Characteristic history and examination findings are usually sufficient to diagnose miliaria.
History and symptoms
Miliaria crystallina is characterised by asymptomatic fragile vesicles that appear in crops days to weeks after exposure to an inciting factor.[1]Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998 Jan;38(1):1-17; quiz 18-20.
http://www.ncbi.nlm.nih.gov/pubmed/9448199?tool=bestpractice.com
Important factors that can induce miliaria crystallina include the following:[1]Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998 Jan;38(1):1-17; quiz 18-20.
http://www.ncbi.nlm.nih.gov/pubmed/9448199?tool=bestpractice.com
[3]Arpey CJ, Nagashima-Whalen LS, Chren MM, et al. Congenital miliaria crystallina: case report and literature review. Pediatr Dermatol. 1992 Sep;9(3):283-7.
http://www.ncbi.nlm.nih.gov/pubmed/1488382?tool=bestpractice.com
[10]Haas N, Martens F, Henz BM. Miliaria crystallina in an intensive care setting. Clin Exp Dermatol. 2004 Jan;29(1):32-4.
http://www.ncbi.nlm.nih.gov/pubmed/14723716?tool=bestpractice.com
[16]Shuster S. Duct disruption, a new explanation of miliaria. Acta Derm Venereol. 1997 Jan;77(1):1-3.
http://www.ncbi.nlm.nih.gov/pubmed/9059666?tool=bestpractice.com
[22]Rochmis PG, Koplon BS. Iatrogenic miliaria crystallina due to bethanechol. Arch Dermatol. 1967 May;95(5):499-500.
http://www.ncbi.nlm.nih.gov/pubmed/6023703?tool=bestpractice.com
[23]Gupta AK, Ellis CN, Madison KC, et al. Miliaria crystallina occurring in a patient treated with isotretinoin. Cutis. 1986 Oct;38(4):275-6.
http://www.ncbi.nlm.nih.gov/pubmed/3465509?tool=bestpractice.com
[24]Godkar D, Razaq M, Fernandez G. Rare skin disorder complicating doxorubicin therapy: miliaria crystallina. Am J Ther. 2005 May-Jun;12(3):275-6.
http://www.ncbi.nlm.nih.gov/pubmed/15891274?tool=bestpractice.com
Exposure to excessive heat and humidity, especially in tropical areas or during summer months in temperate areas
Use of occlusive clothing
Febrile illness
Following sunburn under hot and humid climatic conditions
Medicines such as isotretinoin, doxorubicin, or betacholine
Following staphylococcal scalded skin syndrome
Heavily bundled infants
In newborns immediately after delivery in the setting of maternal fever.
Miliaria rubra is characterised by an eruption of papules accompanied by a sensation of pruritus, prickling, burning, or tingling that is paroxysmal and exacerbated by stimuli that induce sweating.[1]Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998 Jan;38(1):1-17; quiz 18-20.
http://www.ncbi.nlm.nih.gov/pubmed/9448199?tool=bestpractice.com
[2]Sulzberger MB, Harris DR. Miliaria and anhidrosis. 3. Multiple small patches and the effects of different periods of occlusion. Arch Dermatol. 1972 Jun;105(6):845-50.
http://www.ncbi.nlm.nih.gov/pubmed/5030233?tool=bestpractice.com
Exacerbations of miliaria rubra are often followed by periods of anhidrosis in affected sites.[1]Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998 Jan;38(1):1-17; quiz 18-20.
http://www.ncbi.nlm.nih.gov/pubmed/9448199?tool=bestpractice.com
[2]Sulzberger MB, Harris DR. Miliaria and anhidrosis. 3. Multiple small patches and the effects of different periods of occlusion. Arch Dermatol. 1972 Jun;105(6):845-50.
http://www.ncbi.nlm.nih.gov/pubmed/5030233?tool=bestpractice.com
Miliaria rubra most commonly occurs in hot, humid environments, affecting up to 30% of people exposed to these conditions, and usually affects areas of friction and occlusion.[1]Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998 Jan;38(1):1-17; quiz 18-20.
http://www.ncbi.nlm.nih.gov/pubmed/9448199?tool=bestpractice.com
[14]Lyons RE, Levine R, Auld D. Miliaria rubra, a manifestation of staphylococcal disease. Arch Dermatol. 1962 Sep;86:282-6.
http://www.ncbi.nlm.nih.gov/pubmed/14467655?tool=bestpractice.com
[15]Sanderson PH, Sloper JC. Skin disease in the British army in SE Asia. I. Influence of the environment on skin disease. Br J Dermatol. 1953 Jul-Aug;65(7-8):252-64.
