Investigations
Investigations to consider
Tzanck smear
Test
As miliaria crystallina produces clear fluid-filled vesicles, similar to a herpetic eruption, performance of a Tzanck smear may aid in ruling out a herpetic infection.
The clinician opens a vesicle, scrapes the base of the vesicle with a number 15 blade, and evenly smears the fluid onto a microscope slide. The smear is then stained with Giemsa and viewed under the microscope. Multi-nucleated giant cells are indicative of a herpetic viral infection. These would be absent in miliaria. While eosinophils are seen in erythema toxicum neonatorum and neutrophils are seen in transient neonatal pustular melanosis. These cells would not be seen in miliaria.
The sensitivity of the Tzanck smear in the diagnosis of cutaneous herpetic infection is 79% while the specificity is 93%.[28] However, despite the accuracy of the test, identification of multi-nucleated giant cells takes practice. In addition, it is non-specific as herpes simplex virus (HSV) and varicella-zoster virus (VZV) infection produce multi-nucleated giant cells.
[Figure caption and citation for the preceding image starts]: Micrograph demonstrates the presence of herpes simplex virus in a Tzanck smearFrom Brian L. Swick's collection, used with permission [Citation ends].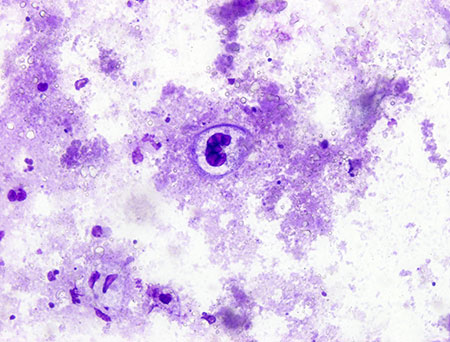
Result
normal in miliaria; rules out herpetic infection, erythema toxicum neonatorum, and neonatal pustular melanosis
viral direct fluorescent antibody (DFA) or culture
Test
As miliaria crystallina produces clear fluid-filled vesicles, similar to a herpetic eruption, performance of a viral DFA/culture may aid in ruling out a herpetic infection.
The clinician opens a vesicle, swabs the base of the vesicle and sends the swab to the laboratory.
The DFA test will differentiate HSV from VZV and results are usually available within hours. DFA sensitivity and specificity are 74% and 85%, respectively.[29]
Viral culture results take longer to receive (48 to 72 hours) and cannot differentiate HSV from VZV infection. However, the test is more sensitive than viral DFA.
Result
normal in miliaria; rules out herpetic infection
viral polymerase chain reaction
Test
As miliaria crystallina produces clear fluid-filled vesicles, similar to a herpetic eruption, performance of a viral polymerase chain reaction (PCR) may aid in ruling out a herpetic infection.
The clinician opens a vesicle, swabs the base of the vesicle, and sends the swab to the laboratory.
PCR sensitivity is at least as good as viral culture and can differentiate HSV from VZV infection. Results are typically available within hours.[30]
Result
normal in miliaria; rules out herpetic infection
bacterial culture
Test
As miliaria crystallina produces fragile vesicles similar to impetigo, performance of a bacterial culture may aid in ruling out impetigo.
Result
normal in miliaria; rules out Staphylococcus aureus infection
fungal culture
Test
Performance of a fungal culture can aid in ruling out candidiasis. This is especially important in distinguishing congenital cutaneous candidiasis from miliaria rubra.
Result
normal in miliaria; rules out candidiasis
potassium hydroxide (KOH) preparation
Test
Performance of a KOH preparation can aid in ruling out candidiasis by visualising budding yeast and pseudohyphae. This is especially important in distinguishing congenital cutaneous candidiasis from miliaria rubra.
Result
normal in miliaria; rules out candidiasis
skin biopsy
Test
Punch biopsy of a vesicle or papule can confirm the diagnosis and rule out other dermatoses with a similar appearance.
Haematoxylin- and eosin-stained sections from a lesion of miliaria crystallina demonstrates a sub-corneal vesicle situated over an acrosyringeal duct with no associated inflammatory infiltrate.
Haematoxylin- and eosin-stained sections from a lesion of miliaria rubra demonstrates spongiosis of an intra-epidermal sweat duct, sometimes forming a spongiotic vesicle, with lymphocytic exocytosis and a superficial perivascular infiltrate of lymphocytes and neutrophils.
