used with permission [Citation ends].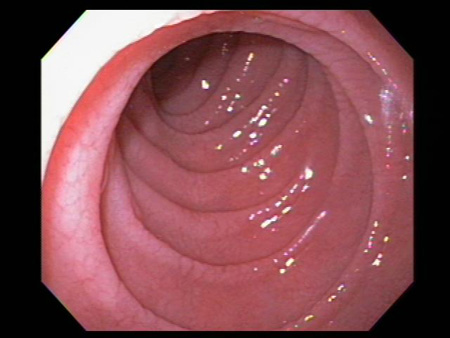
Result
atrophy and scalloping of mucosal folds; nodularity and mosaic pattern of mucosa
small bowel histology
Test
Small bowel histology is essential and the gold-standard test to confirm the diagnosis.
Biopsies should be performed while on a gluten-containing diet. Patients with an elevated IgA-tTG level should be referred for duodenal biopsy. Small intestinal biopsies should be obtained regardless of the IgA-tTG result in patients with a high clinical index of suspicion.[77]
Two biopsies of the duodenal bulb and at least four biopsies of the distal duodenum should be submitted for histologic analysis.
A single biopsy specimen should be collected with each pass of the forceps, to improve the diagnostic quality of the specimens.[34]
Biopsy results are commonly graded using the Marsh criteria.
Result
presence of intraepithelial lymphocytes, villous atrophy, and crypt hyperplasia
Tests to consider
human leukocyte antigen (HLA) typing
Test
May be used to rule out celiac disease in patients already on a gluten-free diet or in patients with an idiopathic celiac-like enteropathy but is only helpful for diagnosis in select cases, such as when there is discrepancy between serologic and histologic findings.[70]
Result
positive HLA-DQ2 or HLA-DQ8
gluten challenge
Test
People with celiac disease on a gluten-free diet prior to evaluation cannot be differentiated from healthy controls. In these patients, gluten challenge is necessary. In a gluten challenge, the person is placed back on a gluten-containing diet (at least two slices of wheat bread daily), and serologic tests and small bowel histology assessed after 2-8 weeks on the gluten-containing diet.[82][83]
Result
increase in celiac serologic tests and presence of intraepithelial lymphocytes, villous atrophy, and crypt hyperplasia on small intestinal biopsy
video capsule endoscopy
Test
Video capsule endoscopy enables imaging of the entire small intestine and has good sensitivity for the detection of macroscopic features of celiac disease. In 3% of cases, villous atrophy is only found in the jejunum, reducing the yield of upper endoscopy and duodenal biopsies for diagnosis.[114]
Capsule endoscopy is, however, typically used to detect complications of celiac disease, such as ulcerative jejunitis or lymphoma.[80][81]
Video capsule endoscopy is not recommended when a stricture is suspected.
Result
atrophy and scalloping of mucosal folds; nodularity and mosaic pattern of mucosa; sensitive for the detection of villous atrophy
immunoglobulin G-tissue transglutaminase (IgG-tTG)
Test
IgG-tTG serology should not be used as initial investigation ahead of IgA-tTG and quantitative IgA assessment.[34][70][71][72]
DGP serology has largely replaced IgG-tTG serology for IgA-deficient patients.
In children ages <2 years who do not have IgA deficiency, IgA-TTG is the preferred test to confirm celiac disease diagnosis, whereas in those with IgA deficiency, IgG-DGP or IgG-tTG can be used as confirmatory tests.[70][78]
Result
elevated titer
Use of this content is subject to our disclaimer