http://www.ncbi.nlm.nih.gov/pubmed/13059235?tool=bestpractice.com
Although formation of miliaria rubra can occur as early as a few days after exposure to a tropical environment, it most commonly occurs after 2 to 5 months of continuous exposure to a hot and humid environment.[1]Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998 Jan;38(1):1-17; quiz 18-20.
http://www.ncbi.nlm.nih.gov/pubmed/9448199?tool=bestpractice.com
[15]Sanderson PH, Sloper JC. Skin disease in the British army in SE Asia. I. Influence of the environment on skin disease. Br J Dermatol. 1953 Jul-Aug;65(7-8):252-64.
http://www.ncbi.nlm.nih.gov/pubmed/13059235?tool=bestpractice.com
Miliaria profunda typically occurs following repeated episodes of miliaria rubra in adults in the tropics and is characterised by asymptomatic lesions that become more prominent when the patient is stimulated to sweat.[1]Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998 Jan;38(1):1-17; quiz 18-20.
http://www.ncbi.nlm.nih.gov/pubmed/9448199?tool=bestpractice.com
In addition, patients are anhidrotic at sites of involvement, with compensatory hyper-hidrosis on the face, hands, and feet, and complain of weakness and dyspnoea from associated heat exhaustion.[1]Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998 Jan;38(1):1-17; quiz 18-20.
http://www.ncbi.nlm.nih.gov/pubmed/9448199?tool=bestpractice.com
[27]O'Brien JP. A study of miliaria rubra, tropical anhidrosis, and anhidrotic asthenia. Br J Dermatol Syph. 1947 Apr-May;59(4-5):125-58.
http://www.ncbi.nlm.nih.gov/pubmed/20242508?tool=bestpractice.com
Physical examination
Miliaria crystallina is characterised by a diffuse eruption, typically on the trunk and proximal extremities, of translucent, fragile, non-follicular vesicles on a non-erythematous base. In neonates, the face and neck may also be involved.[3]Arpey CJ, Nagashima-Whalen LS, Chren MM, et al. Congenital miliaria crystallina: case report and literature review. Pediatr Dermatol. 1992 Sep;9(3):283-7.
http://www.ncbi.nlm.nih.gov/pubmed/1488382?tool=bestpractice.com
[5]Hidano A, Purwoko R, Jitsukawa K. Statistical survey of skin changes in Japanese neonates. Pediatr Dermatol. 1986 Feb;3(2):140-4.
http://www.ncbi.nlm.nih.gov/pubmed/3952030?tool=bestpractice.com
If opened, the vesicles discharge a clear watery liquid. The eruption spontaneously resolves with a superficial branny desquamative appearance.[1]Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998 Jan;38(1):1-17; quiz 18-20.
http://www.ncbi.nlm.nih.gov/pubmed/9448199?tool=bestpractice.com
("Branny" describes the similarity of the appearance to the hard outer layer of cereals.)
Miliaria rubra is characterised by erythematous, non-follicular papules with a central vesicle at sites of friction and occlusion.[1]Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998 Jan;38(1):1-17; quiz 18-20.
http://www.ncbi.nlm.nih.gov/pubmed/9448199?tool=bestpractice.com
[3]Arpey CJ, Nagashima-Whalen LS, Chren MM, et al. Congenital miliaria crystallina: case report and literature review. Pediatr Dermatol. 1992 Sep;9(3):283-7.
http://www.ncbi.nlm.nih.gov/pubmed/1488382?tool=bestpractice.com
In adults, the eruption occurs on the trunk with sparing of the face, while in neonates the face may be involved.[1]Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998 Jan;38(1):1-17; quiz 18-20.
http://www.ncbi.nlm.nih.gov/pubmed/9448199?tool=bestpractice.com
[3]Arpey CJ, Nagashima-Whalen LS, Chren MM, et al. Congenital miliaria crystallina: case report and literature review. Pediatr Dermatol. 1992 Sep;9(3):283-7.
http://www.ncbi.nlm.nih.gov/pubmed/1488382?tool=bestpractice.com
[5]Hidano A, Purwoko R, Jitsukawa K. Statistical survey of skin changes in Japanese neonates. Pediatr Dermatol. 1986 Feb;3(2):140-4.
http://www.ncbi.nlm.nih.gov/pubmed/3952030?tool=bestpractice.com
Non-follicular pustules can also form and, if widespread, the condition is termed miliaria pustulosa.[1]Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998 Jan;38(1):1-17; quiz 18-20.
http://www.ncbi.nlm.nih.gov/pubmed/9448199?tool=bestpractice.com
Anhidrosis may occur in affected sites.[1]Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998 Jan;38(1):1-17; quiz 18-20.
http://www.ncbi.nlm.nih.gov/pubmed/9448199?tool=bestpractice.com
Miliaria profunda is characterised by flesh-coloured, non-folliculocentric, deep-seated papules concentrated on the trunk and proximal extremities with associated anhidrosis of affected areas.[1]Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998 Jan;38(1):1-17; quiz 18-20.