Haematoxylin- and eosin-stained sections from a lesion of miliaria profunda demonstrates an intra-epidermal spongiotic vesicle associated with an acrosyringeal duct with lymphocytic exocytosis, and a superficial perivascular infiltrate of lymphocytes and neutrophils that is denser than that seen in miliaria rubra.[Figure caption and citation for the preceding image starts]: Photomicrograph of miliaria crystallina showing non-inflammatory sub-corneal blister (H&Ex100)From Brian L. Swick's collection, used with permission [Citation ends].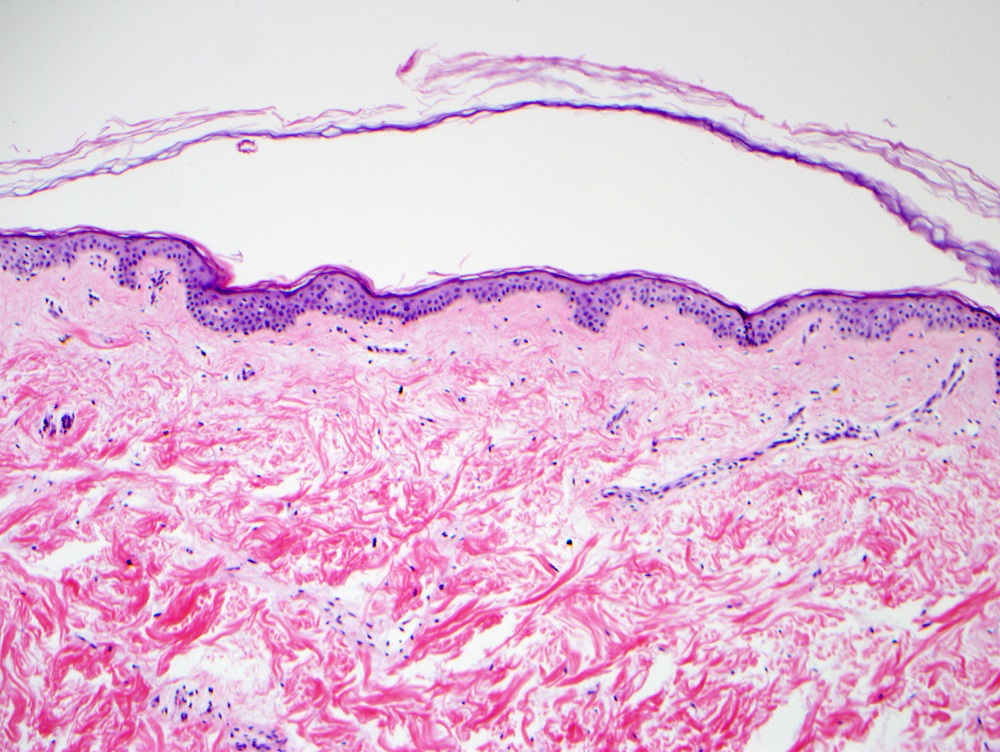 [Figure caption and citation for the preceding image starts]: Photomicrograph of miliaria rubra showing intra-epidermal acrosyringeal spongiosis and underlying chronic inflammation (H&Ex400)From Brian L. Swick's collection, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Photomicrograph of miliaria rubra showing intra-epidermal acrosyringeal spongiosis and underlying chronic inflammation (H&Ex400)From Brian L. Swick's collection, used with permission [Citation ends].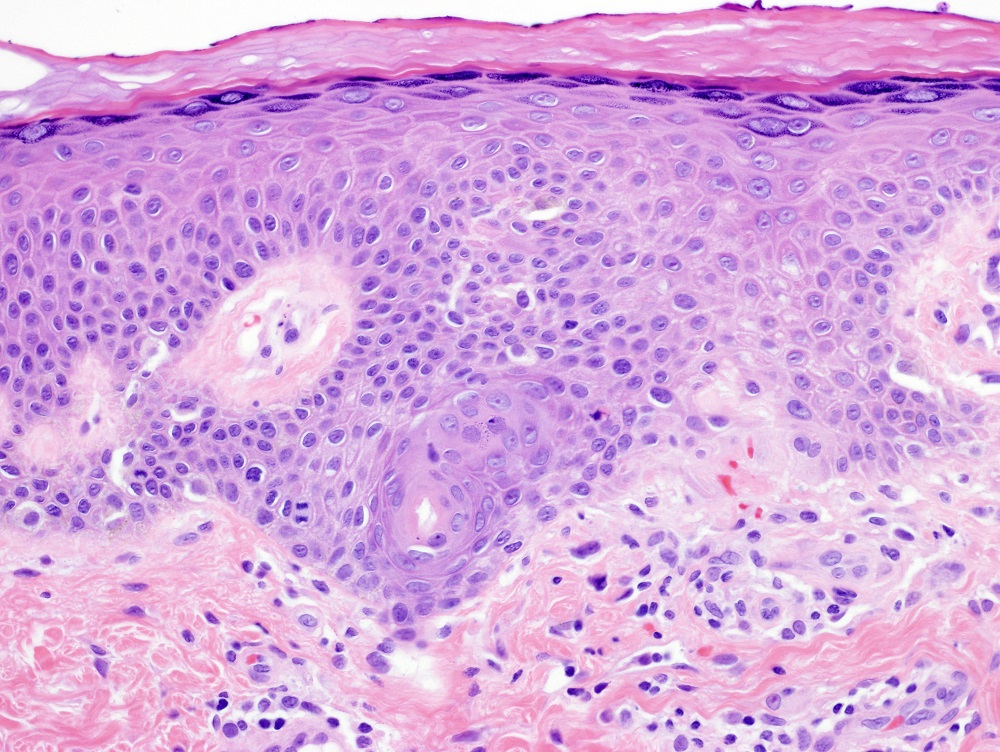 [Figure caption and citation for the preceding image starts]: Photomicrograph of miliaria profunda showing chronic inflammation centred on an eccrine duct in the dermis (H&Ex40)From Brian L. Swick's collection, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Photomicrograph of miliaria profunda showing chronic inflammation centred on an eccrine duct in the dermis (H&Ex40)From Brian L. Swick's collection, used with permission [Citation ends].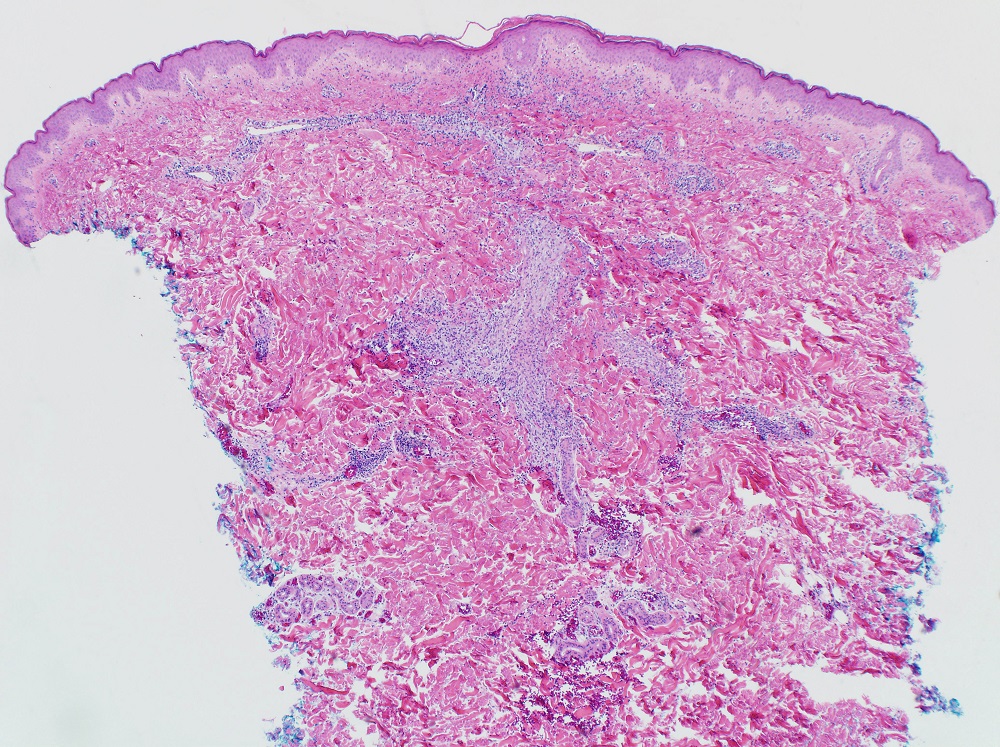
Result
sub-corneal vesicle situated over an acrosyringeal duct with no associated inflammatory infiltrate (miliaria crystallina); spongiosis of an intra-epidermal sweat duct (miliaria rubra); intra-epidermal spongiotic vesicle associated with an acrosyringeal duct with lymphocytic exocytosis (miliaria profunda)
Use of this content is subject to our disclaimer