http://www.ncbi.nlm.nih.gov/pubmed/9448199?tool=bestpractice.com
Other findings include compensatory hyper-hidrosis of the face, axillae, hands, and feet as well as inguinal and axillary adenopathy.[1]Wenzel FG, Horn TD. Nonneoplastic disorders of the eccrine glands. J Am Acad Dermatol. 1998 Jan;38(1):1-17; quiz 18-20.
http://www.ncbi.nlm.nih.gov/pubmed/9448199?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Miliaria crystallina in hospitalised febrile patientFrom Brian L. Swick's collection, used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Miliaria rubraFrom Brian L. Swick's collection, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Miliaria rubraFrom Brian L. Swick's collection, used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Non-inflammatory fragile fluid filled blisters of miliaria crystallinaFrom Brian L. Swick's collection, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Non-inflammatory fragile fluid filled blisters of miliaria crystallinaFrom Brian L. Swick's collection, used with permission [Citation ends].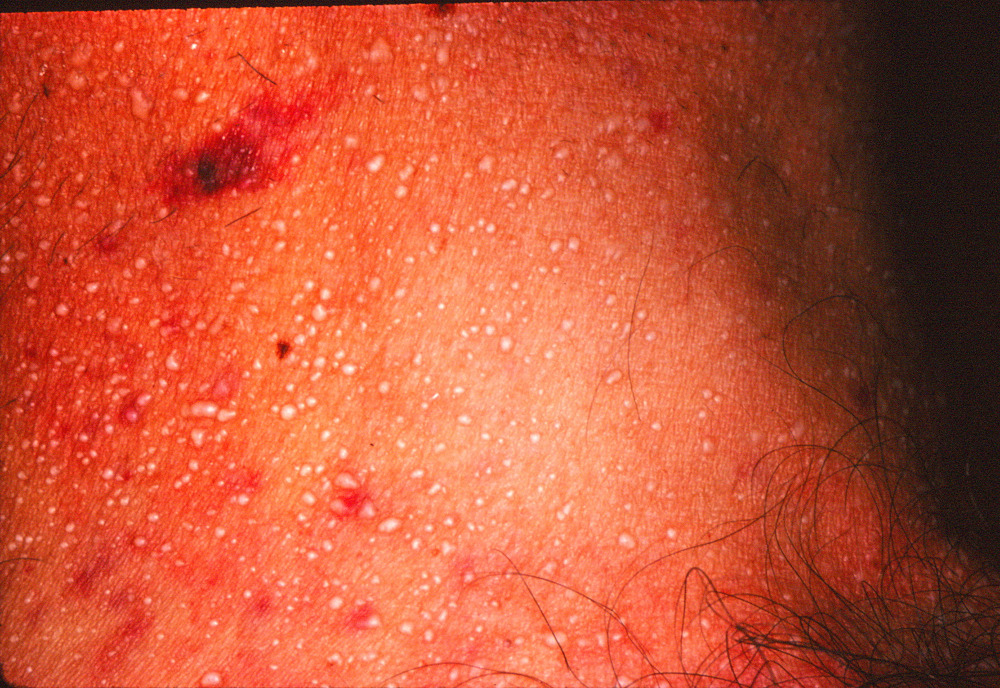 [Figure caption and citation for the preceding image starts]: Small tightly grouped inflammatory papules of miliaria rubraFrom Brian L. Swick's collection, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Small tightly grouped inflammatory papules of miliaria rubraFrom Brian L. Swick's collection, used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Deep inflammatory papules of miliaria profundaFrom Brian L. Swick's collection, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Deep inflammatory papules of miliaria profundaFrom Brian L. Swick's collection, used with permission [Citation ends].
Laboratory evaluation
Laboratory testing is typically not required as the diagnosis is usually made by historical and physical examination findings. However, a skin biopsy of an active lesion may be required for confirmation if the clinical presentation is less distinctive.
Haematoxylin- and eosin-stained sections from a lesion of miliaria crystallina demonstrate a sub-corneal vesicle situated over an acrosyringeal duct with no associated inflammatory infiltrate.
Haematoxylin- and eosin-stained sections from a lesion of miliaria rubra demonstrate spongiosis of an intra-epidermal sweat duct, sometimes forming a spongiotic vesicle, with lymphocytic exocytosis and a superficial perivascular infiltrate of lymphocytes and neutrophils.
Haematoxylin- and eosin-stained sections from a lesion of miliaria profunda demonstrates an intra-epidermal spongiotic vesicle associated with an acrosyringeal duct with lymphocytic exocytosis, and a superficial perivascular infiltrate of lymphocytes and neutrophils that is denser than that seen in miliaria rubra.
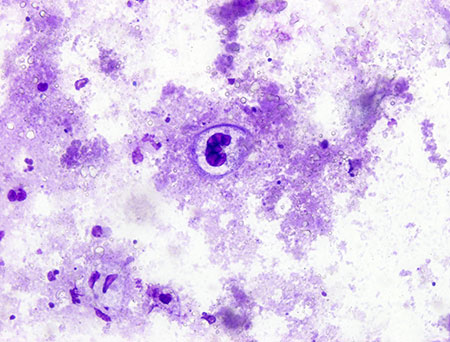
Herpetic infections can be ruled out using a Tzanck smear, viral direct fluorescent antibody, culture, or viral polymerase chain reaction (PCR). Staphylococcal infection can be ruled out with bacterial culture, and candidiasis infection can be ruled out using either a fungal culture or a potassium hydroxide (KOH) preparation.[Figure caption and citation for the preceding image starts]: Micrograph demonstrates the presence of herpes simplex virus in a Tzanck smearFrom Brian L. Swick's collection, used with permission [Citation ends].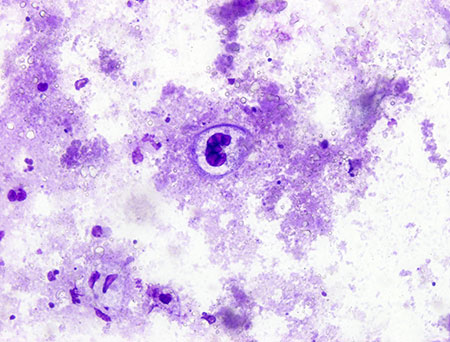
 [Figure caption and citation for the preceding image starts]: Miliaria rubraFrom Brian L. Swick's collection, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Miliaria rubraFrom Brian L. Swick's collection, used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Non-inflammatory fragile fluid filled blisters of miliaria crystallinaFrom Brian L. Swick's collection, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Non-inflammatory fragile fluid filled blisters of miliaria crystallinaFrom Brian L. Swick's collection, used with permission [Citation ends].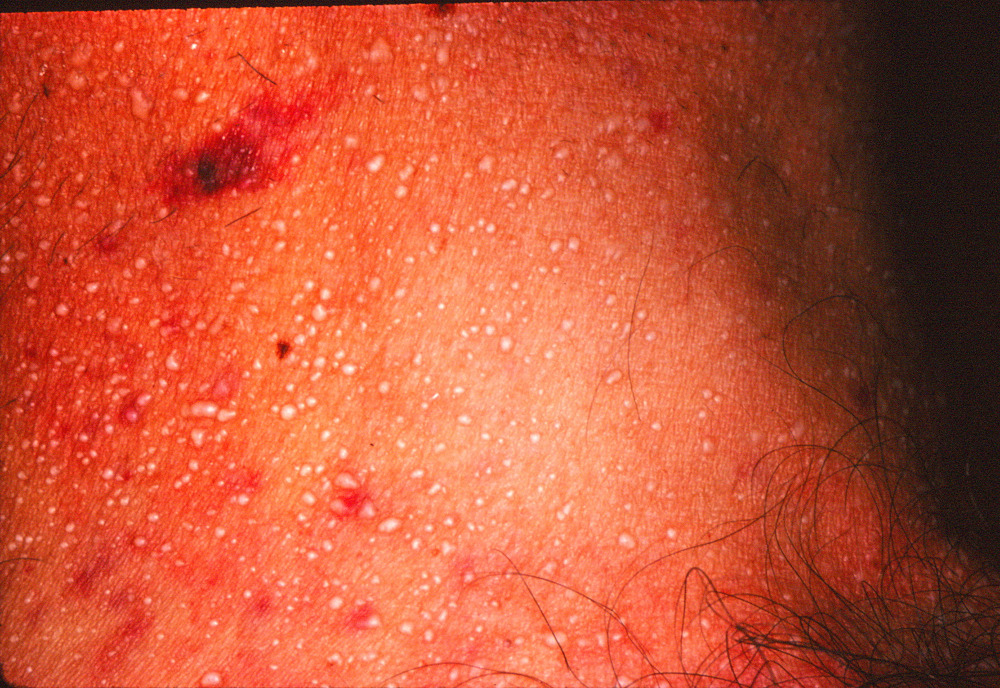 [Figure caption and citation for the preceding image starts]: Small tightly grouped inflammatory papules of miliaria rubraFrom Brian L. Swick's collection, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Small tightly grouped inflammatory papules of miliaria rubraFrom Brian L. Swick's collection, used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Deep inflammatory papules of miliaria profundaFrom Brian L. Swick's collection, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Deep inflammatory papules of miliaria profundaFrom Brian L. Swick's collection, used with permission [Citation ends].